Abstract
We evaluated the long-term results of feminizing genital reconstruction in patients with genital ambiguity with high vaginal confluence. The medical records of 10 consecutive patients with ambiguous genitalia and high vaginal confluence who underwent feminizing genital reconstruction from 1996 to 2007 were reviewed. Seven patients had congenital adrenal hyperplasia, one had mixed gonadal dysgenesis, one had partial androgen insensitivity, and one had 5-alpha reductase deficiency syndrome. Median age at operation was 21 months (range, 2-47 months). Median follow up was 7.7 yr. Of the six patients who underwent feminizing genital reconstruction with the Gonzalez method, three had good results. Of the other three patients, one had a urethrovaginal fistula and underwent fistula repair 9 yr after, one had distal vaginal stenosis and underwent revision vaginoplasty 9 yr after, and one had a urethrovaginal fistula and urethral stricture. The patient with urogenital mobilization had persistent urogenital sinus. Feminizing genitoplasty using the Gonzalez method showed good long-term results in patients with ambiguous genitalia and Congenital adrenal hyperplasia. The procedure is less invasive than other approaches and results in excellent cosmetic outcomes; and complications can be corrected by relatively simple procedures.
Ambiguous genitalia with high vaginal confluence are rare congenital anomalies, observed in only about 5% of patients with congenital adrenal hyperplasia (CAH) (1). The majority of children who undergo surgery for intersex or urogenital sinus conditions have a low vaginal confluence amenable to flap vaginoplasty. The management of children with ambiguous genitalia is an ongoing challenge to the pediatric urologist. Several methods of feminizing genitoplasties are available to treat children with these anomalies including the Passerini-Glazel method, which uses the urogenital sinus and the prepuce to create a tubular flap anastomosed to the proximal vagina, and the Gonzalez-Fernandes method which uses the preputial flap and total urogenital mobilization (2-5). Children treated with these new techniques tend to have short follow-up and the evaluation of their results is subjective. A few recent reports have included long-term follow-up of medical and surgical treatment of CAH, but the various surgical methods have given different results (6, 7). Little is known about the long-term outcomes of the Gonzalez method in patients with ambiguous genitalia and high vaginal confluence. In Korea, there were only 3 reports about feminizing genitoplasty including 2 case reports and 1 short-term result (8-10). We retrospectively evaluated the long-term results of feminizing genitoplasty, especially the Gonzalez method for CAH, in patients with genital ambiguity and high vaginal confluence in Korea.
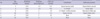
Between 1996 and 2007, 36 patients underwent female surgery for ambiguous genitalia in our center (Table 1). Of these ten had high vaginal confluence including seven with CAH, one with mixed gonadal dysgenesis (MGD), one with partial androgen deficiency, and one with 5-alpha reductase deficiency syndrome.
Preoperative work-up included history taking, discussions of gender identity, physical examination and ultrasonography. Magnetic resonance imaging was performed only if it required. Gender identity was decided to the female in all patients according to the genital appearance, internal organs, hormonal studies including stimulation test, chromosome study, parents' decision, etc. Among them, penile size was considered as most important factor in our institution. Each patient underwent genitography and endoscopy under general anesthesia in one session just prior to the corrective operation to determine the type of high or low vaginal confluence.
Median patient age at the time of surgery was 21.0 months (range, 2-47 months). Six patients with CAH underwent feminizing genital reconstruction using the Gonzalez method (five single stage, one second stage), and one patient with CAH underwent urogenital mobilization. Three patients, one each with MGD, partial androgen insensitivity, and one 5-alpha reductase deficiency syndrome, underwent clitoral reduction only, with delayed vaginoplasty planned as adolescence (Table 2). The median follow-up was 7.7 yr (range, 0.3-12.1 yr).
