Abstract
We investigated molecular epidemiology of methicillin-resistant Staphylococcus aureus (MRSA) isolated at 10 intensive care units (ICUs) in Korea. MRSA isolates from bacteremia and nasal colonization were collected prospectively from October 2008 through May 2009 at 10 University-affiliated hospital ICUs. A total of 83 and 175 MRSA strains were isolated from bacteremia and nasal colonization, respectively. Acquired group accounted for 69.9% (n = 58) of bacteremia and 73.1% (n = 128) of nasal colonization. Pulsed-field gel electrophoresis (PFGE) type B (SCCmec type II/ST5) was dominant in the acquired group followed by PFGE type D (SCCmec type IVA/ST72; a community genotype). Seven of 58 (12.1%) acquired bacteremia and 15 of 128 (11.8%) acquired nasal colonizations had SCCmec type IVA/ST72 genotype, which indicated that the community genotype had already emerged as a cause of ICU acquired MRSA infection or colonization. Antibiotic resistance rates to ciprofloxacin, tetracycline, clindamycin and trimethoprim/ sulfamethoxazole were 84.4%, 67.1%, 78.1%, and 12.0%, respectively. Susceptibility to ciprofloxacin best predicted a community genotype (sensitivity 96.5%; specificity 96.9%; odds ratio 861; 95% confidence interval 169-4,390, P < 0.001) and the positive predictive value was 90.2%. Among 23 nasal re-colonized strains, 7 MRSA strains (30.4%) were different from the originally colonized strains on the basis of PFGE types.
Staphylococcus aureus is a major cause of serious infections in both hospitals and the community and the increasing rates of MRSA infection is now a health problem worldwide (1). The frequency of MRSA from tertiary hospitals in Korea was reported to account for 60%-70% of all S. aureus isolates (2) and MRSA is more prevalent in ICU setting than non-ICU setting among inpatients (3). Bacteremia was three times more common in S. aureus nasal carriers than non-carriers (4), and MRSA nasal carriage increased MRSA infections at ICUs (5, 6). From this point of view, understanding the molecular epidemiology of MRSA from bacteremia and nasal carriage may be useful for understanding the source and transmission of MRSA in ICU settings.
The most commonly used typing techniques for S. aureus are pulsed field gel electrophoresis (PFGE), multilocus sequence typing (MLST), Staphylococcus protein A (spa) typing, and staphylococcal cassette chromosome mec (SCCmec) typing. PFGE is considered the best method to investigate MRSA outbreaks in hospitals, as well as hospital-to hospital transmission of MRSA but is a time-consuming process (7). Therefore, genotyping is not a routine test in daily clinical practice. Recently, there was a report that specific genotype could be predicted by antibiotic susceptibility in bloodstream MRSA infections (8). Whether this phenotypic rule could be applied to MRSA isolates other than bacteremia or from other geographic regions in a similar manner is left to question.
The aims of this study were to analyze the molecular epidemiology of MRSA isolates from bacteremia and nasal colonization and to find out the relationship between phenotype and genotype of MRSA isolates from ICUs in Korea.
This study was a prospective multicenter surveillance of bacteremia and nasal carriage of MRSA at 10 university-affiliated hospital ICUs in Korea from October 2008 through May 2009. The participating institutions included Bucheon St. Mary's Hospital, Kyunghee University Medical Center, Soonchunhyang University Bucheon Hospital, Daejeon St. Mary's Hospital, Hallym University Kangnam Sacred Heart Hospital, Hanyang University Seoul Hospital, Ilsan Hospital, Korea University Guro Hospital, Incheon St. Mary's Hospital and Yeouido St. Mary's Hospital. Cases of MRSA bacteremia were collected from all participating hospitals, but cases of nasal carriage of MRSA only from the first 3 hospitals.
All patients were older than 15 yr. In case of nasal carriers, patients without MRSA infection and expected to stay more than 48 hr at ICU were included and patients already infected with MRSA or planned to be discharged from ICU within 48 hr were excluded.
