Abstract
With regard to the outcome of intensive neonatal care, one of the most important concerns in neonatology is the mortality rate of very low birth weight infants (VLBWI; birth weight < 1,500 g) and extremely low birth weight infants (ELBWI; birth weight < 1,000 g). The present study was conducted to analyze and compare the mortality of VLBWI and ELBWI and neonatal care among Korean, Japanese, and American newborns. In Korea, the survival rates of VLBWI have increased significantly; they were 31.8% in the early 1960s, 65.8% in the early 1990s, 77.5% in 2002, 84.7% in 2007, and 85.7% in 2009. The survival rates of ELBWI have also increased; they were 8.2% in the early 1960s, 37.4% in the early 1990s, 56.1% in 2002, 67.7% in 2007, and 71.8% in 2009. The survival rates of VLBWI and ELBWI have significantly improved over the past 50 yr in Korea. However, the Korean survival rates of VLBWI and ELBWI are still lower than for similar groups in Japan and the USA. To achieve better outcomes that reach the level of these countries, the organization of perinatal care centers, nationwide neonatal perinatal research networks, and regionalization are needed in Korea.
In Korea, the first nursery was built during the 1960s. Special care of premature babies was started in the 1970s and the neonatal intensive care unit (NICU) was established during the early 1980s. The development of neonatology has been reflected in the significant improvement in the survival of low birth weight infants (LBWI) over the past 50 yr in Korea (1-3).
With regard to intensive neonatal care, the mortality rate of very low birth weight infants (VLBWI; birth weight < 1,500 g) and extremely low birth weight infants (ELBWI; birth weight < 1,000 g) is a very important indicator associated with patient care. Among premature babies, the VLBWIs require more intensive care. Recently, the survival rates of ELBWI and VLBWI have significantly improved along with the improvement of neonatal intensive care in Korea.
There have been four reports on the mortality of LBWI, VLBWI, and ELBWI based on a nationwide survey of Korean NICUs; in 1996 (4), 2002 (5), 2007 (6), and 2009 (7). In addition to these nationwide surveys, regional hospitals and single hospital reports in the 2000s were also included (8-15). In Japan and the USA, the mortality of these preterm infants and quality control associated with their care has been reported by studies conducted by neonatal and perinatal multicenter networks (16-25).
The goal of the present study was to analyze the mortality of VLBWI and ELBWI in the 2000s in Korea, and compare the findings to similar data from Japan and the USA. In addition, suggestions of how to improve the outcome of neonatal care in Korea were discussed.
Korean mortality data on VLBWI and ELBWI between the 1960s and 1990s were collected from the reports of Bae and Bae (1), Kim and Bae (2), and Bae (3). In the 2000s, a Korean nationwide survey was reported three times. In the first report, Park et al. (5) studied the survival rate of neonates among 1,842 live births of VLBWI and 592 live births of ELBWI from 62 hospitals in 2002. The second study, reported by Hahn et al. included 2,030 live births of VLBWI and 711 live birth of ELBWI from 57 hospitals in 2007 (6). For these two reports, the survival rates of neonates were defined as neonates that survived over 28 days. The third was a report by Chang and the Committee on Statistics of the Korean Society of Neonatology (7). In this study, 2,587 VLBWIs and 910 ELBWIs, from 82 hospitals in 2009, were included and the survival rate of the neonates was defined as neonates that survived to the time of discharge from NICU. In addition to these nationwide surveys, regional hospitals and single hospital reports of survival rate at time of discharge from NICU in the 2000s were also included (8-15).
The data on survival from Japan in 2000 was collected from the report of the Committee of Neonatal Medicine, of the Japanese Society of Pediatrics (16). The data from the Japanese nationwide NICU network, Neonatal Research Network (17) and the Perinatal Care Center Network (3,170 VLBWIs from 75 NICUs in 2008) (18) was used as well. The recent reports of Kusuda et al. (19) and Itabashi et al. (20) provided the mortality rates for VLBWIs and ELBWIs from two Japanese networks.
