Abstract
Endovascular repair of inflammatory aortic aneurysms has been reported as an alternative to open surgical treatment. In selective cases, adjunctive bypass surgery may be required to provide an adequate landing zone. We report a case of endovascular repair of an inflammatory aortic aneurysm in a patient with Behçet's disease using a carotid-carotid bypass graft to provide an adequate landing zone. A 45-yr-old man with a voice change was referred to our hospital with the diagnosis of saccular aneurysm of the distal aortic arch resulting from vasculitis. Computed tomography showed a thoracic aortic aneurysm with thrombosis. Right to left carotid-carotid bypass grafting was performed. After 8 days, the patient underwent an endovascular stent graft placement distal to the origin of the innominate artery. The patient was discharged with medication and without postoperative complications after 5 days. Hybrid endovascular treatment may be suitable a complementary modality for repairing inflammatory aortic aneurysms.
Endovascular repair of aortic disease has recently gained popularity because it offers greater safety and patient tolerance than open surgical repair. This technique is less invasive and correlates with low morbidity and mortality (1). Endovascular rather than open repair may more appropriate for high-risk patients such as those suffering from inflammatory aortic aneurysms, which have an operative mortality three times higher than that of non-inflammatory aneurysms due to technical complications caused by inflammation and periaortic fibrosis (2). In cases of aortic arch pathologies, which often involve the origin of the supra-aortic branches, it may be necessary to cover the origin of the supra-aortic branches using an endovascular stent graft to extend the proximal landing zone. To reduce the risk of neurologic and vascular complications, adjunctive open surgical bypass surgery may be required to provide an adequate landing zone. This is a case report of carotid-carotid bypass grafting, followed by coverage of the aortic arch with an endovascular stent graft in a patient with an inflammatory aortic aneurysm.
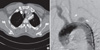
A 45-yr-old man with hoarseness of voice was referred to our hospital with the diagnosis of a distal aortic arch aneurysm due to vasculitis in May 2008. He presented recurrent oral aphthous ulcer and eythemanodosun-like skin eruption, and hyperirritability of skin. Serum erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were elevated (78 mm/hr and 1.5 mg/dL, respectively). A computed tomography (CT) scan was performed and confirmed a thoracic aortic aneurysm with thrombosis and a maximal diameter of 43 mm (Fig. 1). This aneurysm originated in the left subclavian artery with saccular features. The patient was administered immunosuppressive treatment with oral prednisone (40 mg/day) for 4 weeks due to vascular Behçet's disease until the ESR and CRP values were within the normal range. The patient declined a conventional, open surgical treatment and strongly requested a less invasive treatment. As the aneurysm was close to the left common carotid artery, adjunctive surgical bypass grafting was needed to provide an adequate landing zone for an endovascular repair. Once the inflammatory markers normalized, right to left carotid-carotid bypass grafting and endoluminal stent graft insertion was planned. To evaluate the neck- and intracranial vessels, magnetic resonance angiography was performed. The carotid bifurcation and intracranial vessels were patent, but the left subclavian artery was obstructed and the left vertebral artery was stenotic and hypoplastic.
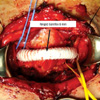
Under general endotracheal anesthesia, a horizontal skin incision was made on 2 cm superior to the sternal notch. A subplastymal muscle flap was made, the bilateral sternothyroid and sternohyoid muscles were divided transversely, and the bilateral carotid sheaths were exposed. After exposure of bilateral common carotid arteries, the right common carotid-left common carotid bypass graft was constructed with an anterior route, in an end-to-side fashion using a ringed Gore-Tex 8 mm graft (W.L. Gore and Associates, AZ, USA) (Fig. 2). There was no change of regional cerebral oxygen saturation during carotid artery clamping according to cerebral oximetry monitoring. The patient was transferred to the intensive care unit after surgery, and then to the general surgical ward on postoperative day 1. He had no clinical evidence of a stroke or vascular complications. Eight days after surgery, the patient underwent endoluminal stent graft placement with a thoracic SEAL stent graft 32 × 100 mm (S&G biotech, Seoul, Korea) just distal to the origin of the innominate artery. The left common carotid artery was occluded with an Amplatzer vascular plug (14 mm; AGA medical, MN, USA) prior to stent graft insertion. There were neither neurologic nor vascular complications. The patient was discharged with medication, 5 days after the second procedure. A CT scan was performed 4 weeks later, showing successful exclusion of the aortic aneurysm without any evidence of leakage (Fig. 3). The patient was treated with steroids due to vascular Behçet's disease. After 3 months, the patient had complete resolution of hoarseness. A CT scan performed after 24 months showed that the carotid-carotid bypass graft was patent and the previous aneurysm was nearly occluded.
