Abstract
This is a cross-sectional observational study undertaken to explore the current prescription pattern of non-steroidal anti-inflammatory drugs (NSAIDs) and the prevalence of NSAID-induced gastrointestinal (GI) risk factors of orthopaedic patients in real clinical practice in Korea. Study cohort included 3,140 orthopaedic outpatients at 131 hospitals and clinics between January 2008 and August 2008. A self-administered questionnaire was completed by each patient and physician. A simplified risk scoring scale (the Standardized Calculator of Risk for Events; SCORE) was used to measure patients' risk for GI complications. The pattern of NSAIDs prescription was identified from medical recordings. Forty-five percents of the patients belonged to high risk or very high risk groups for GI complications. The cyclooxygenase-2 enzyme (COX-2) selective NSAID showed a propensity to be prescribed more commonly for high/very high GI risk groups, but the rate was still as low as 51%. In conclusion, physician's considerate prescription of NSAIDs with well-understanding of each patient's GI risk factors is strongly encouraged in order to maximize cost effectiveness and to prevent serious GI complications in Korea. Other strategic efforts such as medical association-led education programs and application of Korean electronic SCORE system to hospital order communication system (OCS) should also be accompanied in a way to promote physician's attention.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are one of the most commonly used medications in the world. NSAID-induced adverse reactions involve upper gastrointestinal (GI) tract complications, which can be life-threatening. GI complications occur in 1%-5% of patients taking NSAIDs for more than one year and result in high costs and mortality (1-6). Rates of GI complications may vary substantially depending on each patient's clinical characteristics. Identification of the NSAID-related GI risk factors is therefore crucial in determining the proper treatment for each patient. Many studies already reported that the development of serious GI complications are highly correlated with certain factors, including health status of disability (7, 8), increasing age (2), concomitant use of systemic steroids (9) or anticoagulants (10), history of a GI ulcer of bleed (11), diagnosis of rheumatoid arthritis (4), certain patterns of prior NSAID use (12), history of cardiovascular disease (13), smoking status (7, 14), and NSAID-related GI symptoms (8, 10, 15).
Prior to market release of the first cyclooxygenase-2 enzyme (COX-2) selective inhibitor (celecoxib), northern California health maintenance organization (HMO) developed a treatment guideline for the use of NSAIDs based on the Standardized Calculator of Risk for Events (SCORE) program developed at Stanford University, Division of Immunology and Rheumatology (2, 8). The SCORE tool stratifies patients by risk of developing serious GI complications using patient characteristics that have assigned points. After May 1999, different NSAIDs were recommended for patients depending on the total number of points assigned by the SCORE tool.
It is desirable that physicians consider each patient's clinical factors before prescribing NSAIDs. Some studies already demonstrated the relationship between the clinical factors and the use of the NSAIDs (16). However, few domestic studies have been undertaken on physician's prescription patterns of NSAIDs and the GI risks factors of the patients taking them.
In this study, we evaluated the current prescription pattern of NSAIDs and the prevalence of NSAID-induced GI risk factors of orthopaedic patients in real clinical practice in Korea.
This was a cross-sectional observational study of Korean patients taking NSAIDs for the treatment of orthopaedic problems. Study members included 3,140 all adults (20 yr-old or older) who visited orthopaedic department of 131 hospitals (9 general hospitals, 122 private clinics) in the period between January and August 2008.
A self-administered questionnaire was prepared to assess the risk factors of GI complications. The questionnaire was given to the patients at the outpatient office who agreed to complete the questionnaire and was filled directly by the patients. The questions on the risk factors of GI complications consisted of age, current health status, smoking habit (over 10 cigarettes/day or less), drinking habit (100 g/day), diagnosis of rheumatoid arthritis, history of Helicobactor pylori infection, concomitant use of corticosteroids (number of months in a year), long-term NSAIDs therapy (≥ 3 months), aspirin use, anticoagulant use, selective serotonin reuptake inhibitor (SSRI) use, previous hospitalization event due to GI problems (an ulcer or a bleed), history of GI symptoms and diagnosis of co-morbid disease (cardiovascular, kidney, liver, diabetes, hypertension).
Additionally, we employed GI SCORE for each patient. The GI SCORE takes into account six predictors (age, diagnosis of rheumatoid arthritis, current health status, proportion of time taking steroids, history of a previous GI side effects, and history of a previous GI hospitalization) which were already identified from the questionnaires (16). A certain number of points were allocated for the responses of each predictor and the GI SCORE was calculated for each patient. The risk levels were stratified into 4 groups. A score of 10 or less indicated that risk of a serious GI problem was low; 11-15 points indicated moderate risk; 16-20 points indicated high risk; and more than 20 points indicated very high risk.
