Abstract
The precore (G1896A) and core promoter (A1762T, G1764A) mutations of the hepatitis B virus gene are known to be associated with changes in immunologic phase or the progression to complicated liver disease in adults. We analyzed these mutations in chronically HBV-infected children. Serum was collected from 37 children with chronic HBV infection from March 2005 to September 2008. HBV DNA extraction and nested PCR were followed by sequencing of the PCR products. The children were 6.7 ± 4.6 yr old. All of 37 children had HBV genotype C. Of the cohort, 31 (83.8%) were HBeAg-positive and 6 (16.2%) were HBeAg-negative; the former group comprised 18 (48.6%) who were in the immune-tolerance phase (ITP) and 13 (35.2%) in the immune-clearance phase (ICP). Most of the patients had HBV DNA levels of > 1.0 × 108 copies/mL. In the ITP group, only 1 (5.5%) had core promoter mutations, and none had the precore mutation. In the ICP group, only 2 (15.4%) had core promoter mutations; the remaining 6 patients had HBV DNA levels of < 2.0 × 103 copies/mL and no core promoter/precore mutations. The very low incidence of the precore/core promoter gene mutation, in children, suggests that these mutations may be the result of life-long chronic HBV infection.
There are three phases in the natural history of chronic HBV infection (1). The first is the immune-tolerant phase (ITP) defined by hepatitis B e antigen (HBeAg)-positive, normal hepatic enzyme levels and high serum HBV DNA concentrations. The second is the immune-clearance phase (ICP) defined by HBeAg-positive, abnormal hepatic enzyme levels and falling serum HBV DNA concentrations. The third is the HBeAg negative carrier stage defined by seroconversion from HBeAg to hepatitis B e antibody (HBeAb), normal hepatic enzyme levels and low or nondetectable serum HBV DNA concentrations. After the third phase, reactivation may develop. The progression from the first to the third or reactivation phase over several decades may cause the development of complications of chronic HBV infection, such as liver cirrhosis and hepatocellular carcinoma (2).
Precore mutations, such as G1896A (guanine-to-adenine mutation at nucleotide 1,896), and core promoter (CP) mutations, including A1762T (adenine-to-thymine mutation at nucleotide 1,762) and G1764A (guanine-to-adenine mutation at nucleotide 1,764), are known to be associated with HBeAg status in adults (3). The precore stop-codon mutation (G1896A) abolishes HBeAg and the dual mutation in the CP region (A1762T, G1764A) down-regulates HBeAg production. These mutations are also reported to be associated with change of the immunologic phase and the resulting severity of liver disease in adults with chronic HBV infection (4, 5). However, the causal relationship between these mutations and the change of the immunologic phase or severity of liver disease has not been established definitively. Some researchers have reported that these mutations are not related to either immunologic change or liver disease (1, 6).
The aim of this study was to determine the incidence of precore/CP mutations in relation to the change of the immunologic phase in young chronic infected children.
Serum was collected from 37 children with chronic HBV infection who had been HBsAg-positive for over 6 months and had visited Jeju National University Hospital (JNUH), Jeju, Korea between March 2005 and September 2008. The number of blood sampling from each patient was 3 to 5 times matching to every visit to the pediatric clinic. Serum from patients who were taking antiviral agents, such as lamivudine or adefovir, was excluded from the analysis. All sera were immediately stored in a deep freezer at -80.0℃ until required for analysis. We also recorded information regarding the patients' serology, levels of aspartate aminotransferase (AST), alanine aminotransferase (ALT), HBeAg/HBeAb, and HBV DNA (copies/mL) in serum.
Normal serum AST and ALT level was defined when lower than 45 IU/L. Immune tolerant phase was defined by normal AST/AST level, HBeAg positive and high serum HBV DNA concentrations (7). The transient abnormal AST/ALT level caused by other viral infections was also clarified to this phase in our study. Immune clearance phase was defined by abnormal AST/AST level, HBeAg positive and falling serum HBV DNA concentrations (7). Immune clearance phase was differentiated from the transient nonspecific hepatitis caused by other viral infection in the children.
