Abstract
Carotid intima-media thickness (CIMT) is considered as a surrogate marker for cardiovascular disease (CVD). We determined the normative value of CIMT and correlates of CVD risk factors and Framingham risk score (FRS) in Korean rural middle-aged population. We measured CIMT with a B-mode ultrasonography in 1,759 subjects, aged 40 to 70 yr, in a population-based cohort in Korea. A healthy reference sample (n = 433) without CVD, normal weight and normal metabolic parameters was selected to establish normative CIMT values. Correlates between CIMT and conventional CVD risk factors were assessed in the entire population. Mean values of CIMT (in mm) for healthy reference sample aged 40-49, 50-59, and 60-70 yr were 0.55, 0.59, and 0.66 for men and 0.48, 0.55, and 0.63 for women, respectively. In multivariate regression analysis, CIMT was correlated with older age, higher BMI, male gender, higher LDL-cholesterol level and history of diabetes mellitus. The mean CIMT was also correlated with FRS in both gender (r2 = 0.043, P < 0.01 for men; r2 = 0.142, P < 0.01 for women). We identified normative value of CIMT for the healthy Korean rural middle-aged population. The CIMT is associated with age, obesity, gender, LDL-cholesterol, diabetes mellitus and FRS.
There is great deal of interest in identifying high-risk asymptomatic patients in the general population to prevent mortality and morbidity due to cardiovascular disease (CVD) (1, 2). Measurement of carotid intima-media thickness (CIMT) with a B-mode ultrasonography is a valid approach for identifying and quantifying the presence of subclinical atherosclerosis. It is a noninvasive, sensitive, and reproducible technique for identifying and quantifying atherosclerotic burden and CVD risk. It is also a well-validated research tool that has been translated into clinical practice (2-4).
The American Heart Association Writing Group 3, National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATP III), the American Society of Echocardiography, Screening of Heart Attack Prevention and Education (SHAPE) guideline, European Society of Hypertension recommend measuring CIMT for refining CVD risk assessment in patients with subclinical atherosclerosis (5-8).
Normal CIMT values should be defined on the basis of age, gender and race/ethnicity within a general healthy population (2). Various CVD risk stratification schemes have been developed using prospective data derived predominantly from Caucasian populations. Given the ethnic diversity in the profile of CVD, varied risk associations and different levels of genetic-environmental interactions in different populations, such studies performed in Caucasian populations cannot be directly applied to Korean populations. Currently, there are limited data for the normative values of CIMT in the general East Asian population.
The aim of this study was to determine the normative values of CIMT for healthy Korean subjects aged 40 to 70 yr, based on a cohort in Korea and assess the correlates of CVD risk factors and Framingham risk score (FRS) in entire population.
The Atherosclerosis RIsk of Rural Area iN Korea General population (ARIRANG) study is an ongoing cohort study of cardiovascular and metabolic risk factors conducted in a rural area in Korea. We analyzed 1,716 subjects (male: 40.4%) aged from 40 to 70 who underwent CIMT measurements.
For the assessment of normative CIMT values, we selected a healthy reference sample by excluding subjects with any of the following conditions: 1) history of stroke including cerebral infarction or transient ischemic attack, myocardial infarction, or heart failure; 2) hypertension (systolic blood pressure [SBP] ≥ 140 mmHg, diastolic blood pressure [DBP] ≥ 90 mmHg, or drug treatment for hypertension); 3) diabetes mellitus (fasting blood glucose ≥ 126 mg/dL or drug treatment for diabetes mellitus); 4) total cholesterol ≥ 220 mg/dL or pharmacologic therapy for dyslipidemia; 5) current smoking; and 6) body mass index (BMI) ≥ 30 kg/m2.
All subjects underwent a complete cardiovascular evaluation after 8 hr of fasting, including: 1) medical history for previous stroke, myocardial infarction, heart failure, hypertension, diabetes mellitus, dyslipidemia or smoking; 2) anthropometric analysis including height, weight, waist circumference and hip circumference; 3) blood pressure measurement (obtained after 10 min of rest in the sitting position, expressed as the average of three consecutive measurements); 4) serum glucose levels; 5) plasma lipids profile including total cholesterol, triglyceride, high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C) level; 6) serum high sensitive C-reactive protein (hs-CRP) level.