The data on the prescription type of the NSAIDs were filled up by the physicians at the outpatient clinic office. The patterns of NSAIDs prescription were analyzed and the percentage of COX-2 inhibitor prescription was also assessed in each risk group.
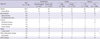
A total of 3,140 adult patients taking NSAIDs were eligible for this study. Women accounted for 69% of the patients and the average age for the group was 63.1 (20-98) yr. When dividing into two age subgroups, 1,690 (54%) patients were aged over 65 yr and females were 75% in the older aged group (≥ 65 yr). Arthritis was the most common cause of taking NSAIDs (67%), followed by spinal disease (9%), fracture (5%), sprain (4%), other inflammatory disease (4%), and others (12%) (Table 1).
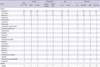
Among the GI risk factors identified in the questionnaire, long-term use of NSAIDs (≥ 3 months) was the most prevalent risk factor in the overall study population, followed by old age (≥ 65 yr) (54%), co-morbid disease (cardiovascular, renal, liver, diabetes, hypertension) (46%), higher NSAID doses (43%), previous GI events (36%) and aspirin use (15%) (Table 2).
When the study groups were stratified into four risk groups according to GI SCORE tool, 45% of the patients belonged to high risk or very high risk groups for GI complications, and female accounted for about 75% (Fig. 1). Female patients tended to be more risky compared to male patients (49% vs 37%), and older groups (≥ 65 yr) had greater GI risk compared to younger groups (< 65 yr) (72% vs 14%). The proportion of arthritis patients also had a tendency to be greater as the risk level was higher (31% [low risk] < 67% [moderate] < 71% [high] < 76% [very high]).
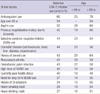
When the type of prescription was analyzed in overall study groups, celecoxib (COX-2 selective inhibitor) was the most commonly used NSAIDs, comprising 36% of the patients. Aceclofenac (22%), meloxicam (15%), zaltoprofen (7%), nabumetone (5%), loxoprofen (5%), and talniflumate (5%) were followed consecutively (Table 3).
COX-2 selective inhibitor was prescribed in 56.2% of very high risk patients and 50.9% of high risk patients. Only 51% of patients at high or very high risk patients were receiving COX-2 selective inhibitors. Analysis of prescription pattern revealed that only 60% of patients with concomitant anticoagulant use, 54% of the patients aged over 65 yr, 52% of patients with concurrent aspirin use were prescribed COX-2 selective inhibitor to decrease the risk of developing GI complications. Its prescription rate was even lower in patients with the other GI risk factors. Comparing two age groups with each GI risk factor, its prescription rate was greater in older aged groups (≥ 65 yr) overall (Table 4).
Multiple case-control population and database studies have confirmed that use of NSAIDs increases the risk of significant GI complications (e.g., bleeding, hospitalization, surgery) from 3.5-fold to 7.8-fold overall (4, 17, 18). The adverse events are usually mild such as in dyspepsia and abdominal pain in most of the cases, but sometimes the events can be life-threatening in cases of bleeding and perforation. In the United States, it is estimated that approximately 107,000 patients are hospitalized annually for NSAID-related GI complications and at least 16,500 NSAID-related deaths occur each year among arthritis patients alone (15).
The symptoms of NSAID-induced GI complication vary and sometimes can be completely absent, that the understanding of the NSAID-induced GI risk factors has been emphasized (19). Several epidemiologic studies have identified the risk factors for developing GI complications, including health status of disability (7, 8), increasing age (2), concomitant use of systemic steroids (9) or anticoagulants (10), history of a GI ulcer of bleed (11), diagnosis of rheumatoid arthritis (4), certain patterns of prior NSAID use (12), history of cardiovascular disease (13), smoking status (7, 14), and NSAID-related GI symptoms (8, 10, 15). While individual risk factors have been identified by a number of studies, the necessity of a multivariate risk factor model to permit estimation of risk in individual patient and initiation of appropriate therapeutic action has been suggested. Fries et al. first created a GI bleeding risk model based on Arthritis, Rheumatism, and Aging Medical Information System (ARAMIS) database in 1991 (2). A refined updated model, the SCORE tool, was presented in abstract form by Singh et al. in 1998. The SCORE tool is accepted as a reliable and accurate predictor of serious NSAID-related GI events in rheumatoid arthritis and osteoarthritis patients and currently used as a main risk model in related studies (16, 20-22).