HBV DNA levels were quantified by a polymerase chain reaction (PCR) assay with a lower limit of detection of 2×102 copies/mL and a linearity range of 2 × 102-2 × 105 copies/mL (Cobas Amplicor HBV Monitor, Roche Diagnostic Systems, Pleasanton, CA, USA). All HBeAg-positive samples were prediluted up to 106-fold, and a 105-fold dilution was used for initial testing.
HBV DNA was extracted at room temperature from 200 µL aliquots of each child's serum (thawed at 4.0℃) using the High Pure Viral Nucleic Acid Kit (Roche, Penzberg, Germany). The extracted HBV DNA was immediately used for genotyping and nested PCR.
Using genotype-specific primers developed by Naito et al. (8), the nucleotide sequences of the pre-S1 through S genes were amplified. Genotyping was performed for only three (A-C) of the six (A-F) types. The first PCR was performed using universal primers, including P1 and S1-2, and was followed by a second PCR, which was performed using the primer mixtures specifying different genotypes, including A, B, and C. Finally, genotyping was performed based on the band sizes (type A, 281 bp; type B, 122 bp; and type C, 68 bp) shown on electrophoresis (data not shown).
The tube for the first PCR of the precore and CP genes was prepared using 50 µL aliquots of mixtures containing 10 µL of extracted HBV DNA, 1 µL of 10 pM of external primers, each of the four dNTPs at 0.2 mM, 1.5 mM MgCl2, 1 U of Taq polymerase, 5 µL of 10 LPCR buffer (Promega, Madison, WI, USA), and 32 µL of nuclease-free water. The external primers were P1 (5'-CATAAGAGGACTCTTGGACT-3', positions 1,653-1,672) and P2 (5'-GGAAAGAAATCAGAAGGCA-3', positions 1,974-1,956). The mixture for the first PCR was put into the thermocycler and the following PCR protocol used: denaturation at 94.0℃ for 5 min; followed by 40 cycles of denaturation at 94.0℃ for 30 sec, annealing at 54.0℃, and extension at 72.0℃ for 45 sec; with a final extension at 72.0℃ for 10 min.
The tube for the second PCR was prepared using the 50 µL of mixture comprising the first PCR product, 1 µL of 10 pM of internal primers, 0.2 mM of each of the four dNTPs, 1.5 mM MgCl2, 1 U of Taq polymerase, 5 µL of 10 LPCR buffer (Promega), and 40 µL of nuclease-free water. The internal primers were P3 (5'-GGACTCTTGGACTCTCAGCAA-3', positions 1,660-1,680) and P4 (5'-TCCACAGAAGCTCCAAATTCTTT-3', positions 1,941-1,919). The protocol for the second PCR was the same as for the first. The final PCR products were identified on electrophoresis carried out using 1.0% agarose gel stained with ethidium bromide.
Finally, the second PCR product was sequenced using an ABI PRISM BigDye Terminator v3.1 cycle sequencing kit (Applied Biosystems, Foster City, CA, USA) and then analyzed using a genetic analyzer (ABI PRISM 3100, Applied Biosystems). The PCR products, which included 4 µL of Terminator Ready Reaction Mix, 1 µL of cleaned PCR product (20-40 ng of PCR product), 1 µL of primer (5 pM), and sterile water to a total volume of 10 µL, was placed in a reaction tube. Cycle sequencing was then carried out as follows: 30 cycles of 96.0℃ for 10 sec, 50.0℃ for 5 sec, and 60.0℃ for 4 min. Precipitation and loading of the samples were then performed according to the manufacturer's instructions.
Results are expressed as the mean ± standard deviation (range). Differences between categorical variables were analyzed using chi-squared test. Kruskal-Wallis test was used for continous variables according to 3 immunologic phases. A P value of less than 0.05 (two-tailed) was considered statistically significant.