The following data were collected from all cases; demographic information, underlying diseases, comorbid conditions, previous medical and surgical history, microbiological data, sources of infections, presence of indwelling catheters, and other important clinical parameters at the time of infection. Health care-associated risk factors included history of MRSA infection or colonization, use of antibiotics or steroid, dialysis, the presence of an invasive device (e.g. vascular catheter, urinary catheter, gastric feeding tube, or tracheostomy tube), and a history of hospitalization, surgery, long-term care facility within one year prior to the MRSA culture date.
MRSA bacteremia was defined as isolation of MRSA from at least 2 separate blood cultures within 24 hr or 1 blood culture with clinical significance. Only the first isolate was included when multiple positive cultures were obtained from one patient.
Nasal carriage was defined as the presence of MRSA in a nasal swab culture. Eradication was defined as the clearance of MRSA in the following 3 consecutive nasal swab cultures after decolonization. Recolonization was defined as the first presence of MRSA in a nasal swab culture following successful eradication.
Each case of MRSA bacteremia or nasal colonization was classified as either 'imported' or 'acquired' depending on the hours from the date of ICU admission to the date of culture-positive specimens. Imported bacteremia or colonization was defined as a positive culture sample obtained within 72 hr after ICU admission and acquired bacteremia or colonization was defined as a positive culture sample obtained on or later than 72 hr after ICU admission (9).
For all study patients, nasal swabs were taken for surveillance cultures of MRSA. Surveillance cultures were performed weekly starting the admission date until ICU discharge. Nasal swab specimens were transported in Amie's medium (Micromedia Co., Seoul, Korea) and were streaked directly on sheep blood agar plate (D-BAP) (Asan Medical Co., Seoul, Korea), incubated at 35℃, and examined at 24 and 48 hr. Suspicious colonies were identified as S. aureus by catalase production, positive clumping test, or positive tube coagulase test. MRSA was confirmed by cefoxitin disk diffusion susceptibility testing according to clinical and laboratory standards institute (CLSI) guidelines (13). All isolates identified from each hospital were transported to the Catholic Research Institutes of Medical Science for molecular typing.
In case of MRSA nasal carriers, decolonization was preformed with mupirocin intranasally once daily for 5 days and daily chlorhexidine gluconate bathing for 3 days. Patients with MRSA colonization or infection were placed in contact isolation in single rooms or if a single room was not available, cohorting was acceptable. A clinical warning was entered into the electronic medical record and the patient's bedside identifying the patient as positive for MRSA. The use of gloves and masks was required for all contacts with a patient in contact isolation. Putting on goggles was recommended, if necessary. The patient's care was provided by the smallest possible regular team with doctors and nurses. Contact with other healthcare workers and visitors was kept to a minimum. Hand-hygiene was emphasized again before and after contact with these patients.
Identification of MRSA and antimicrobial susceptibility tests were performed on the Vitek II automated system with GP cards and AST-P601 cards (bioMérieux, Hazelwood, MO, USA), respectively, or MicroScan Pos Combo Panel Type 6 automated system with combination PBC28 cards (Baxter Diagnostics, West Sacramento, CA, USA).
Molecular typing of all MRSA isolates was performed using PFGE, MLST, and spa typing method as described elsewhere (14-18). The spa complex was defined by visual analysis, in which spa types with similar short sequence repeats were clustered into complexes, as described by Ruppitsch et al. (16) and Park et al. (10). The SCCmec types were determined by multiplex PCR, as described by Oliveira et al. (19). Nontypeable strains were defined as strains that showed unexpected fragments or that lacked some fragments in multiplex PCR and thus did not correspond to previously defined SCCmec types.
Data analysis was performed using SPSS software, version 12.0K. Statistical significance was assessed via the chi-squared test or the Fisher exact test for categorical variables and the Student t-test or the Mann-Whitney U-test for continuous variables. P values of less than 0.05 were considered to be statistically significant.
A total of 281 MRSA strains were isolated from 258 patients. Cases of bacteremia, nasal colonization and nasal re-colonization consisted of 83, 175 and 23 strains, respectively.
