Abstract
We investigated the clinical significance of large difference (≥ 2 points) between biopsy-derived (bGS) and post-prostatectomy Gleason scores (pGS). At 14 medical centers in Korea, 1,582 men who underwent radical prostatectomy for prostate cancer were included. According to the difference between bGS and pGS, the patients were divided into three groups: A (decreased in pGS ≥ 2, n = 30), B (changed in pGS ≤ 1, n = 1,361; control group), and C (increased in pGS ≥ 2, n = 55). We evaluated various clinicopathological factors of prostate cancer and hazards for biochemical failure. Group A showed significantly higher mean maximal percentage of cancer in the positive cores (max%) and pathological T stage than control. In group C, the number of biopsy core was significantly smaller, however, tumor volume and max% were significantly higher and more positive biopsy cores were presented than control. Worse pathological stage and more margin-positive were observed in group A and C than in control. Hazard ratio for biochemical failure was also higher in group A and C (P = 0.001). However, the groups were not independent factors in multivariate analysis. In conclusion, large difference between bGS and pGS shows poor prognosis even in the decreased group. However it is not an independent prognostic factor for biochemical failure.
The prostate cancer is the most common malignant disease of men in Western countries (1). Its incidence is continuously increasing Korea and its age-standardized incidence rates per 100,000 men was 4.6 cases, which was the 8th-highest cause among the organ-specific malignant tumors in 2007 (2). Many pre-treatment prognostic factors have been proposed to be used to determine one of the treatment modalities and the Gleason system was proved to be one of the most important prognostic factors. Histological variation within each tumor brought two grades, the predominant, or primary grade and the less extensive, or secondary grade (3). Biopsy-derived Gleason score (bGS) is used as one of the most important pretreatment prognostic factors (4, 5). Though the overall accuracy of Gleason grade on needle biopsies was found to be good in predicting prostatectomy specimen grade, upgrading and downgrading have been reported 9%-26% and 18%-22%, respectively (6, 7). Moreover, large difference (≥ 2 points) between biopsy-derived and post-prostatectomy Gleason scores (pGS) may confuse the clinicians in consulting the patients. We investigated the clinical significance of this difference.
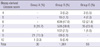
At 14 medical centers in Korea, the medical records of 1,582 men who underwent radical prostatectomy for prostate cancer between 1995 and 2007 were reviewed retrospectively. Prostate biopsy was recommended to the patients who had abnormal finding in digital rectal examination or whose serum prostate specific antigen (PSA) level was above 3.0 or 4.0 ng/mL according to the policy for prostate biopsy of each medical center. All the pathologic slides of 18-gauge needle biopsy and the surgical prostate specimen from the involved medical centers were reevaluated by single expert uropathologist. According to the 2005 International Society of Urological Pathology (ISUP) consensus on Gleason grading of prostatic carcinoma (8), bGS was defined as summation of primary GS and highest grade GS of all biopsy cores; and pGS was defined as summation of primary and secondary GS in the prostate specimen. Tumor volume was measured in the whole mount section of the resected prostate by the pathologist. The patients who took neoadjuvant therapy including androgen deprivation or radiation therapy and the patients whose pathological slides showed too poor quality to reevaluate were excluded. Finally 1,446 patients were included in this study. Biochemical failure was defined as serum PSA elevation above 0.2 ng/mL from nadir after radical prostatectomy. Time to biochemical failure was measured by the time interval from radical prostatectomy to biochemical failure. Needle biopsy specimen was taken from 6 (10.9%), 8 (8.4%), 10 (14.8%) and 12 cores (65.8%) and additional cores of suspicious nodules. Clinical stage was classified into cT1, cT2, and cT3 based on digital rectal examination and MRI findings. Operation procedure was included 1,036 radical retropubic prostatectomies (71.6%), 220 radical perineal prostatectomies (15.2%), 125 laparoscopic radical prostatectomies (8.6%) and 65 robot-assisted radical prostatectomies (4.5%). Mean age was 64.9 (38-85) yr old and preoperative sPSA was 11.8 ng/mL. The distribution of bGS was 46.7%, 39.5% and 13.8% in GS ≤ 6, 7, and ≥ 8, respectively (Table 1). According to the difference between bGS and pGS, the patients were divided into three groups: group A (decreased in pGS by 2 or more), group B as a control group (changed in pGS within 1 point), and group C (increased in pGS by 2 or more). We evaluated various clinicopathological factors of prostate cancer, including age, preoperative sPSA, the number of biopsy cores, the highest cancer % in biopsy cores, clinical and pathological stage, volume % and distribution of cancer cells in surgical specimen, and surgical margin status, univariately and multivariately. Hazards for biochemical failure of these groups were also analyzed.