One main purpose of this study was to understand and present the NSAID-induced GI risk factors and the actual pattern of NSAID prescription in real clinical practice in Korea. Therefore, the GI risk factors already identified in previous studies other than the SCORE tool have been also included in the questionnaire. This study revealed that long-term use of NSAIDs was the most prevalent risk factor in Korean orthopaedic patients, followed by old age (over 65 yr) (54%), co-morbid disease (cardiovascular, renal, liver, diabetes, hypertension) (46%), use of high dose NSAIDs (43%), previous GI events (36%) and aspirin use (15%) (Table 2). The Korean Knee Society (KKS) presented comparable results, yielding old age over 65 yr (56%), history of previous GI symptom (40%), presence of co-morbid disease (25%) were prevalent risk factors in the NSAID-induced GI risk management study in 2009 (22).
Our study also showed that about half (45% in this study) of the population taking NSAIDs for a number of reasons were classified into high/very high risk groups for GI complications, but only 51% of them were given COX-2 selective inhibitor for the prevention of GI events. Similarly, only 50% of old patients (over 65 yr) with previous GI symptom and only 60% of old aged patients previously hospitalized due to GI events were prescribed COX-2 selective inhibitor. Korea Food and Drug Administration has forbidden the combined use of non-selective NSAIDs with aspirin due to high bleeding tendency and decreased renal function. Nonetheless, the proportion of the combined use of non-selective NSAIDs among the patients taking aspirin was high up to 48% in our study. Physician's neglect on patient's GI factor in real practice, each physician's preference for a specific NSAID, vigorous marketing of pharmaceutical companies, harsh curtailment of medical expenses by Health Insurance Review and Assessment Service (HIRAS) as well as unawareness of the patients could be accounted for the inappropriate NSAIDs prescription.
Although COX-2 selective inhibitor significantly decreases GI complications compared to non-selective NSAIDs, its unconditional prescription is inappropriate because cost-effectiveness of COX-2 selective inhibitor is likely to be lower in population at lower risk for GI complications (16). The northern California HMO guideline recommended different NSAIDs for patients depending on the total number of points assigned by the SOCRE tool (16). A COX-2 selective inhibitor was recommended for patients with a score of 21 or greater; a moderate-risk NSAID such as nabumetone, etodolac, or salsalate for patients with intermediate scores (16-20 points); and a traditional NSAID such as ibuprofen, sulindac or naproxen for patients with the lowest scores (1-15 points). This treatment guideline was designed to maximize the cost-effectiveness of NSAID utilization by prescribing less expensive non-selective NSAIDs for the patients at low GI risk and reserving expensive COX-2 selective inhibitor for the patients at higher risk. With an effort such as mailing the guideline to the physicians enrolled in the HMO and education program through drug education pharmacists, a 5.5-fold difference in the use of COX-2 selective NSAIDs was obtained between the patients in the highest-risk decile and the patients in the lowest risk decile (16). Correspondingly, the risk stratification model used in developing the SCORE tool showed that the risk of hospitalization or death due to NSAID-related GI complication decreased by approximately 4-fold between arthritis patients in higher and lower risk strata (2, 16). Our study resulted in similar pattern of NSAID utilization, showing more frequent use of COX-2 selective inhibitor in higher risk groups (6% [low] < 28% [moderate] < 51% [high] < 56% [very high]) and more common use of non-selective NSAIDs in less risk groups. However, it is evident that little effort has been made to decrease GI complication for Korean patients taking NSAIDs as mentioned before. In an observational study by Korea Knee Society, only 41% of overall patients taking NSAIDs and 43% of patients at high risk groups were prescribed GI protective medication, indicating that physicians make little efforts to consider patient's individual GI risk factors in real practice. Comparable results were reported that the prescription rates of GI protector in patients with current GI symptom and in patients without it were not significantly different (44% vs 39%) (22), meaning that physicians prescribe GI protector rather in the customary manner without considering patient's factor. Physician's voluntary efforts to put more attention on individual factor, patient's self-awareness on the adverse effects caused by NSAIDs as well as government-led promotion programs such as mailing guideline booklets and periodic education program could aid in decreasing GI complications induced by NSAIDs medication.
Cote et al. (23) reported that after the intervention (combination of education and computer alert), the use of gastroprotector in high risk patients increased from 45% with no intervention to 52% with physician education alone, to 46% with the computer alert alone, and to 67% with the combination of physician education and computer alert (P < 0.005). Recently, a revised SCORE tool (electronic SCORE) was designed with an effort to easily access patient criteria and estimate a patient's risk using computer-stored medical and demographic information (21). Application of electronic SCORE to hospital Order-Communication system (OCS) could be another method to easily predict individual's risk for NSAID-induced GI complication.