The patient was placed in the lithotomy position for the best exposure of the perineum. The abdomen and perineum were prepared and the perineum was draped in a sterile field. Initial genitography and endoscopy was used to determine the high or low type of vaginal confluence (Table 1) and the type of operation. In patients with high vaginal confluence, an inverted U-shaped cutaneous flap of skin and subcutaneous tissue was created for the distal portion of the future posterior vaginal wall after indwelling Foley catheter. A circumferential incision was made around the opening of the urogenital sinus (Fig. 1). After turning the flap, the inferior aspect of the urogenital tract was dissected and exposed. The vagina was incised using catheter ballooning. The junction between the vagina and the urogenital sinus was divided. The posterior flap of the perineal skin and subcutaneous tissue was sutured to the posterior vaginal wall. A 1-cm portion of the anterior vaginal wall was dissected from the posterior wall of the urogenital sinus and the opening of the urogenital sinus was closed with interrupted sutures.
A circumferential incision was made around the corona of the phallus and connected with the incision around the opening of the urogenital sinus. A reduction clitoroplasty was performed to preserve the dorsal neurovascular bundle. The corpora were excised from the corona to just beyond their bifurcation. Two incisions were made through the midline of the preputial flap to accommodate the glans clitoris and the urethral meatus. The preputial flap was brought posteriorly and the free end of the flap was sutured to the anterior vaginal wall (Fig. 2). Lateral suturing was performed until the anterior and posterior flaps met to create the labia minora. The lateral scrotal folds were used to create the labia majora (Fig. 3). A Foley catheter was left in the urethra for 3 or 5 days, and a slight compressive dressing was applied for 3 days. Postoperative appearance showed excellent cosmetic results (Fig. 4).
Among the six patients who underwent the Gonzalez method, three had good results after follow-up times of 3 months, 5 yr, and 12 yr, respectively. The other three patients had long-term complications. One patient had an urethrovaginal fistula that required fistula repair and one had a distal vaginal stenosis that required revision vaginoplasty, both 9 yr after surgery. Both of these two patients underwent revision operations and are now 13 yr old and have no problems. The third patient with a complication had an urethrovaginal fistula and urethral stricture at 3.8 yr after surgery; this patient, however, was lost to follow-up (Table 3). Four of the six patients with CAH who underwent surgery using the Gonzalez method have reached puberty, and two of these patients have experienced genital menarche. None of these patients has experienced clitoral atrophy, hypospadias, or urinary incontinence. Patients and their parents reported satisfaction with external genital appearance.
One patient with CAH who underwent a total urogenital mobilization had a persistent urogenital sinus; revision vaginoplasty was planned at adolescence. The three patients who underwent clitoroplasty only, one each with MGD, partial androgen deficiency, and 5-alpha reductase deficiency syndrome, were planned for delayed vaginoplasty owing to the short distance between the bladder neck and vaginal confluence.
Children born with a urogenital sinus associated with genital ambiguity usually have clitoral hypertrophy, fusion of the labia with absence of the labia minor, and a common urogenital sinus. Patients reconstructed as females are those with excessive androgen stimulation, such as those with CAH, and those with other intersex conditions such as mixed gonadal dysgenesis and true hermaphrodites. For these patients, genital reconstruction usually involves three steps including clitoroplasty (or clitoral reduction), labioplasty, and vaginoplasty (11). Currently, every effort is made to provide a normal cosmetic appearance without sacrificing sensation or vascularity of the glans, due to the importance of the clitoris in female sexual response and in achieving orgasm. Thus, subtunical reduction of cavernous erectile tissue allows preservation of the glans and its neurovascular supply along Buck's fascia, as well as the dorsum of the corpora (12). In CAH patients, the labia minora are absent and the labia majora are superior to the new vaginal introitus. During surgery, the labia minora are created using the split phallic skin, and the labia majora are moved inferiorly by Y-V-plasty to create a vagina with normal cosmetic appearance (13).