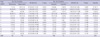
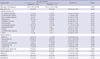
In bacteremia group, acquired infection accounted for 69.9% (n = 58). Age, sex, underlying diseases and sources of bacteremia were not different between the acquired and imported groups. Previous hospitalization and stay in long-term care facility were more frequent in the imported group, but only the latter showed significant difference. History of MRSA infections, recent antibiotic use, and presence of central venous catheter or indwelling urinary catheter were significantly higher in the acquired group (Table 1). In nasal carriage group, acquired group accounted for 73.1% (n = 128). Underlying malignancies were more frequent in the imported group. Previous antimicrobial use and presence of indwelling urinary catheter were significantly higher in the acquired group (Table 2). Among 258 cases with bacteremia or nasal colonization, all acquired cases had at least one healthcare-associated risk factors and in the imported cases, 2 cases of bacteremia and 6 cases of nasal colonization did not have any healthcare-associated risk factors.
Results from molecular typing of MRSA isolates by PFGE, MLST, spa typing and SCCmec typing are summarized in Table 3. One-hundred sixty three MRSA isolates of PFGE type A, B, C, G, K, M, and O shared the same MLST profile (ST5) and spa complex A and carried SCCmec II or II variant. All 58 isolates of PFGE type D shared ST72 and spa complex B and carried SCCmec type IVA. Of 258 isolates, 223 (88.8%) clustered into 4 major PFGE types (designated A, B, D, and E). The number of PFGE types was 11 in bacteremia and 13 in nasal colonization. Among 258 isolates, excluding nasal re-colonization, the most frequent PFGE type was type B (n = 120, 46.5%), and the second was type D (n = 58, 22.5%). There was no difference in the distribution of PFGE type B and D between bacteremia and nasal colonization. PFGE patterns were similar except for type A. PFGE type A was detected in 11.4% of nasal colonization, which is significantly higher than 1.2% of bacteremia (Table 4). Acquired group consisted of 13 PFGE types, and type B accounted for 55.9% followed by type D and E, each of which comprised 11.8%. On the other hand, imported group consisted of 11 PFGE types, and type D accounted for 50.0% followed by type B (22.2%). PFGE type B and E were significantly higher in the acquired group and type D in the imported group (Table 4).
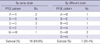
Results of antibiotic susceptibility were not available in 2 of bacteremia and 5 of nasal colonization. Tetracycline (TC) susceptibility was reported in only 225 out of 258 isolates. Of all MRSA isolates, each antibiotic susceptibility rate to ciprofloxacin (CPX), TC, clindamycin (CDM) and trimethoprim/sulfamethoxazole (TMP/SMX) was 24.3%, 32.9%, 21.9%, and 88.0%, respectively. Among MRSA isolates with PFGE type B, susceptibility rates were 0.8%, 4.8%, 0.8% and 93.2%, in contrast to the 96.5%, 96.0%, 86.0% and 100% found among MRSA isolates with PFGE type D. We found that susceptibility to CPX (sensitivity 96.5%; specificity 96.9%; odds ratio 861; 95% confidence interval [CI] 169-4,390, P < 0.001) best predicted a community genotype, i.e., PFGE type D (SCCmec type IVA/ST72). The positive predictive value (PPV) for identifying a PFGE type D was 90.2% (Table 5). The PPV of CPX susceptibility was the highest when analyzing bacteremia and nasal colonization separately (85.7% and 92.5%, respectively).
Nasal recolonization of MRSA was identified in 23 cases. Among these cases, 7 (30.4%) MRSA strains were different from the originally colonized ones on the basis of PFGE types (Table 6). Mean duration of ICU stay was significantly longer in the recolonizers than non-recolonizers (37.6 days vs 21.9 days, P = 0.031).
This study investigated the molecular epidemiology and the relationship between antibiotic susceptibility pattern and PFGE types of MRSA strains isolated from ICU patients with bacteremia and nasal colonization.