The data from the USA was collected by the nationwide networks for neonatal care; the Vermont Oxford Network (21) and National Institute of Child Health and Human Development (NICHD) Neonatal Research Network (22). Two recent reports by Payne et al. (23) based on the Vermont Oxford Network, and Fanaroff et al. (24) based on the NICHD Neonatal Research Network were also analyzed. Even though there was a recent report by Stoll et al. (25) that described in detail the mortality and morbidity data of preterm babies based on gestational age, from the NICHD Neonatal Research Network, data from that study was not used. The present study was performed to analyze mortality according to birth weight.
Using the data collected from the above reports, changes in the survival and mortality of VLBWI and ELBWI among the three countries was compared, e.g., Korea, Japan, and the USA.
As shown in Fig. 1A, the mortality rates of VLBWI were 68.2% and 63.7% in the early and late 1970s. These rates have fallen over the last 40 yr to 55.8% and 57.6% in the 1970s, to 56.2% and 48.1% in the 1980s, and to 33.5% and 24.5% in the 1990s. The changes in the mortality rate of LBWI and VLBWI by 10-yr intervals are shown in Fig. 1B. The mortality rates of LBWI were 23.4% in the 1960s, 17.0% in the 1970s, 14.2% in the 1980s, and 8.1% in the 1990s. For VLBWI the mortality rates were 66.2% (survival rate 33.8%) in the 1960s, 56.8% (survival rate 43.2%) in the 1970s, 50.8% (survival rate 49.2%) in the 1980s, and 32.9% in the 1990s. The mortality rates have fallen quite dramatically over the last 40 yr (1).
The Korean nationwide survey on the survival rates of VLBWI and ELBWI in the 2000s are summarized in Table 1, which included data reported by Park et al. (5), Hahn et al. (6), and Chang and the Committee on Statistics of the Korean Society of Neonatology (7). The survival rates of VLBWI have continued to increase; 77.5% in 2002, 84.7% in 2007, and 85.7% in 2009. The ELBWI also showed improving survival rates; 56.1% in 2002, 67.7% in 2007, and 71.8% in 2009.
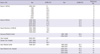
There were several reports from NICUs of regional hospitals and a single hospital in Korea in the 2000s; the survival rates of VLBWI and ELBWI from seven hospitals (9) and eight hospitals (15) in Busan, from four hospitals in Seoul and Buchoen (8), and from some reports from a single hospital (10-14) are summarized in Table 2. The VLBWIs showed survival rates from 52% to 92% and the ELBWI showed survival rates from 26% to 85%. There were some differences in survival rates among centers and by region; some large scale NICUs showed better survival rates.
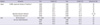
The survival rates have improved significantly in the 2000s in Japan and the USA; VLBWI, 92.0% in 2003 (19), 92.0% in 2008 (18) in Japan and 92.6% in 2006 (24) in the USA; ELBWI, 87.0% in 2005 (20), 85.5% in 2008 (18) in Japan and 85.0% in 2006 in the USA (24). These findings show better outcomes compared to the Korean results. The changes in survival rates of VLBWI and ELBWI in Japan and the USA are summarized in Table 3 and the recent data is compared among the three countries in Fig. 3.
The history of neonatology in Korea started with the first lecture on neonatology at the Seoul National University College of Medicine in 1954. Special neonatal care was established in the 1960s and units for the care of premature babies were set up in the 1970s, as incubators were introduced. During the 1980s, specialized incubators and mechanical ventilation became available in Korea, and the care for high-risk neonates became possible. The introduction of artificial pulmonary surfactant therapy (26) and high frequency ventilators in the 1990s, was associated with significant improvement in the survival of premature babies. During the 2000s, several institutional developments have been implemented to improve neonatal outcomes (3).
As shown in the results of this study, the survival rates of VLBWI increased from 33.8% in the 1960s, to 43.2% in the 1970s, to 49.2% in the 1980s, to 67.1% in the 1990s. This improving tendency further continued throughout the 2000s to 77.5% in 2002, 84.7% in 2007, and 85.7% in 2009. The survival rates of ELBWI were similar but showed a more significant increase; 8% in the early 1960s to 37.4% in the early 1990s, to 56.1% in 2002, 67.7% in 2007, and 71.8% in 2009.
However, the comparison of outcomes of premature babies among the three countries: Korea (2009), Japan (2003, 2005, and 2008), and the USA (2006) show a lower survival rate in the Korean VLBWIs and ELBWIs (Fig. 3). The survival rates were 85.7%, 92.0%, and 92.6% (VLBWI) and 71.8%, 87.0%, and 85.0% (ELBWI) in Korea, Japan, and the USA in the 2000s, respectively.