Many urologists have contributed to the current state of vaginoplasty for patients with high vaginal confluence (14). Many repairs utilize a posteriorly based perineal flap as first described in 1964 (15). Recognition of the variable anatomy of the genitourinary sinus led to the development of "pull-through" vaginoplasty (16). The Passerini-Glazel method, first described in 1989, uses the mobilized urogenital sinus by dividing it dorsally and using the prepuce to create a tubular flap to the proximal vagina (2). In this method, a posterior inverted U skin flap was not incorporated to prevent skin level stenosis.
The Gonzalez and Fernandes method uses the anterior preputial and posterior skin flaps with the vagina in situ, instead of the extensive vaginal mobilization of the "pull-through" method and slightly modified clitoroplasty (3, 12). This modified technique preserves the muscle complex of the bladder neck and urethra, which is responsible for continence and prevents the morbidity of female hypospadias. This method creates an ample vagina and a normal female appearance of the vulva, and the final anatomical and functional results have been excellent. The operation can be performed on patients of all ages. We prefer the Gonzalez method for patients with ambiguous genitalia and CAH because it is less invasive and gives excellent cosmetic results.
To our knowledge, the long-term results of modern techniques, including the Gonzalez method, have not yet been reported. The long-term results of the Passerini-Glazel operation as a primary or secondary procedure in 22 patients of mean age 2 yr have been described (6). At a mean age of 10 yr, or at 8 yr after surgery, the cosmetic results were good, and none of these patients had clitoral atrophy, hypospadias, or urinary incontinence. Eight girls (36%) had no vaginal stenosis. And four (18%) had mild anastomotic stenosis that was easily dilatable. Ten (45%) of these patients, however, had tight stenosis that required surgical revision. A modification of the Fortunoff technique in 11 patients (mean age at surgery, 3.8 yr) showed superior cosmetic results 2.5 yr after surgery (17). These vaginas were in a more physiological position, and none of these patients experienced vaginal stenosis. One patient had a mild mid-urethral stenosis, which required a single dilation under anesthesia. Most of these patients, however, were prepubertal, and the mean follow-up time was short. Use of a modified Passerini-Glazel feminizing genitoplasty in 46 patients was associated with good cosmetic results with minor complications at a mean follow-up of 5 yr (5). In addition, menarche occurred in 20 patients.
In our series, all patients and parents reported satisfaction with external genital appearance. Two patients (33%) had no vaginal stenosis, and one had mild vaginal stenosis that was easily dilatable. One patient had a tight stenosis that required vaginal dilation under general anesthesia. Two patients had urethrovaginal fistula. However, these results compare favorably with those of other studies owing to the long follow-up period (7.7 yr) and the fact that four of the six patients had gone through puberty. There were no voiding problems such as weak stream or urinary incontinence after surgery including repairs of urethral stricture and urethrovaginal fistula. Unfortunately, we did not assess genital sensation and coitus status. Women with CAH have been reported to have a higher incidence of sexual dysfunction than the normal women (18). Assessment of genital sensation after feminizing genitoplasty in six patients aged ≥ 16 yr showed that all six had highly abnormal clitoral sensation (7). Only three of these patients had an introitus capable of admitting the vaginal probe. A self-administered sexual function assessment completed by the five women who were sexually active showed sexual difficulties, particularly infrequent intercourse and anorgasmia.
Conclusively, feminizing genitoplasty using the Gonzalez method showed good long-term results in patients with ambiguous genitalia and CAH that was a 50% long-term complication rate including urethrovaginal fistula, urethral stricture, and distal vaginal stenosis. The procedure is less invasive than other approaches and results in excellent cosmetic outcomes and complications can be corrected by relatively simple procedures.
Figures and Tables
Fig. 4
Genital appearances. (A) Preoperative image. (B) Postoperative image at the 3 months after surgery.