ANOVA and chi-square test was used for analysis of the variables in three groups. Scheffe's method and Dunnett's C method were used for post-hoc test for identifying the groups which made difference. Kaplan-Meier method and log rank test and Cox-regression hazard model were used for analysis of the hazards for biochemical failure of the groups.
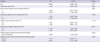
Each group included 30 (2.1%), 1,361 (94.1%) and 55 (3.8%) patients. Group A included bGS 7, 9 and 10 by 26.7%, 70.0%, and 3.3%, respectively, and group C, bGS 4, 5, 6, 7, and 8 by 5.5%, 7.3%, 21.8%, 63.6%, and 1.8% (Table 1). In the comparison of the clinicopathological factors of the three groups, the number of biopsy cores, maximal cancer % in positive cores, clinical and pathological stage, cancer volume %, and surgical margin status were significantly different (Table 2). In group A and C, maximal % of tumor in biopsy cores (P < 0.001 and P = 0.032, respectively) and margin positivity (P = 0.025 and P = 0.002, respectively) were higher than the control group B and pathological T stage was also worse in the group A and C than the control group B (P = 0.006 and P < 0.001, respectively). In group C, the number of biopsy core was significantly lower but tumor volume % in the pathology specimen was significantly higher and tumor was more widely distributed in the prostate specimen than the control group B (P = 0.001), which were different aspects from group A (Table 3). Of the patients in group A, 73.3% diagnosed as prostate cancer of bGS 9 or 10 and their pGS fell into pGS 7 or 8. Though pGS of 8 patients (26.7%) who was diagnosed as bGS 7 was decreased to 5, the pathological stage of 7 of them were pT2c or higher.
Hazard ratio (HR) for biochemical failure was significantly higher in both groups (Group A, HR 2.385, 95% CI [1.222-4.656] P = 0.011; Group C, HR 1.750, 95% CI [1.147-2.672], P = 0.009) (Fig. 1). The median time to biochemical failure in group A and C were 46.0 and 62.6 months respectively but that of the control group did not reach median value within follow-up period. In multivariate analysis, however, this difference of bGS and pGS was not an independent prognostic factor of biochemical recurrence. Well-known prognostic factors of prostate cancer such as pGS (P = 0.045), pT stage (P < 0.001), surgical margin (P = 0.004) were significant in multivariate analysis (Table 4).
It has been noted that there is 20%-40% of discrepancy between bGS and pGS in the pathology of prostate cancer (6, 7, 9). Interestingly, in the univariate analysis, the result of current study demonstrated that the patients with this large difference between GS of pre- and post-prostatectomy showed worse clinicopathological findings and worse prognosis in biochemical failure than the control group irrespective of increase or decrease of the pGS compared with bGS. A similar study to this, in which the patients were classified into three groups, namely, upgraded, downgraded, and unchanged, proposed that GS upgrading was associated with adverse pathological outcome compared with downgraded and unchanged groups, which included higher rates of extraprostatic extension, lymph node metastasis, positive surgical margins, and seminal vesicle invasion (7). Of the patients who showed two or more points decreased in pGS from bGS, 50% was diagnosed as pT3a or higher. Some of them were diagnosed as pGS 5, however, pathological stage of most of them was pT2c or higher. One of the reasons of this discrepancy between bGS and pGS may be sampling error in biopsy of heterogenic and multicentric prostate cancer (10). Prostate cancer which showed uniform pattern histology was reported only 12%-33% in several studies (11). Another reason can be considered as the presence of high grade of tertiary component. Needle biopsy specimen could be obtained mainly in high grade of tertiary component, which would be ignored in prostatectomy specimen. If the biopsy specimen contained small amount of high grade prostate cancer, the pathologists would be tend to diagnose needle biopsy specimen as more aggressive cancer. In a study, analyzing 101 completely sectioned whole-mounted radical prostatectomy samples, the average number of different grades was 2.7 (range 1-5) (12). In an extended study with 155 tumors from 61 whole-mounted radical prostatectomy samples, 15% of tumors included three or more histological grades (13). A recent meta-analysis revealed that the presence of tertiary grade correlated with pathological stage, PSA recurrence and clinical progression (14). In several studies, samples characterized with pathological variables of poor outcome, such as extraprostatic extension and positive surgical margins contained a high grade tertiary component with consistently higher frequency (15, 16). Therefore bGS of the patients in group A rather than pGS may reflect prognosis and should be considered as one of the important prognostic factors together with pathological stage.