This study has a few limitations. First, there were no researches on the pattern and type of gastroprotector use. As mentioned previously, Korean Knee Society reported the overall prescription rate of gastroprotector was as low as 41% and physicians used gastroprotector in customary manner rather than considering patient's individual factor including current GI symptom (22). Young medical specialists (with certification year less than 10) prescribed gastroprotectors more actively, assuming that doctors recently educated were rather well aware of the severity of adverse effects caused by NSAIDs. The most commonly used gastroprotector was cytoprotectant followed by H2 receptor antagonist, gastroprokinetic and proton pump inhibitor (22). The low prescription rate of proton pump inhibitor seemed to be related to low rate of reimbursement by National Health Insurance (NHI). Secondly, this study was a cross-sectional observational study designed to obtain an initial data for the current pattern of NSAIDs utilization and confirm the prevalence of GI risk factors of Korean patients taking NSAIDs. Therefore, we did not put much effort to develop new GI risk factor. More interesting data could be obtained if we had progressed more research on the topic such as new GI risk factor typical to Korean population, degree of patient's awareness on adverse effects by NSAIDs, physician's criterion or principle in choosing the type of NSAIDs or gastroprotectors. This study is still meaningful in that it offered valuable data on the current prescription pattern of NSAIDs in real clinical practice in Korea at the very first, and gave us a moment to share insights on the solution to minimize NSAID-induced GI complications effectively. Strategic efforts such as physician's voluntary attention to estimate individual patient's risk factor, patient's self-awareness on the adverse effects caused by NSAIDs, government-led campaign activities such as mailing guideline booklets, medical association-led periodic education programs for physicians and patients, and development and application of Korean electronic SCORE system to hospital Order Communication System (OCS) could aid in decreasing GI complications induced by NSAIDs medication.
In conclusion, although about half of Korean orthopaedic patients receiving NSAIDs are at high or very high risk for NSAID-induced GI complications, physicians' prescription pattern for NSAIDs appears to be inconsiderate. Physician's considerate prescription of NSAIDs with well-understanding of each patient's GI risk factors is strongly encouraged in order to maximize cost effectiveness as well as to prevent serious GI complications in Korea. Other strategic efforts such as patient's self-awareness, government-led educational campaigns, medical association-led educational programs, and application of Korean electronic SCORE system to hospital OCS should also be accompanied in a way to promote physician's attention.
Figures and Tables
ACKNOWLEDGMENTS
The author sincerely appreciate Seong-il Bin, M.D., Choong-Hyeok Choi, M.D., Hee-Chun Kim, M.D., Dong Chul Lee, M.D., Myung-Chul Lee, M.D., Byoung-Hyun Min, M.D., Seo Seung Suk, M.D., Soo-Jae Yim, M.D. and other orthopaedic surgeons in private clinics for their contribution to data collection in this study.
AUTHOR SUMMARY
Prescription Pattern of NSAIDs and the Prevalence of NSAID-induced Gastrointestinal Risk Factors of Orthopaedic Patients in Clinical Practice in Korea
Sung-Hun Lee, Chang-Dong Han, Ick-Hwan Yang, and Chul-Won Ha
This cross-sectional observation study was aimed to explore the current prescription pattern of non-steroidal anti-inflammatory drugs (NSAIDs) and the prevalence of NSAID-induced GI risk factors in orthopedic patients (3140 orthopedic outpatients at 131 hospitals in Korea). Questionnaires and medical recordings showed that 45% of the patients belong to high risk or very high risk groups for GI complications. However, only 51% of risked patients were prescribed for COX-2 selective NSAID. Physician's considerate prescription of NSAIDs with well-understanding of each patient's GI risk factors is strongly requested in Korea.
References
1. Schlansky B, Hwang JH. Prevention of nonsteroidal anti-inflammatory drug-induced gastropathy. J Gastroenterol. 2009. 44:Suppl 19. 44–52.
2. Fries JF, Williams CA, Bloch DA, Michel BA. Nonsteroidal anti-inflammatory drug-associated gastropathy: incidence and risk factor models. Am J Med. 1991. 91:213–222.
3. Johnson RE, Hornbrook MC, Hooker RS, Woodson GT, Shneidman R. Analysis of the costs of NSAID-associated gastropathy. Experience in a US health maintenance organisation. Pharmacoeconomics. 1997. 12:76–88.