In Japan, neonatology was established as a specialty earlier than in Korea. Special medical care for premature babies was started in 1958 and supported by the government. The national action of supporting medical instruments for perinatal care and the regionalization of perinatal medicine were introduced in 1979. Starting in 1984, national support for maternal-fetal intensive care units was started and additional support for the medical expenses needed for perinatal medicine was achieved in 1986. These national projects continued to develop and include the organization of the Tertiary Central Perinatal Care Centers and Secondary Regional Perinatal Care Centers in 1996 (27). This system regionalized perinatal and neonatal care and built an effective management system for the care of high-risk pregnancies and neonates. The highest survival rates and the lowest mortality rates for VLBWI and ELBWI throughout the world could be achieved with this perinatal care system. One of the most useful institutional approaches seems to be the regionalization of perinatal medicine and organization of perinatal care centers in Korea (28).
In addition, the patient information network is an important feature. The Japanese nationwide "Neonatal Research Network" was introduced in 1999 (17). Another network, the "Perinatal Care Center Network" was started in 2003 (18). These two networks include all NICUs in Japan and they have very excelent functions. Data on all patients were registered in this system, and the results of the data analysis published and shared between all centers. Moreover, these data were used for quality control of medical management in NICUs; e.g., a NICU with poor outcome data is managed by the network center to improve outcomes. Kusuda et al. (19) reported the necessity of quality control for the standardization of NICU management. Among 37 level III NICUs registered in the Neonatal Research Network, in 2003, the mortality of VLBWI had a very wide gap among NICUs and the differences were statistically significant; low mortality, 4.8% in 11 NICUs; moderate mortality, 11.0% in 12 NICUs; and high mortality, 17.1% in 14 NICUs. However, evaluation study in neonatal mortality has not been done between NICUs in Korea; the details related to neonatal mortality during 2009 will be reported in the future.
In the USA, the nationwide networks, the Vermont Oxford Network started in 1988 (21) and the NICHD Neonatal Research Network started in 1986 (22), analyzed the morbidity and mortality of neonates and clinical study results, and proposed evidence based medical guidelines for the practice of neonatology. In addition, reports on quality control and improvement in the care obtained in NICUs as well as regionalization of perinatal medicine have been included in the reports (29-32). Such systematic data collection has significantly contributed to the development of neonatology and the organization of nationwide networks; this model might improve outcomes if adoped in Korea.
Table 4 shows the history of major developments and the degree of institutional organization of neonatal and perinatal medicine in Korea, Japan (33) and the USA. Compared to Japan and the USA, the aspects of Korean neonatal care that require future attention include: regionalization of neonatal medicine, development and implementation of maternal transfer systems, organization of perinatal care centers, bed expansion in NICUs, support systems for disabled infants, and the organization of nationwide neonatal, perinatal research networks etc.
The survival rates of VLBWI and ELBWI have significantly improved over the past 50 yr and have been very impressive in Korea in the 2000s. However, the survival rates of VLBWI and ELBWI are still lower in Korea than in Japan and the USA. To achieve better outcomes in Korea, the organization of perinatal care centers, nationwide neonatal and perinatal research networks, and regionalization of neonatal and perinatal medicine are needed.
Figures and Tables
Fig. 1
Changes in the neonatal mortality of low birth weight infants (LBWI) and very low birth weight infants (VLBWI) in Korea by 5-yr intervals (A) and 10-yr intervals (B). F, first half of the decade; S, second half of the decade (Quotation from reference 1 after permission).

Fig. 2
Changes in the survival rates for very low birth weight infants (VLBWI) and extremely low birth weight infants (ELBWI) in Korea. F, first half of the decade; S, second half of the decade (Quotation from reference 2 after permission).

Fig. 3
Comparison of recent survival rates for very low birth weight infants (VLBWI) and extremely low birth weight infants (ELBWI) in Korea, Japan and the USA. *Neonatal survival rate within 28 days after births; †Neonatal survival rate at time of discharge from NICU.