The measurement was carried out according to a validated procedure, using a high-resolution B-mode ultrasonography view of the far wall of the common carotid artery, with an ultrasonography system (Vivid-7; General Electric-Vingmed, Milwaukee, WI, USA) and a phased array 12-MHz transducer (9).
Patients were placed comfortably in the supine position with the head directed away from the side of interest and the neck extended slightly. Thereafter, the proximal, mid, and distal common carotid artery (CCA), carotid bifurcation, and proximal portion of internal carotid artery were systematically interrogated along the long- and short-axis views. Still images of the CCA and carotid bifurcation were digitally acquired. The CIMT was determined at the far wall of the CCA using the semi-automated edgedetection software. Using this software, a region of interest (about 2 cm in length and 1 cm away from bifurcation) was placed perpendicular to the vessel wall. The software detects the lumenintima and the media-adventitia interface at the far wall of the vessel (Fig. 1). Because mean values are more reproducible, we use the mean CIMT (2).
Risk assessment for determining the 10-yr risk for developing CVD is carried out using Framingham risk score. The risk factors included in the Framingham calculation of 10-yr risk are: age, total cholesterol, HDL-C, SBP, treatment for hypertension, and cigarette smoking. The calculation was performed according to the ATP III guideline (6).
Data for continuous variables are presented as the mean ± standard deviation and proportions are presented as frequencies and percentages. The CIMT data between the different age groups were assessed by one-way ANOVA and Post Hoc analysis was performed with Scheffe's test. We evaluated the effect of traditional risk factors on CIMT (as a continuous variable) using linear regression both with and without adjustment for age and gender. Multivariate regression analysis was performed using the following variables: age, gender, SBP, DBP, triglycerides, HDL-C, LDL-C, hs-CRP which was log-transformed because of a positive skew distribution, BMI, history of diabetes mellitus and smoking including current and ex-smoking. The correlate of Framingham risk score and CIMT was assessed by simple linear regression analysis without adjustment of other factors. All tests were two-sided and P < 0.05 was considered to be statistically significant. SPSS for Windows-version 15 (SPSS Inc., USA) was used for analyses.
The study population was consisted of 1,716 subjects (693 [40.4%] men) aged 40 to 70 yr (mean age 55.1), of whom 433 (107 [24.7%] men) were found to be healthy (Fig. 2). In entire population, men were older and have more frequent history of stroke and diabetes mellitus. Smoking was also frequent in men. Men were taller and heavier than women, but mean BMI was not different between two genders. SBP and DBP were higher in men. Total cholesterol level was similar but triglyceride level was higher in men. On contrary, HDL-C and LDL-C level was higher in women. Higher hs-CRP level was observed in men. Demographic, clinical and laboratory characteristics of the study population were presented in Table 1.
In the healthy reference sample, mean CIMT was higher in men (0.60 ± 0.12 mm vs 0.53 ± 0.10 mm, P < 0.01). A significant correlation was observed between age and mean CIMT for both men (r2 = 0.144, P < 0.01) and women (r2 = 0.321, P < 0.01). Mean values of CIMT (in mm) in healthy subjects aged 40-49, 50-59, and 60-70 yr were: 0.55 ± 0.08, 0.59 ± 0.13, and 0.66 ± 0.13 mm for men and 0.48 ± 0.07, 0.55 ± 0.09, and 0.63 ± 0.12 mm for women, respectively. Mean values of CIMT in men were higher at each age group but not in subjects aged 60-70 yr (0.66 ± 0.13 mm vs 0.63 ± 0.12 mm, P = 0.38). Mean CIMT values according to age groups were presented at Fig. 3. The mean value and 5th, 10th, 25th, 50th, 75th, 90th, and 95th percentiles value of CIMT among men and women according to age groups were presented in Table 2.
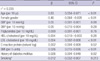
In the entire population, CIMT showed associations with age, gender, SBP, DBP, total cholesterol, triglyceride, HDL-C, LDL-C, BMI, history of diabetes and smoking by simple linear regression. After adjustment for age and gender, these associations were persistent (Table 3). In multivariate regression analysis, independent predictors of increasing CIMT were older age, higher BMI, male gender, higher LDL-C level and history of diabetes mellitus (Table 4).
Linear regression between increasing CIMT and Framingham risk score was performed in the entire population. A significant correlation was observed for both men (r2 = 0.043, P < 0.01) and women (r2 = 0.152, P < 0.01) but weak correlation in men (Fig. 4).