AUTHOR SUMMARY
Long-term Follow-up after Feminizing Genital Reconstruction in Patients with Ambiguous Genitalia and High Vaginal Confluence
Sungchan Park, Seong Heon Ha, and Kun Suk Kim
Ambiguous genitalia with high vaginal confluence are rare congenital anomalies, observed in only about 5% of patients with congenital adrenal hyperplasia (CAH). The management of children with ambiguous genitalia is an ongoing challenge to the pediatric urologist. A few recent reports have included long-term follow-up of medical and surgical treatment of CAH, but the various surgical methods have given different results. In Korea, there were only 3 reports about feminizing genitoplaty including 2 case reports and 1 short-term result. We retrospectively evaluated the long-term results of 10 feminizing genitoplasties for ten years in Korea. The median follow-up was 7.7 yr and four patients have reached puberty. Feminizing genitoplasty using the Gonzalez method is less invasive than other approaches and results in excellent cosmetic outcomes and complications including urethral stricture and distal vaginal stenosis can be corrected by relatively simple procedures.
References
1. Dumanian GA, Donahoe PK. Bilateral rotated buttock flaps for vaginal atresia in severely masculinized females with adrenogenital syndrome. Plast Reconstr Surg. 1992. 90:487–491.
2. Passerini-Glazel G. A new 1-stage procedure for clitorovaginoplasty in severely masculinized female pseudohermaphrodites. J Urol. 1989. 142:565–568.
3. Gonzalez R, Fernandes ET. Single-stage feminization genitoplasty. J Urol. 1990. 143:776–778.
4. Peña A. Total urogenital mobilization--an easier way to repair cloacas. J Pediatr Surg. 1997. 32:263–267.
5. Lesma A, Bocciardi A, Montorsi F, Rigatti P. Passerini-glazel feminizing genitoplasty: modifications in 17 years of experience with 82 cases. Eur Urol. 2007. 52:1638–1644.
6. Bocciardi A, Lesma A, Montorsi F, Rigatti P. Passerini-glazel feminizing genitoplasty: a long-term followup study. J Urol. 2005. 174:284–288.
7. Crouch NS, Minto CL, Laio LM, Woodhouse CR, Creighton SM. Genital sensation after feminizing genitoplasty for congenital adrenal hyperplasia: a pilot study. BJU Int. 2004. 93:135–138.
8. Kim HH. A case of true hermaphroditism. Korean J Urol. 1990. 31:786–789.
9. Kang HW, Kim KS. A case of mixed gonadal dysgenesis managed in newborn period. Korean J Urol. 1998. 39:289–292.
10. Kwon JB, Yoo ES, Chung SK. Surgical correction of intersex with feminizing genitoplasty. Korean J Urol. 2004. 45:1028–1034.
11. Rink RC, Kaefer M. Kavoussi LR, Novick AC, Partin AW, Peters CA, Wein AJ, editors. Surgical management of intersexuality, cloacal malformation, and other abnormalities of the genitalia in girls. Campbell-Walsh urology. 2007. 9th ed. Philadelphia: Saunders;3830–3869.
12. Kogan SJ, Smey P, Levitt SB. Subtunical total reduction clitoroplasty: a safe modification of existing techniques. J Urol. 1983. 130:746–748.
13. Rink RC, Adams MC. Feminizing genitoplasty: state of the art. World J Urol. 1998. 16:212–218.
14. González R, Piaggio LA. Ambiguous genitalia. Curr Opin Urol. 2006. 16:273–276.
15. Fortunoff S, Lattimer JK, Edson M. Vaginoplasty technique for female pseudohermaphrodites. Surg Gynecol Obstet. 1964. 118:545–548.
16. Hendren WH, Crawford JD. Adrenogenital syndrome: the anatomy of the anomaly and its repair. Some new concepts. J Pediatr Surg. 1969. 4:49–58.
17. Gosalbez R, Castellan M, Ibrahim E, DiSandro M, Labbie A. New concepts in feminizing genitoplasty - is the Fortunoff flap obsolete? J Urol. 2005. 174:2350–2353.
18. May B, Boyle M, Grant D. A comparative study of sexual experiences: women with diabetes and women with congenital adrenal hyperplasia. J Health Psychol. 1996. 1:479–492.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download