Among the 37 children with chronic HBV infections (age 6.7 ± 4.6 yr, mean ± SD; range 10 months-15.8 yr), vertical infection was the most common route of infection (n = 31, 83.8%), followed by another member of the family (n = 3, 8.1%); the origin of infection was unknown in three patients (8.1%).
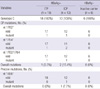
Of the cohort, 18 patients (48.6%) were in the ITP, with high viral replication and normal ALT levels (Table 1), and 13 (35.2%) were in the ICP, with viral replication and elevated ALT levels. Six patients (16.2%) were in the HBeAg negative carrier state (Table 1). There was no significant association between gender and immunologic phase (P = 0.189, chi-squared test). The mean age was highest in the HBeAg negative carrier group, followed by the ICP and ITP groups (Table 1).
Hepatic enzyme levels, including AST and ALT, were all near the upper limit of normal in the ITP group, three or five times the upper limit of normal in the ICP group, and near the lower limit of normal in those in the HBeAg negative carrier state. The distribution of the two hepatic enzymes differed significantly between the three immunologic phase groups (P < 0.001, Kruskal-Wallis test; Table 1).
In the ITP and ICP groups, most patients had high HBV DNA levels (i.e., more than 1.0 × 108 copies/mL). In the HBeAg negative carrier group, all of the patients had low HBV DNA levels (range 102-105 copies/mL; Table 1). The distribution of HBV DNA levels differed significantly between the groups (P < 0.001, chi-squared test; Table 1).
All of the 37 patients had HBV genotype C. Only 3 of the 37 patients exhibited CP mutations. Only one (5.5%) of the 18 ITP patients had the G1764A mutation and 1 had the A1762T/G1764A mutation (Table 2). Of the 13 patients in the ICP group, only two (15.4%) exhibited CP mutations, including one A1762T/G1764A mutation. None of the patients in the HBeAg negative carrier group had any CP mutations.
Only one of the entire cohort exhibited a precore mutation: an ICP patient (7.7%). The distributions of both the precore and CP mutations did not differ significantly (A1762T, P = 0.788; G1764A, P = 0.447; G1896A, P = 0.387, chi-squared test; Table 2).
Precore and CP gene mutations frequently occur over several decades of chronic HBV infection. The common mutations of the CP genes are the adenine-to-thymine mutation at nucleotide 1762 (A1762T) and/or the guanine-to-adenine mutation at nucleotide 1764 (G1764A) (9-11). In the precore gene, the guanine-to-adenine mutation at nucleotide 1896 (G1896A) is the most prevalent (3, 11).
There are many conflicting reports regarding the association between these gene mutations and disease severity in chronic HBV infection, with progression from the immune tolerant phase to the HBeAg negative carrier or reactivation phase (12). There are some reports that precore/CP mutations are correlated with the patient's immunological and/or disease status (4, 5, 13-17), but others that those mutations have no significant correlation with viral replication or liver damage (1, 6).
The prevalence of CP mutations is higher than that of precore mutations (4) among Koreans, in whom only the C genotype is expressed (18). In Korean adults (4), CP mutations (A1762T, G1654A) were found in 95.0% of ICP patients, in 67% of HBeAg negative carriers, and in 30.0% of ITP patients. The precore mutation (G1896A) was less prevalent than CP mutations (i.e., 5% of ICP patients, 32.5% of HBeAg negative carriers, and 22.5% of ITP patients). In Taiwanese adults with HBeAg negative chronic hepatitis B (19), the overall prevalence of the precore stop codon mutant and basal core promoter mutant was 67% and 60%, respectively. Genotype B and C are major strains in Taiwan.
In German adults with HBeAg negative chronic hepatitis B (20), the overall prevalence of the precore stop codon mutant and basal core promoter mutant was 46% and 59%, respectively. Genotype A and D are major strains in Germany. In the analysis of these mutation rates of 3 countries, it seems to be similar results in HBeAg negative carriers.