We present normative values of CIMT for healthy Korean rural adults aged 40-70 yr. We also report on the cross-sectional associations between increasing CIMT and conventional cardiovascular risk factors in entire sample. In addition, we present the correlation CIMT and Framingham risk score in this population.
The Oslo Ischemia Study showed that a significant number of participants remain asymptomatic despite significant coronary artery disease, but sudden cardiac death frequently occurs at the first presentation of coronary heart disease (10). Thus, it is very important to identify subjects who are in subclinical atherosclerosis and initiate primary prevention for CVD. The extent of carotid atherosclerosis positively correlates with the severity of coronary atherosclerosis and the severity of CIMT independently correlates with the risk of major cardiovascular disease such as transient cerebral ischemia, stroke and coronary events. Therefore, measurement of CIMT with B-mode ultrasonography is a valid, noninvasive, sensitive and reproducible technique (2).
Although many committees and studies have shown the importance of CIMT measurements, there is not enough data regarding normal CIMT values, especially in Koreans. Recent studies including the Atherosclerosis Risk in Communities (ARIC) and Multi-Ethnic Study of Atherosclerosis (MESA) have showed different CIMT values according to age, gender and geographical origin, and therefore normative CIMT values should be defined based on these factors (2, 11). The American Society of Echocardiography recommends population-specific normative data according to age, gender, and ethinicity (2). Since data from Caucasian populations cannot be directly applied to Korean because of difference of genetic and environmental factors, the normative data provided for CIMT in our study will allow the application of CIMT measurement in individual subjects from this ethnic group.
Our study is not the first report of normative CIMT values in Korean. Bae et al. (12) and Cho et al. (13) already reported normative CIMT values in Korean. But, Cho et al. did not use the semi-automated edge-detection method for measuring CIMT and Bae et al. used subjects who had visited the general hospital and BMI was not considered in the criteria for healthy subjects (12, 13). The mean CIMT in our study was thinner than those of the two Korean studies, independent of age. Difference of mean CIMT could be explained that our study was based on a cohort and used very strict criteria for healthy subjects.
The statistical difference of mean CIMT between men and women was not observed in subjects aged 60-70 yr despite correlation of increasing CIMT and age in entire population. This phenomenon could be explained by menopause in females and this finding correlates well with a study of the effect of menopause on carotid artery remodeling (14).
Since the National Cholesterol Education Program (NCEP) Expert Panel (ATP III) recommends measuring CIMT because the finding of an elevated CIMT (e.g., ≥ 75th percentile for age and gender) could reclassify a person with multiple risk factors to a higher risk category, we also present the 5th, 10th, 25th, 50th, 75th, 90th, and 95th percentiles value of CIMT among men and women (5, 6). Further evaluation which percentiles of value should be used for cut-off value of abnormal CIMT is needed.
In our study, the mean CIMT was significantly correlated with age, gender and other cardiovascular risk factors including SBP, DBP, total cholesterol, triglyceride, HDL-C, LDL-C, hs-CRP, BMI, history of diabetes mellitus and smoking by simple linear regression. But, in multivariate analysis using stepwise linear regression, only age, BMI, gender, LDL-C and history of diabetes mellitus were correlated with increasing CIMT in this population. We could explain the reason for this result as following: First, there might be the potential ethnic differences regarding the role of classic versus novel risk factor as determinants of carotid atherosclerosis and cardiovascular risk. Second, because metabolic components clustered closely with each others, multiple collinearity should be considered to accept this result. To confirm correlates with CIMT, further studies would be required.
We evaluated the relationship between CIMT and Framingham risk score because the Framingham risk score accurately estimates 10-yr CVD risk (2). In our study, CIMT was correlated well with Framingham risk score in both genders, but the CIMT of men showed weak correlation with Framingham risk score compared with the CIMT of women. Because relatively small number of men and lack of diabetes mellitus and obesity for calculating Framingham risk score may be the reasons that their CIMT values showed weak correlate with FRS. Another reason could be that since Framingham risk equations are derived from a North American population, consisting of mainly whites, it is not clear if they can directly be extrapolated to the Korean population and some concern has been raised over the fact that the original Framingham risk score underestimated risk (15). Whether the estimating the vascular age by mean of measuring the CIMT could be a better approach for calculating CVD risk should be evaluated with the long-term follow-up data.