The patients who showed two or more points increase in pGS from bGS also demonstrated aggressive tumor burden and poor prognosis in biochemical failure. In these patients, the number of biopsy core was significantly smaller than other groups. A recent study of 301 patients with low-risk prostate cancer (clinical Stage T1c-T2a, PSA ≤ 10 ng/mL, and bGS ≤ 6) who underwent an extended (≥ 10-core) prostate needle biopsy, in men assessed with 10-12 cores, the rate of GS upgrading was 47.9%, which was significantly higher than 23.5% in 18 cores (17). In another study, the authors proposed that prostate size and number of sampling was associated with Gleason upgrading (18). The mean prostate volume of the patients in group C was smaller than that of control group. On the other hand, tumor volume in whole-mount prostate was bigger. Thus insufficient number of prostate sampling, especially in small prostate containing aggressive cancer might cause Gleason upgrading. However, multivariate analysis showed clinical significance not in the difference of bGS and pGS but in well-known prognostic factors of prostate cancer such as sPSA, bGS or pGS itself, pT stage and surgical margin. In the clinical settings, even if both of the clinicians and the patients would be confused with the somewhat large discrepancy in bGS and pGS, it can be ignored compared with other well-known prognostic clinicopathological factors. However, the clinicians had better kept in mind that many of these patients who showed large discrepancy in bGS and pGS might have other unfavorable clinicopathological factors of prostate cancer.
Bias related with interobserver variation in the pathologic result of Gleason score or Gleason sum would be one of major limitation of this kind of study. A considerable interobserver variation in the Gleason scores of prostate cancer referred to several studies has been reported (19, 20). In addition, we did not review the tertiary component of prostate cancer specimen in group A, and survival analysis was not included due to the short follow-up period. Practically, the large Gleason score gap of 2 or more points in bGS and pGS rarely occurs. In the current study, the total number of reviewed patients was 1,582, however, the number of focused patients was very small, which can be addressed as another limit point.
In summary, large difference between bGS and pGS shows poor prognosis even in the decreased group. However it is not an independent prognostic factor for biochemical failure.
Figures and Tables
 | Fig. 1Hazard for biochemical recurrence of the three groups: Group A (decreased in pGS by 2 or more), Group B as a control group (changed in pGS within 1 point), and Group C (increased in pGS by 2 or more). |
AUTHOR SUMMARY
Clinical Significance of a Large Difference (≥ 2 points) between Biopsy and Post-prostatectomy Pathological Gleason Scores in Patients with Prostate Cancer
Changhee Yoo, Cheol Young Oh, Jin Seon Cho, Cheryn Song, Seong Il Seo, Hanjong Ahn, Tae-Kon Hwang, Jun Cheon, Kang Hyun Lee, Tae Gyun Kwon, Tae Young Jung, Moon Kee Chung, Sang Eun Lee, Hyun Moo Lee, Eun Sik Lee, Young Deuk Choi, Byung Ha Chung, Hyung Jin Kim, Wun-Jae Kim, Seok-Soo Byun, and Han Yong Choi
Large difference (≥ 2 points) between biopsy-derived (bGS) and post-prostatectomy Gleason scores (pGS) may confuse the clinicians in consulting the patients with prostate cancer. In the present study, we compared the prognosis of patients with the difference between pGS and bGS. When the pGS was changed from bGS by 2 points or above, such patients showed poor prognosis. Strikingly, even in the decreased group (pGS < bGS) showed poor prognosis. However the large difference between bGS and pGS was not an independent prognostic factor, and one should be cautious in the interpretation of the scoring values.
References
1. Edwards BK, Brown ML, Wingo PA, Howe HL, Ward E, Ries LA, Schrag D, Jamison PM, Jemal A, Wu XC, Friedman C, Harlan L, Warren J, Anderson RN, Pickle LW. Annual report to the nation on the status of cancer, 1975-2002, featuring population-based trends in cancer treatment. J Natl Cancer Inst. 2005. 97:1407–1427.
2. Jung KW, Park S, Kong HJ, Won YJ, Boo YK, Shin HR, Park EC, Lee JS. Cancer statistics in Korea: incidence, mortality and survival in 2006-2007. J Korean Med Sci. 2010. 25:1113–1121.