Compared with reports in Korean adults (4), the CP mutation rate of our study was very low: 9.1% of the ITP group, 11.1% of the ICP, and 0% of those in the HBeAg negative carrier state. The incidence of the precore mutation was extremely low (4.1%), and was found only in the ITP group. There are a few reports associated with precore or core promoter mutation of HBV in chronic infected children in other countries (21-24). In the analysis for 89 sera from 32 chronic HBV infected Taiwanese children (24), precore stop codon mutant was found in 10%-25% of children before HBeAg seroconversion and in 39% of children after seroconversion. Core promoter mutations rates of Taiwanese children (22) were 9.1% in seroconverters (HBeAg negative carrier) and 5.5% in the nonseroconverters. In the analysis of 155 European children (21), 2 (2.2%) of 90 HBeAg positive patients and 5 (7.7%) of 65 anti-HBe positive children had precore stop codon mutation.
In the HBeAg negative carriers, the mutation rates of precore stop codon and basal core promoter genes are high in adult and low in children. This wide disparity suggest that these mutations may be the result of life-long chronic HBV infection.
These low mutation rates in our study may originate from the mutated HBV gene of the patient's mother when the patient was born. Unfortunately, the incidence of these gene mutations in the mothers of all 37 children was not analyzed. The actual mutation rate of these genes may thus be nearly 0%, despite the changes in immunologic phase. These findings suggest that precore/CP mutation is a only secondary occurrence, and not the cause of immunological change in patients with chronic HBV infection. These findings also support the opinion of Chang et al. (24), who stated that "The precore stop codon mutant is selected by host immune pressure, but is not an initiator of the loss of immune tolerance during chronic HBV infection in children".
Although HBeAg seroconversion is estimated to be affected by age (Table 1), the age distribution did not differ significantly with the immunologic phase (P = 0.061, Kruskal-Wallis test). This may be due to the small size of each group and the wide standard deviations.
There are limitations in our study. The first is small sample size. The second is that direct sequencing of DNA samples of nested PCR performed in our study reflects the major strains of HBV. It is possible that the prevalence of precore/core promoter gene mutation in these samples is underestimated when the mutant strains are minor strains. HBV viral quasi-species evolution in the precore/core gene before and after HbeAg seroconversion in chronic HBV infected patients was reported (25). They suggested that the high viral diversity, including the entire mutant strains, may be associated with the change from the immune tolerance pahse to the immune clearance phase (25).
HBeAg-negative chronic hepatitis B, which represents the reactivation phase, is common in adults and is associated with a high prevalence of precore/CP mutations (26). However, as confirmed in the present study, this type is rare in children (27).
The geographical distribution of HBV genotypes reveals a high prevalence of genotypes B and C in East Asia (12, 28, 29), and countries that have many immigrants of East Asiatic origin, such as Canada (30). Only genotype C was found in previous Korean studies (18, 28). In our study, all 37 patients had genotype C.
In conclusion, the very low incidence of the precore/core promoter gene mutation, in children, suggests that these mutations may be the result of life-long chronic HBV infection.
Figures and Tables
Table 1
Baseline characteristics of the 37 patients with chronic hepatitis B virus (HBV) infection

*P = 0.189 (χ2 test); †P = 0.061 (Kruskal-Wallis test); ‡P < 0.001 (Kruskal-Wallis test); §P < 0.001 (Kruskal-Wallis test); ∥P ≤ 0.001 (χ2 test); ¶Mean ± 2SD. ITP, immune tolerance phase; ICP, immune clearance phase; AST, aspartate aminotransferase; ALT, alanine aminotransferase; high, > 108 copies/mL; moderate, 105-108 copies/mL; low, 102-105 copies/mL; negative, < 102 copies/mL. From 3 to 5 samples of each patient, the highest value out of laboratory data and the value at the time of mutation were selected in the patients without and with precore/core gene mutation, respectively.