Table 1
Survival rates of very low birth weight infant (VLBWI) and extremely low birth weight infant (ELBWI) in the Korea in 2000s by the Korean the nationwide surveys
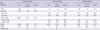
Table 2
Survival rates at discharge from neonatal intensive care units of very low birth weight infants (VLBWI) and extremely low birth weight infants (ELBWI) in regional hospitals and single hospital in Korea
AUTHOR SUMMARY
Recent Trends in Neonatal Mortality in Very Low Birth Weight Korean Infants: In Comparison with Japan and the USA
Won-Ho Hahn, Ji-Young Chang, Yun Sil Chang, Kye Shik Shim, and Chong-Woo Bae
Owing to the recent development of intensive neonatal care, survival rates of very low birth weight infants (VLBWI; birth weight < 1,500 g) and extremely low birth weight infants (ELBWI; birth weight < 1,000 g) is greatly improved. Here we analyze and compare the mortality of VLBWI and ELBWI among Korean, Japanese, and American newborns. The survival rates of VLBWI and ELBWI have significantly improved over the past 50 yr in Korea while still lower than the similar groups in Japan and USA. To achieve better outcomes in Korea, the organization of perinatal care centers, nationwide neonatal perinatal research networks, and regionalization are requested.
References
1. Bae YM, Bae CW. The changes in the mortality rates of low birth weight infant and very low birth weight infant in Korea over the past 40 years. J Korean Med Sci. 2004. 19:27–31.
2. Kim KS, Bae CW. Trends in survival rate for very low birth weight infants and extremely low birth weight infants in Korea, 1967-2007. Korean J Pediatr. 2008. 51:237–242.
3. Bae CW. The changes in the birth and mortality rates of newborn in Korea. J Korean Med Assoc. 2006. 49:975–982.
4. Bae CW, Kim MH, Chun CS, Lee C, Moon SJ, Yoo BH, Lim BK, Lee SG, Choi YY, Byun SH, Choi AH, Pi SY, Han DG, Yun CK. Neonatal statistics of Korea in 1996: collective results of live-births, neonatal mortality, and incidence of discharge against medical advice at 64 hospitals. J Korean Soc Neonatol. 1997. 4:153–169.
5. Park DK, Kil CH, Bae CW. Neonatal statistics of Korea in 2002: collective results of live-births and neonatal mortality rates from 62 hospitals. J Korean Soc Neonatol. 2004. 11:122–129.
6. Hahn WH, Chang JY, Bae CW. Birth statistics and mortality rates for neonatal intensive care units in Korea during 2007: collective results from 57 hospitals. J Korean Soc Neonatol. 2009. 16:36–47.
7. Chang YS. The Committee on Statistics of the Korean Society of Neonatology. The survey on the actual conditions of neonatal intensive care units and analysis of survival rate of high-risk newborn infants. 2010 Report Management Center for Health Promotion. 2010.
8. Kim SS, Kim MH, Shin JW, Ko SY, Lee EK, Chang YS, Kang IS, Park WS, Lee MH, Lee SI, Lee HJ. Changes in the outcomes of very low birth weight infants. J Korean Pediatr Soc. 2002. 45:828–835.
9. Kim BJ, Lee YA, Park SE, Sinn JB, Kim SM, Hong SY, Seo SS, Byun SO. Mortality and morbidity of very low birth weight infants in Busan area during recent 6 years. J Korean Soc Neonatol. 2003. 10:143–152.
10. Ma TH, Lee YK, Kim KA, Ko SY, Kim MJ, Shin SM. Outcome of very low birth weight infants in past 2 years at Samsung Cheil Hospital. J Korean Soc Neonatol. 2003. 10:7–13.
11. Kim JT, Park HK, Jun NL, Lim JW, Kim EA, Kim KS, Pi SY. Recent outcome of extremely low birth weight infants at Asan Medical Center. J Korean Soc Neonatol. 2003. 10:133–142.
12. Cho JJ, Lee SB, Park WS, Chang YP. Survival rate in very low birth weight infants. Korean J Pediatr. 2004. 47:505–509.
13. Park SE, Jeon GW, Choi CW, Hwang JH, Koo SH, Kim YJ, Lee CH, Chang YS, Park WS. Evaluation of perinatal and management factors associated with improved survival in extremely low birth weight infants. Korean J Pediatr. 2005. 48:1324–1329.