3. Gleason DF, Mellinger GT. Prediction of prognosis for prostatic adenocarcinoma by combined histological grading and clinical staging. J Urol. 1974. 111:58–64.
4. Lerner SE, Blute ML, Bergstralh EJ, Bostwick DG, Eickholt JT, Zincke H. Analysis of risk factors for progression in patients with pathologically confined prostate cancers after radical retropubic prostatectomy. J Urol. 1996. 156:137–143.
5. Epstein JI, Partin AW, Sauvageot J, Walsh PC. Prediction of progression following radical prostatectomy. A multivariate analysis of 721 men with long-term follow-up. Am J Surg Pathol. 1996. 20:286–292.
6. Smith EB, Frierson HF Jr, Mills SE, Boyd JC, Theodorescu D. Gleason scores of prostate biopsy and radical prostatectomy specimens over the past 10 years: is there evidence for systematic upgrading? Cancer. 2002. 94:2282–2287.
7. Moussa AS, Li J, Soriano M, Klein EA, Dong F, Jones JS. Prostate biopsy clinical and pathological variables that predict significant grading changes in patients with intermediate and high grade prostate cancer. BJU Int. 2009. 103:43–48.
8. Epstein JI, Allsbrook WC Jr, Amin MB, Egevad LL. ISUP Grading Committee. The 2005 International Society of Urological Pathology (ISUP) Consensus Conference of Gleason grading of prostatic carcinoma. Am J Surg Pathol. 2005. 29:1228–1242.
9. Köksal IT, Ozcan F, Kadioglu TC, Esen T, Kiliçaslan I, Tunç M. Discrepancy between Gleason scores of biopsy and radical prostatectomy specimens. Eur Urol. 2000. 37:670–674.
10. Catalona WJ, Stein AJ, Fair WR. Grading errors in prostatic needle biopsies: relation to the accuracy of tumor grade in predicting pelvic lymph node metastases. J Urol. 1982. 127:919–922.
11. Müller HA, Ackermann R, Frohmüller HG. The value of perineal punch biopsy in estimating the histological grade of carcinoma of the prostate. Prostate. 1980. 1:303–309.
12. Aihara M, Wheeler TM, Ohori M, Scardino PT. Heterogeneity of prostate cancer in radical prostatectomy specimens. Urology. 1994. 43:60–66.
13. Ruijter ET, van de Kaa CA, Schalken JA, Debruyne FM, Ruiter DJ. Histological grade heterogeneity in multifocal prostate cancer. Biological and clinical implications. J Pathol. 1996. 180:295–299.
14. Harnden P, Shelley MD, Coles B, Staffurth J, Mason MD. Should the Gleason grading system for prostate cancer be modified to account for high-grade tertiary components? A systematic review and meta-analysis. Lancet Oncol. 2007. 8:411–419.
15. Mosse CA, Magi-Galluzzi C, Tsuzuki T, Epstein JI. The prognostic significance of tertiary Gleason pattern 5 in radical prostatectomy specimens. Am J Surg Pathol. 2004. 28:394–398.
16. van Oort IM, Schout BM, Kiemeney LA, Hulsbergen CA, Witjes JA. Does the tertiary Gleason pattern influence the PSA progression-free interval after retropubic radical prostatectomy for organ confined prostate cancer? Eur Urol. 2005. 48:572–576.
17. Capitanio U, Karakiewicz PI, Valiquette L, Perrotte P, Jeldres C, Briganti A, Gallina A, Suardi N, Cestari A, Guazzoni G, Salonia A, Montorsi F. Biopsy core number represents one of foremost predictors of clinically significant Gleason sum upgrading in patients with low-risk prostate cancer. Urology. 2009. 73:1087–1091.
18. Turley RS, Terris MK, Kane CJ, Aronson WJ, Presti JC Jr, Amling CL, Freedland SJ. SEARCH Database Study Group. The association between prostate size and Gleason score upgrading depends on the number of biopsy cores obtained: results from the Shared Equal Access Regional Cancer Hospital Database. BJU Int. 2008. 102:1074–1079.
19. Allsbrook WC Jr, Mangold KA, Johnson MH, Lane RB, Lane CG, Epstein JI. Interobserver reproducibility of Gleason grading of prostatic carcinoma: general pathologist. Hum Pathol. 2001. 32:81–88.
20. McLean M, Srigley J, Banerjee D, Warde P, Hao Y. Interobserver variation in prostate cancer Gleason scoring: are there implications for the design of clinical trials and treatment strategies? Clin Oncol (R Coll Radiol). 1997. 9:222–225.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download