4. Singh G, Rosen Ramey D. NSAID induced gastrointestinal complications: the ARAMIS perspective--1997. Arthritis, Rheumatism, and Aging Medical Information System. J Rheumatol Suppl. 1998. 51:8–16.
5. White TJ, Arakelian A, Rho JP. Counting the costs of drug-related adverse events. Pharmacoeconomics. 1999. 15:445–458.
6. Tramèr MR, Moore RA, Reynolds DJ, McQuay HJ. Quantitative estimation of rare adverse events which follow a biological progression: a new model applied to chronic NSAID use. Pain. 2000. 85:169–182.
7. Singh G, Triadafilopoulos G. Epidemiology of NSAID induced gastrointestinal complications. J Rheumatol Suppl. 1999. 56:18–24.
8. Fries JF. NSAID GI toxicity: epidemiology. J Musculoskel Med. 1991. 8:21–28.
9. Piper JM, Ray WA, Daugherty JR, Griffin MR. Corticosteroid use and peptic ulcer disease: role of nonsteroidal anti-inflammatory drugs. Ann Intern Med. 1991. 114:735–740.
10. Shorr RI, Ray WA, Daugherty JR, Griffin MR. Concurrent use of nonsteroidal anti-inflammatory drugs and oral anticoagulants places elderly persons at high risk for hemorrhagic peptic ulcer disease. Arch Intern Med. 1993. 153:1665–1670.
11. Gabriel SE, Jaakkimainen L, Bombardier C. Risk for serious gastrointestinal complications related to use of nonsteroidal anti-inflammatory drugs. A meta-analysis. Ann Intern Med. 1991. 115:787–796.
12. Gutthann SP, García Rodríguez LA, Raiford DS. Individual nonsteroidal antiinflammatory drugs and other risk factors for upper gastrointestinal bleeding and perforation. Epidemiology. 1997. 8:18–24.
13. Silverstein FE, Graham DY, Senior JR, Davies HW, Struthers BJ, Bittman RM, Geis GS. Misoprostol reduces serious gastrointestinal complications in patients with rheumatoid arthritis receiving nonsteroidal anti-inflammatory drugs. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 1995. 123:241–249.
14. McIntosh JH, Fung CS, Berry G, Piper DW. Smoking, nonsteroidal anti-inflammatory drugs, and acetaminophen in gastric ulcer. A study of associations and of the effects of previous diagnosis on exposure patterns. Am J Epidemiol. 1988. 128:761–770.
15. Singh G. Recent considerations in nonsteroidal anti-inflammatory drug gastropathy. Am J Med. 1998. 105:31S–38S.
16. Bull SA, Conell C, Campen DH. Relationship of clinical factors to the use of COX-2 selective NSAIDs within an arthritis population in a large HMO. J Manag Care Pharm. 2002. 8:252–258.
17. García Rodríguez LA, Barreales Tolosa L. Risk of upper gastrointestinal complications among users of traditional NSAIDs and COXIBs in the general population. Gastroenterology. 2007. 132:498–506.
18. Koncz TA, Lister SP, Makinson GT. Gastroprotection in patients prescribed non-selective NSAIDs, and the risk of related hospitalization. Curr Med Res Opin. 2008. 24:3405–3412.
19. Taha AS, Dahill S, Sturrock RD, Lee FD, Russell RI. Predicting NSAID related ulcers--assessment of clinical and pathological risk factors and importance of differences in NSAID. Gut. 1994. 35:891–895.
20. Fries JF, Bruce B. Rates of serious gastrointestinal events from low dose use of acetylsalicylic acid, acetaminophen, and ibuprofen in patients with osteoarthritis and rheumatoid arthritis. J Rheumatol. 2003. 30:2226–2233.
21. Cheetham TC, Levy G, Spence M. Predicting the risk of gastrointestinal bleeding due to nonsteroidal antiinflammatory drugs: NSAID electronic assessment of risk. J Rheumatol. 2003. 30:2241–2244.
22. NSAID-induced GI management study. MO online. c2000-2011. accessed on14 Mar 2011. Korea: Medical observer;Available at http://www.moonline.co.kr/News/news_view.aspx?Cid=H1707&Cno=38293.
23. Coté GA, Rice JP, Bulsiewicz W, Norvell JP, Christensen K, Bobb A, Postelnick M, Howden CW. Use of physician education and computer alert to improve targeted use of gastroprotection among NSAID users. Am J Gastroenterol. 2008. 103:1097–1103.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download