The PFGE patterns of MRSA were diverse in several studies. A few genotypes were dominant in some studies (20, 21), but not so in others (22, 23). Overall, 13 genotypes were identified with 2 major types. PFGE type B and D counted for 69.0% and in combination with type A and E, 4 PFGE types counted for more than 85%. Although the number of PFGE types in bacteremia and nasal colonization was 11 and 13, PFGE types B and D accounted for 78.3% and 64.6%, respectively and most types had less than 7 isolates (Table 4). PFGE type B in the acquired group and type D in the imported group comprised more than 50% for each group (Table 4). PFGE type B was the second most common PFGE type in the imported group, resulting in an interesting contrast with the acquired group. Considering PFGE type B is SCCmec type II/ST5 genotype representing hospital genotype (HG) and type D is SCCmec type IVA/ST72 genotype representing community genotype (CG) epidemiologically in Korea (10, 12, 24), these findings suggest CG is dominant in the imported group. In addition, it is noticeable that CG (SCCmec type IVA/ST72) accounted for about 11.8% in the acquired group. Nosocomial MRSA infection by CG has increased recently and community-associated MRSA strains are emerging as major causes of bloodstream infections in healthcare settings in Korea (10). These findings are consistent with our results. Considering CG was prevalent in patients with history of hospitalization or long term care facility admission, there is a concern that classification between CG and HG genotype could prove to be ambiguous in the future. In fact, among 258 isolates of bacteremia or nasal colonization, all but 8 cases had at least one healthcare-associated risk factors.
Lee et al. investigated the antimicrobial susceptibilities of 90 MRSA clinical isolates at a tertiary hospital in Korea (25). The resistance rate to CPX, TC, and CDM was 96.7%, 96.7%, and 86.7%, respectively. Various clinical specimens (e.g. pus, sputum, blood, sputum, etc.) were included in this study and the resistance rate to TMP/SMX was not reported. In another study in Korea, 36 MRSA isolates were obtained from blood consecutively for 5 months at a tertiary hospital, and the antibiotic resistance rate to CPX, TC, CDM and TMP/SMX was 83.3%, 72.2%, 83.3%, and 8.3%, respectively (26). Similarly in our study, the antibiotic resistance rate to CPX, TC, CDM and TMP/SMX in the bacteremia group was 72.8%, 70.4%, 80.2%, and 7.4%, respectively.
Popovich et al. (8) assessed the performance characteristics of a rule using the antimicrobial phenotype to predict genotype from 147 MRSA bloodstream isolates in a tertiary hospital. USA-300 and USA-400 were classified as CG; USA-100, USA-500, and USA-800 were labeled HG. A CG was seen in 86 isolates. Susceptibility to CDM (sensitivity, 95%; specificity, 80%; likelihood ratio, 4.86; 95% CI, 3.29 to 6.47) or fluoroquinolones (sensitivity, 73%; specificity, 86%; likelihood ratio, 5.34; 95% CI, 2.91 to 10.58) best predicted a CG (8). We applied this rule to both bacteremia and nasal carrier isolates. Of all isolates, susceptibility to CPX was best for predicting a CG (SCCmec type IVA/ST72) (sensitivity, 96.5%; specificity, 96.9%; odds ratio, 861; 95% CI, 169-4390, P < 0.001) and the PPV was 90.2%. In a separate analysis for each group, CPX susceptibility was the best predictive rule. This means that certain phenotype can be used to predict specific genotype, and it is useful when genotype test is not available or while waiting for genotypic results. However, because the epidemiology of phenotype and genotype are not constantly maintained in a certain geographic region or hospital, periodic re-evaluation and accumulation of data are essential to apply temporally appropriate phenotypic rule (10, 23, 27). Huang et al. (23) studied changing molecular epidemiology of MRSA bloodstream isolates collected from a teaching hospital over a 4-yr interval. PFGE type A accounted for 78.2% (97/124) during 2000 to 2001, but decreased to 30.6% (38/124) during 2004 to 2005. However, PFGE type B, D, F, and AH increased from less than 3% (0.0%-2.4%) to more than 10% (10.5%-12.1%), while type D did not change during the same period. In Korea, Park et al. (10) reported CG (SCCmec type IVA) MRSA bloodstream infections increased more than the past among patients with healthcare-associated risk factors.