Since the first successful endovascular thoracic aortic aneurysm repair, performed by Dake and colleagues in 1994 (3), endovascular repair has evolved into a valuable treatment for thoracic aortic aneurysm. In a metaanalysis of perioperative results, the mortality and incidence of major neurological injury were significantly lower with endovascular repair than with open surgery (4). In addition, surgical treatment of inflammatory aortic aneurysms in the setting of Behçet's disease led to recurrent false aneurysms at the anastomotic site in 30%-50% of cases (5). Endovascular repair of inflammatory aortic aneurysms has been used as an alternative to open surgical repair and seems to provoke less of a cytokine release and inflammatory response (6). The endovascular procedure-related and follow-up mortality were 0% and 13.0%, respectively (7). In addition, this procedure excludes the aneurysm and can reduce the size of the aneurismal sac and the extent of periaortic fibrosis with acceptable long-term morbidity (8). Despite these results, anatomic suitability is necessary, particularly with regard to an adequate landing zone. For an aneurysm involving the supra-aortic branches, an adequate landing zone may be created by using a combined surgical bypass graft (9). In this case, we have performed a carotidcarotid bypass that covered the origin of the left common carotid and left subclavian arteries, in order to obtain adequate proximal anchorage of the stent graft in zone 1. A theoretic concern with using a carotid artery as a donor is the possibility of decreased flow to its own distal vascular bed. Aortic arch branches without significant proximal disease have been used as donor arteries without the threat of steal, with greatly increased blood flow supplying more than one distal vascular bed (10). Carotidcarotid bypass grafts have high flow rates and are relatively short and well protected from injury due to the position of the graft deep in the neck (11). Abou-Zamzam et al. (12) reported a patency rate as high as 90% over 5 yr for extrathoracic grafts performed due to carotid artery obstructive disease; in carotid-carotid cross over, the patency rates was 88% at 3 yr and stroke-free survival was 94% at 4 yr (13).
Recurrence of aneurysm after repair is a major problem and is difficult to avoid completely in Behçet disease (14). To suppress vasculitis and prevent recurrent aneurysm after stent implantation, immunosuppressive and anti-inflammatory medication should be maintained.
Endovascular treatment may be suitable as a complementary treatment of inflammatory aortic aneurysm in a patient with Behçet's disease. When performing an endovascular repair of aortic aneurysms involving zone 1, a right common carotid-left common carotid bypass graft can be used as an adjunctive surgical procedure to provide an adequate landing zone.
Figures and Tables
Fig. 1
Preoperative computed tomography and aortogram. (A) Computed tomography scan shows a saccular aneurysm on the distal aortic arch. (B) An aortogram shows obstruction of the left subclavian artery.
References
1. Schoder M, Grabenwöger M, Hölzenbein T, Cejna M, Ehrlich MP, Rand T, Stadler A, Czerny M, Domenig CM, Loewe C, Lammer J. Endovascular repair of the thoracic aorta necessitating anchoring of the stent graft across the arch vessels. J Thorac Cardiovasc Surg. 2006. 131:380–387.
2. Pennell RC, Hollier LH, Lie JT, Bernatz PE, Joyce JW, Pairolero PC, Cherry KJ, Hallett JW. Inflammatory abdominal aortic aneurysm: a thirty-year review. J Vasc Surg. 1985. 2:859–869.
3. Dake MD, Miller DC, Semba CP, Mitchell RS, Walker PJ, Liddell RP. Transluminal placement of endovascular stent-grafts for the treatment of descending thoracic aortic aneurysms. N Engl J Med. 1994. 331:1729–1734.
4. Walsh SR, Tang TY, Sadat U, Naik J, Gaunt ME, Boyle JR, Hayes PD, Varty K. Endovascular stenting versus open surgery for thoracic aortic disease: systematic review and meta-analysis of perioperative results. J Vasc Surg. 2008. 47:1094–1098.
5. Vasseur MA, Haulon S, Beregi JP, Le Tourneau T, Prat A, Warembourgh H. Endovascular treatment of abdominal aneurysmal aortitis in Behçet's disease. J Vasc Surg. 1998. 27:974–976.
6. Swartbol P, Truedsson L, Norgren L. The inflammatory response and it's consequence for the clinical outcome following aortic aneurysm repair. Eur J Vasc Endovasc Surg. 2001. 21:393–400.
7. Puchner S, Bucek RA, Rand T, Schoder M, Hölzenbein T, Kretschmer G, Reiter M, Lammer J. Endovascular therapy of inflammatory aortic aneurysms: a meta-analysis. J Endovasc Ther. 2005. 12:560–567.
8. Puchner S, Bucek RA, Loewe C, Hoelzenbein T, Kretschmer G, Reiter M, Lammer J. Endovascular repair of inflammatory aortic aneurysms: long-term results. AJR Am J Roentgenol. 2006. 186:1144–1147.
9. Ryu YG, Choo SJ, Lim JY, Yoon HK, Chung CH. Hybrid procedure for a traumatic aortic rupture consisting of endovascular repair and minimally invasive arch vessel transposition without sternotomy. J Korean Med Sci. 2010. 25:142–144.
10. Mitchell RS, Ishimaru S, Ehrlich MP, Iwase T, Lauterjung L, Shimono T, Fattori R, Yutani C. First international summit on thoracic aortic endografting: roundtable on thoracic aortic dissection as an indication for endografting. J Endovasc Ther. 2002. 9:Suppl 2. II98–II105.
11. Ozsvath KJ, Roddy SP, Darling RC 3rd, Byrne J, Kreienberg PB, Choi D, Paty PS, Chang BB, Mehta M, Shah DM. Carotid-carotid crossover bypass: is it a durable procedure? J Vasc Surg. 2003. 37:582–585.
12. Abou-Zamzam AM Jr, Moneta GL, Edwards JM, Yeager RA, McConnell DB, Taylor LM Jr, Porter JM. Extrathoracic arterial grafts performed for carotid artery occlusive disease not amenable to endarterectomy. Arch Surg. 1999. 134:952–957.
13. Manart FD, Kempczinski RF. The carotid-carotid bypass graft. Arch Surg. 1980. 115:669–671.
14. Liu CW, Ye W, Liu B, Wu W, Dake MD. Endovascular treatment of aortic pseudoaneurysm in Behçet disease. J Vasc Surg. 2009. 50:1025–1030.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download