AUTHOR SUMMARY
Precore and Core Promoter Mutations of the Hepatitis B Virus Gene in the Chronic Genotype C -Infected Child
Hyun Sik Kang, Ki Soo Kang, and Byung-Cheol Song
The precore (G1896A) and core promoter (A1762T, G1764A) mutations of the hepatitis B virus gene are known to be associated with changes in immunologic phase or the progression to complicated liver disease in adults. In contrast to the high mutation rates in adults, our study in children revealed the very low mutation rates of precore and core promoter gene. Such results suggest that these mutations may be the result of life-long chronic HBV infection.
References
1. Yuen MF, Lai CL. Natural history of chronic hepatitis B virus infection. J Gastroenterol Hepatol. 2000. 15:Suppl. E20–E24.
2. Rehermann B, Nascimbeni M. Immunology of hepatitis B virus and hepatitis C virus infection. Nat Rev Immunol. 2005. 5:215–229.
3. Carman WF, Jacyna MR, Hadziyannis S, Karayiannis P, McGarvey MJ, Makris A, Thomas HC. Mutation preventing formation of hepatitis b e antigen in patients with chronic hepatitis b infection. Lancet. 1989. 2:588–591.
4. Song BC, Cui XJ, Kim HU, Cho YK. Sequential accumulation of the basal core promoter and the precore mutations in the progression of hepatitis b virus-related chronic liver disease. Intervirology. 2006. 49:266–273.
5. Chu CJ, Keeffe EB, Han SH, Perrillo RP, Min AD, Soldevila-Pico C, Carey W, Brown RS Jr, Luketic VA, Terrault N, Lok AS. U.S. HBV Epidemiology Study Group. Prevalence of HBV precore/core promoter variants in the United States. Hepatology. 2003. 38:619–628.
6. Chun YK, Kim JY, Woo HJ, Oh SM, Kang I, Ha J, Kim SS. No significant correlation exists between core promoter mutations, viral replication, and liver damage in chronic hepatitis B infection. Hepatology. 2000. 32:1154–1162.
7. Liaw YF, Chu CM. Hepatitis B virus infection. Lancet. 2009. 373:582–592.
8. Naito H, Hayashi S, Abe K. Rapid and specific genotyping system for hepatitis B virus corresponding to six major genotypes by PCR using type-specific primers. J Clin Microbiol. 2001. 39:362–364.
9. Yuh CH, Chang YL, Ting LP. Transcriptional regulation of precore and pregenomic RNAs of hepatitis B virus. J Virol. 1992. 66:4073–4084.
10. Chen IH, Huang CJ, Ting LP. Overlapping initiator and TATA box functions in the basal core promoter of hepatitis B virus. J Virol. 1995. 69:3647–3657.
11. Locarnini S, McMillan J, Bartholomeusz A. The hepatitis B virus and common mutants. Semin Liver Dis. 2003. 23:5–20.
12. Pumpens P, Borisova GP, Crowther RA, Grens E. Hepatitis B virus core particles as epitope carriers. Intervirology. 1995. 38:63–74.
13. Hou J, Lau GK, Cheng J, Cheng CC, Luo K, Carman WF. T1762/a1764 variants of the basal core promoter of hepatitis b virus; serological and clinical correlations in chinese patients. Liver. 1999. 19:411–417.
14. Friedt M, Gerner P, Lausch E, Trübel H, Zabel B, Wirth S. Mutations in the basic core promotor and the precore region of hepatitis B virus and their selection in children with fulminant and chronic hepatitis B. Hepatology. 1999. 29:1252–1258.
15. Chen CH, Lee CM, Lu SN, Changchien CS, Eng HL, Huang CM, Wang JH, Hung CH, Hu TH. Clinical significance of hepatitis B virus (HBV) genotypes and precore and core promoter mutations affecting HBV e antigen expression in Taiwan. J Clin Microbiol. 2005. 43:6000–6006.