Corbella et al. (28) studied the relationship between S. aureus nasal carriage and subsequent staphylococcal infection. They reported one nasal carrier initially colonized by methicillin susceptible S. aureus (MSSA) was recolonized by MRSA. In our study, 23 cases were recolonized by MRSA in subsequent surveillance nasal cultures after successful eradication. Among them, 7 (30.4%) MRSA strains were different from the originally colonized strains on the basis of PFGE types. The longer duration of ICU stay in the recolonizers (37.6 days vs 21.9 days, P = 0.031) may contribute to reacquiring nasal MRSA. Healthcare workers such as doctors or nurses, visitors and other patients could be potential sources of subsequent repetitive MRSA carriage. Cross-contamination through transient colonization of the hands of healthcare personnel is a common route of patient-to-patient transmission of MRSA (29). However, further research will be needed to identify their origin.
This study has several limitations. Although MRSA isolates were collected prospectively, some of them were missed. Also, cases of nasal carriage of MRSA were collected from only 3 hospitals compared with those of bacteremia, which were collected from 10 hospitals. But all collected strains were carried to the central laboratory for molecular analysis. Second, because this study was not designed to investigate the direct relationship between nasal carrier and subsequent bacteremia, no temporal and spatial interpretation between these 2 groups could be inferred. Third, although the antibiotic predictive rule can help to make an estimation of molecular epidemiology, objective data on which the predictive rule is based may change with time, resulting in limited clinical decision making applicability.
In conclusion, PFGE patterns of MRSA at tertiary hospital ICUs in Korea are diverse, but a small number of clones form more than 85%. Community strains and hospital strains have been already mixed up in Korean ICUs. CPX susceptibility could be a useful tool for predicting SCCmec type IVA/ST72, the CG in Korea. About one third of nasal MRSA recolonizations in ICUs are new strains on the basis of PFGE types.
Figures and Tables
Table 4
Comparison of PFGE pattern of MRSA between bacteremia and nasal carrier and between acquired and imported groups
ACKNOWLEDGMENTS
We thank all the staffs and associated workers from each hospital for help in data collections.
Notes
AUTHOR SUMMARY
Molecular Epidemiologic Analysis of Methicillin-Resistant Staphylococcus aureus Isolates from Bacteremia and Nasal Colonization at 10 Intensive Care Units: Multicenter Prospective Study in Korea
Jae-Cheol Kwon, Si-Hyun Kim, Sun Hee Park, Su-Mi Choi, Dong-Gun Lee, Jung-Hyun Choi, Chulmin Park, Na-Young Shin, and Jin-Hong Yoo
Staphylococcus aureus is a major cause of serious infections in both hospitals and the community. Increasing rates of methicillin-resistant Staphylococcus aureus (MRSA) infection is now a worldwide health problem. We investigated molecular epidemiology of MRSA isolates from blood and nasal secretion at 10 University-affiliated hospital ICUs (from October 2008 to May 2009). Pulsed-field gel electrophoresis (PFGE) patterns were diverse; PFGE type B was dominant in the ICU-acquired group and PFGE type D in the ICU-imported group. PFGE type D, which represents community genotype epidemiologically in Korea, accounted for more than 10% in the ICU-acquired group. This suggests that community strains and hospital strains have been already mixed up in Korean ICUs. Among MRSA isolates with PFGE type D, susceptibility rate to ciprofloxacin was 96.5%. The susceptibility to ciprofloxacin best predicted a community genotype, i.e., PFGE type D.
References
1. Tacconelli E. Methicillin-resistant Staphylococcus aureus: source control and surveillance organization. Clin Microbiol Infect. 2009. 15:Suppl 7. 31–38.
2. Chong Y, Lee K. Present situation of antimicrobial resistance in Korea. J Infect Chemother. 2000. 6:189–195.
3. Sista RR, Oda G, Barr J. Methicillin-resistant Staphylococcus aureus infections in ICU patients. Anesthesiol Clin North America. 2004. 22:405–435.