14. Kim DH, Shim SY, Kim JR, Shin SH, Kim ES, Joung KE, Kim SD, Lee JA, Choi CW, Kim EK, Kim HS, Kim BI, Choi JH. Recent outcome of extremely low birth weight infants: the use of CRIB(clinical risk index for babies) II score for analyzing the survival rate. Korean J Pediatr. 2006. 49:952–958.
15. Wang SW, Lee YA, Park SE, Shin JB, Hong YR, Park JJ, Lee JA, Son SH, Byun SO, Kim JP. Changes in the outcomes of very low birth weight infants in Busan area. J Korean Soc Neonatol. 2007. 14:206–214.
16. Horiuchi T, Ohno T, Itani Y, Kabe K, Nakamura T, Nakamura H. Studies on the states of care for high risk neonates and neonatal mortality in our country (year 2000). J Jpn Pediatr Soc. 2002. 106:603–613.
17. Neonatal Research Network, Japan. accessed on 20 Dec 2010. Available at http://nrn.shiga-med.ac.jp.
18. Perinatal Care Center Network, Japan. accessed on 20 Dec 2010. Available at http://plaza.umin.ac.jp/nrndata/syukei.htm.
19. Kusuda S, Fujimura M, Sakuma I, Aotani H, Kabe K, Itani Y, Ichiba H, Matsunami K, Nishida H. Neonatal Research Network, Japan. Morbidity and mortality of infants with very low birth weight in Japan: center variation. Pediatrics. 2006. 118:e1130–e1138.
20. Itabashi K, Horiuchi T, Kusuda S, Kabe K, Itani Y, Nakamura T, Fujimura M, Matsuo M. Mortality rates for extremely low birth weight infants born in Japan in 2005. Pediatrics. 2009. 123:445–450.
21. Vermont Oxford Network. accessed on 20 Dec 2010. Available at http://www.vtoxford.org.
22. National Institute of Child Health and Human Development (NICHD) Neonatal Research Network. accessed on 20 Dec 2010. Available at https://neonatal.rti.org.
23. Payne NR, Finkelstein MJ, Liu M, Kaempf JW, Sharek PJ, Olsen S. NICU practices and outcomes associated with 9 years of quality improvement collaboratives. Pediatrics. 2010. 125:437–446.
24. Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR, Bauer CR, Donovan EF, Korones SB, Laptook AR, Lemons JA, Oh W, Papile LA, Shankaran S, Stevenson DK, Tyson JE, Poole WK. NICHD Neonatal Research Network. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol. 2007. 196:147.
25. Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, Hale EC, Newman NS, Schibler K, Carlo WA, Kennedy KA, Poindexter BB, Finer NN, Ehrenkranz RA, Duara S, Sánchez PJ, O'Shea TM, Goldberg RN, Van Meurs KP, Faix RG, Phelps DL, Frantz ID 3rd, Watterberg KL, Saha S, Das A, Higgins RD. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010. 126:443–456.
26. Bae CW, Hahn WH. Surfactant therapy for neonatal respiratory distress syndrome: a review of Korean experiences over 17 years. J Korean Med Sci. 2009. 24:1110–1118.
27. Japan Perinatal Care Center. accessed on 20 Dec 2010. Available at http://nrn.shiga-med.ac.jp.
28. Bae CW. Bench-marking of Japanese Perinatal Center System for improving maternal and neonatal outcome in Korea. Korean J Perinatol. 2010. 21:129–139.
29. Iams JD, Romero R, Culhane JF, Goldenberg RL. Primary, secondary, and tertiary interventions to reduce the morbidity and mortality of preterm birth. Lancet. 2008. 371:164–175.
30. Lasswell SM, Barfield WD, Rochat RW, Blackmon L. Perinatal regionalization for very low-birth-weight and very preterm infants: a meta-analysis. JAMA. 2010. 304:992–1000.
31. Horbar JD, Soll RF, Edwards WH. The Vermont Oxford Network: a community of practice. Clin Perinatol. 2010. 37:29–47.
32. NICHD Neonatal Research Network. Report to the NACHHD Council September 2008. accessed on 20 Dec 2010. Available at http://www.jaog.or.jp/japanese/jigyo/JYOSEI/center.htm.
33. Igarashi T, Watanabe T. Neonatal medicine. 2010. 1st ed. Tokyo: Nakayama Shoten Co., Ltd;2–5.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download