16. Lin CL, Liao LY, Wang CS, Chen PJ, Lai MY, Chen DS, Kao JH. Basal core-promoter mutant of hepatitis B virus and progression of liver disease in hepatitis B e antigen-negative chronic hepatitis B. Liver Int. 2005. 25:564–570.
17. Kim HJ, Yoo BC. The prevalence and clinical significance of precore and core promoter mutations in Korean patients with chronic hepatitis B virus infection. Korean J Hepatol. 2002. 8:149–156.
18. Song BC, Cui XJ, Kim H. Hepatitis B virus genotypes in Korea: an endemic area of hepatitis B virus infection. Intervirology. 2005. 48:133–137.
19. Lin CL, Liao LY, Liu CJ, Chen PJ, Lai MY, Kao JH, Chen DS. Hepatitis B genotypes and precore/basal core promoter mutants in HBeAg-negative chronic hepatitis B. J Gastroenterol. 2002. 37:283–287.
20. Funk ML, Rosenberg DM, Lok AS. World-wide epidemiology of HBeAg-negative chronic hepatitis B and associated precore and core promoter variants. J Viral Hepat. 2002. 9:52–61.
21. Wintermeyer P, Gerner P, Gehring S, Karimi A, Wirth S. Prevalence of hepatitis B virus precore stop codon mutations in chronically infected children. World J Gastroenterol. 2006. 12:2235–2238.
22. Ni YH, Chang MH, Hsu HY, Tsuei DJ. Longitudinal study on mutation profiles of core promoter and precore regions of the hepatitis B virus genome in children. Pediatr Res. 2004. 56:396–399.
23. Barbera C, Calvo P, Coscia A, Perugini L, Dastoli G, Randone A, Bonino F, Brunetto MR. Precore mutant hepatitis B virus and outcome of chronic infection and hepatitis in hepatitis B e antigen-positive children. Pediatr Res. 1994. 36:347–350.
24. Chang MH, Hsu HY, Ni YH, Tsai KS, Lee PI, Chen PJ, Hsu YL, Chen DS. Precore stop codon mutant in chronic hepatitis B virus infection in children: its relation to hepatitis B e seroconversion and maternal hepatitis B surface antigen. J Hepatol. 1998. 28:915–922.
25. Lim SG, Cheng Y, Guindon S, Seet BL, Lee LY, Hu P, Wasser S, Peter FJ, Tan T, Goode M, Rodrigo AG. Viral quasi-species evolution during hepatitis Be antigen seroconversion. Gastroenterology. 2007. 133:951–958.
26. Hadziyannis SJ, Vassilopoulos D. Hepatitis B e antigen-negative chronic hepatitis B. Hepatology. 2001. 34:617–624.
27. Söderström A, Norkrans G, Conradi N, Krantz M, Horal P, Lindh M. Histologic activity of childhood chronic hepatitis B related to viremia levels, genotypes, mutations, and epidemiologic factors. J Pediatr Gastroenterol Nutr. 2002. 35:487–494.
28. Odgerel Z, Nho KB, Moon JY, Kee SH, Park KS, Song KJ, Baek LJ, Yeon JE, Byun KS, Lee CH, Song JW. Complete genome sequence and phylogenetic analysis of hepatitis B virus (HBV) isolates from patients with chronic HBV infection in Korea. J Med Virol. 2003. 71:499–503.
29. Yuen MF, Sablon E, Tanaka Y, Kato T, Mizokami M, Doutreloigne J, Yuan HJ, Wong DK, Sum SM, Lai CL. Epidemiological study of hepatitis B virus genotypes, core promoter and precore mutations of chronic hepatitis B infection in Hong Kong. J Hepatol. 2004. 41:119–125.
30. Fung SK, Wong FS, Wong DK, Hussain MT, Lok AS. Hepatitis B virus genotypes, precore and core promoter variants among predominantly Asian patients with chronic HBV infection in a Canadian center. Liver Int. 2006. 26:796–804.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download