4. Wertheim HF, Vos MC, Ott A, van Belkum A, Voss A, Kluytmans JA, van Keulen PH, Vandenbroucke-Grauls CM, Meester MH, Verbrugh HA. Risk and outcome of nosocomial Staphylococcus aureus bacteraemia in nasal carriers versus non-carriers. Lancet. 2004. 364:703–705.
5. Garrouste-Orgeas M, Timsit JF, Kallel H, Ben Ali A, Dumay MF, Paoli B, Misset B, Carlet J. Colonization with methicillin-resistant Staphylococcus aureus in ICU patients: morbidity, mortality, and glycopeptide use. Infect Control Hosp Epidemiol. 2001. 22:687–692.
6. Honda H, Krauss MJ, Coopersmith CM, Kollef MH, Richmond AM, Fraser VJ, Warren DK. Staphylococcus aureus nasal colonization and subsequent infection in intensive care unit patients: does methicillin resistance matter? Infect Control Hosp Epidemiol. 2010. 31:584–591.
7. Deurenberg RH, Stobberingh EE. The evolution of Staphylococcus aureus. Infect Genet Evol. 2008. 8:747–763.
8. Popovich K, Hota B, Rice T, Aroutcheva A, Weinstein RA. Phenotypic prediction rule for community-associated methicillin-resistant Staphylococcus aureus. J Clin Microbiol. 2007. 45:2293–2295.
9. Tomic V, Svetina Sorli P, Trinkaus D, Sorli J, Widmer AF, Trampuz A. Comprehensive strategy to prevent nosocomial spread of methicillin-resistant Staphylococcus aureus in a highly endemic setting. Arch Intern Med. 2004. 164:2038–2043.
10. Park SH, Park C, Yoo JH, Choi SM, Choi JH, Shin HH, Lee DG, Lee S, Kim J, Choi SE, Kwon YM, Shin WS. Emergence of community-associated methicillin-resistant Staphylococcus aureus strains as a cause of healthcare-associated bloodstream infections in Korea. Infect Control Hosp Epidemiol. 2009. 30:146–155.
11. Bae IG, Kim JS, Kim S, Heo ST, Chang C, Lee EY. Genetic correlation of community-associated methicillin-resistant Staphylococcus aureus strains from carriers and from patients with clinical infection in one region of Korea. J Korean Med Sci. 2010. 25:197–202.
12. Park C, Lee DG, Kim SW, Choi SM, Park SH, Chun HS, Choi JH, Yoo JH, Shin WS, Kang JH, Kim JH, Lee SY, Kim SM, Pyun BY. Predominance of community-associated methicillin-resistant Staphylococcus aureus strains carrying staphylococcal chromosome cassette mec type IVA in South Korea. J Clin Microbiol. 2007. 45:4021–4026.
13. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing: 17th informational supplement. 2007. Wayne, PA: Clinical and Laboratory Standards Institute.
14. McDougal LK, Steward CD, Killgore GE, Chaitram JM, McAllister SK, Tenover FC. Pulsed-field gel electrophoresis typing of oxacillin-resistant Staphylococcus aureus isolates from the United States: establishing a national database. J Clin Microbiol. 2003. 41:5113–5120.
15. Shopsin B, Gomez M, Montgomery SO, Smith DH, Waddington M, Dodge DE, Bost DA, Riehman M, Naidich S, Kreiswirth BN. Evaluation of protein A gene polymorphic region DNA sequencing for typing of Staphylococcus aureus strains. J Clin Microbiol. 1999. 37:3556–3563.
16. Ruppitsch W, Indra A, Stöger A, Mayer B, Stadlbauer S, Wewalka G, Allerberger F. Classifying spa types in complexes improves interpretation of typing results for methicillin-resistant Staphylococcus aureus. J Clin Microbiol. 2006. 44:2442–2448.
17. Enright MC, Day NP, Davies CE, Peacock SJ, Spratt BG. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. J Clin Microbiol. 2000. 38:1008–1015.
18. Murchan S, Kaufmann ME, Deplano A, de Ryck R, Struelens M, Zinn CE, Fussing V, Salmenlinna S, Vuopio-Varkila J, El Solh N, Cuny C, Witte W, Tassios PT, Legakis N, van Leeuwen W, van Belkum A, Vindel A, Laconcha I, Garaizar J, Haeggman S, Olsson-Liljequist B, Ransjo U, Coombes G, Cookson B. Harmonization of pulsed-field gel electrophoresis protocols for epidemiological typing of strains of methicillin-resistant Staphylococcus aureus: a single approach developed by consensus in 10 European laboratories and its application for tracing the spread of related strains. J Clin Microbiol. 2003. 41:1574–1585.
19. Oliveira DC, de Lencastre H. Multiplex PCR strategy for rapid identification of structural types and variants of the mec element in methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 2002. 46:2155–2161.
20. Chen CB, Chang HC, Huang YC. Nasal meticillin-resistant Staphylococcus aureus carriage among intensive care unit hospitalised adult patients in a Taiwanese medical centre: one time-point prevalence, molecular characteristics and risk factors for carriage. J Hosp Infect. 2010. 74:238–244.
21. Tenover FC, McAllister S, Fosheim G, McDougal LK, Carey RB, Limbago B, Lonsway D, Patel JB, Kuehnert MJ, Gorwitz R. Characterization of Staphylococcus aureus isolates from nasal cultures collected from individuals in the United States in 2001 to 2004. J Clin Microbiol. 2008. 46:2837–2841.
22. Dar JA, Thoker MA, Khan JA, Ali A, Khan MA, Rizwan M, Bhat KH, Dar MJ, Ahmed N, Ahmad S. Molecular epidemiology of clinical and carrier strains of methicillin resistant Staphylococcus aureus (MRSA) in the hospital settings of north India. Ann Clin Microbiol Antimicrob. 2006. 5:22.
23. Huang YC, Su LH, Wu TL, Lin TY. Changing molecular epidemiology of methicillin-resistant Staphylococcus aureus bloodstream isolates from a teaching hospital in Northern Taiwan. J Clin Microbiol. 2006. 44:2268–2270.
24. Ko KS, Lee JY, Suh JY, Oh WS, Peck KR, Lee NY, Song JH. Distribution of major genotypes among methicillin-resistant Staphylococcus aureus clones in Asian countries. J Clin Microbiol. 2005. 43:421–426.
25. Lee HJ, Suh JT, Kim YS, Lenz W, Bierbaum G, Schaal KP. Typing and antimicrobial susceptibilities of methicillin resistant Staphylococcus aureus (MRSA) strains isolated in a hospital in Korea. J Korean Med Sci. 2001. 16:381–385.
26. Peck KR, Baek JY, Song JH, Ko KS. Comparison of genotypes and enterotoxin genes between Staphylococcus aureus isolates from blood and nasal colonizers in a Korean hospital. J Korean Med Sci. 2009. 24:585–591.
27. Blanc DS, Petignat C, Wenger A, Kuhn G, Vallet Y, Fracheboud D, Trachsel S, Reymond M, Troillet N, Siegrist HH, Oeuvray S, Bes M, Etienne J, Bille J, Francioli P, Zanetti G. Changing molecular epidemiology of methicillin-resistant Staphylococcus aureus in a small geographic area over an eight-year period. J Clin Microbiol. 2007. 45:3729–3736.
28. Corbella X, Domínguez MA, Pujol M, Ayats J, Sendra M, Pallares R, Ariza J, Gudiol F. Staphylococcus aureus nasal carriage as a marker for subsequent staphylococcal infections in intensive care unit patients. Eur J Clin Microbiol Infect Dis. 1997. 16:351–357.
29. Calfee DP, Salgado CD, Classen D, Arias KM, Podgorny K, Anderson DJ, Burstin H, Coffin SE, Dubberke ER, Fraser V, Gerding DN, Griffin FA, Gross P, Kaye KS, Klompas M, Lo E, Marschall J, Mermel LA, Nicolle L, Pegues DA, Perl TM, Saint S, Weinstein RA, Wise R, Yokoe DS. Strategies to prevent transmission of methicillin-resistant Staphylococcus aureus in acute care hospitals. Infect Control Hosp Epidemiol. 2008. 29:Suppl 1. S62–S80.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download