Our study is limited by its cross-sectional nature. In addition, our examination for CIMT was limited to measurement of either side of common carotid arteries and lack of data for presence of carotid plaque which is another important marker for atherosclerosis. Although we exclude the subjects with CVD by history for previous stroke, myocardial infarction or heart failure, we did not exclude the subjects of peripheral artery disease because of lack of availability of the data. However, pending prospective data, our results for normative CIMT value provide important insights into the determinants of subclinical vascular disease in this population. A longitudinal study is needed for a better evaluation of the relationships between cardiovascular risk factors, subclinical atherosclerosis and the risk of cardiovascular events in this population.
In conclusion, normative CIMT values were identified for the healthy Korean rural adults aged 40-70 yr using a B-mode ultrasonography. The values are closely associated with age, obesity, gender, LDL-C and diabetes mellitus. Increasing CIMT is correlated with Framingham risk score in both genders.
Figures and Tables
Fig. 1
Measuring Carotid Intima-Media Thickness Measurement using a high-resolution B-mode ultrasonography view of the far wall of the common carotid artery, with an ultrasonography system. The software detects the lumen-intima and the media-adventitia interface at the far wall of the vessel.

Fig. 3
Estimation of mean carotid intima-media thickness according to age groups and genders in healthy reference (men = 107; women = 326). CIMT, carotid intimamedia thickness.

Fig. 4
Correlation between carotid intima-media thickness and Framingham risk score according to gender (men = 693; women = 1,023). CIMT, carotid intima-media thickness.

Table 2
The mean value and 5th, 10th, 25th, 50th, 75th, 90th, and 95th percentiles value of carotid intima-media thickness among men and women according to age group

Table 3
Association of individual atherosclerotic risk factors with increasing CIMT in linear regression models with and without adjustment for age and gender (n = 1,716)

*Defined as current smoking or ex-smoking. BMI, body mass index; Chol., cholesterol; CI, confidence interval; DBP, diastolic blood pressure; DM, diabetes mellitus; HDL-C, high density lipoprotein cholesterol; hs-CRP; high sensitive C-reactive protein; LDL-C, low density lipoprotein cholesterol; SBP, systolic blood pressure; TG, triglyceride.
AUTHOR SUMMARY
Normative Values and Correlates of Mean Common Carotid Intima-Media Thickness in the Korean Rural Middle-aged Population: The Atherosclerosis RIsk of Rural Areas iN Korea General Population (ARIRANG) Study
Young Jin Youn, Nam Seok Lee, Jang-Young Kim, Jun-Won Lee, Joong-Kyung Sung, Sung-Gyun Ahn, Byung-Su You, Seung-Hwan Lee, Junghan Yoon, Kyung-Hoon Choe, Sang Baek Koh, and Jong Ku Park
Carotid intima-media thickness (CIMT) is considered as a surrogate marker for cardiovascular disease (CVD). We determined the normative value of CIMT and correlates of CVD risk factors and Framingham risk score (FRS) in a community based cohort in Korea. We measured CIMT with a B-mode ultrasonography in a consecutive 1,759 subjects, aged 40 to 70 yr. A healthy reference subject (n = 433) without CVD, normal weight and normal metabolic parameters was selected to establish normative CIMT values.
Correlates between CIMT and conventional CVD risk factors were assessed in the entire population. Mean normative values of CIMT aged 40-49, 50-59 and 60-70 were 0.55, 0.59 and 0.66 mm for men and 0.48, 0.55 and 0.63 mm for women, respectively. In multivariate regression analysis, CIMT was positively correlated with age, body mass index, male, LDL-cholesterol level and history of diabetes mellitus. The mean CIMT was also correlated with FRS in both gender (r2 = 0.043, P < 0.01 for men; r2 = 0.142, P < 0.01 for women).
References
1. Taylor AJ, Merz CN, Udelson JE. 34th Bethesda Conference: executive summary-can atherosclerosis imaging techniques improve the detection of patients at risk for ischemic heart disease? J Am Coll Cardiol. 2003. 41:1860–1862.
2. Stein JH, Korcarz CE, Hurst RT, Lonn E, Kendall CB, Mohler ER, Najjar SS, Rembold CM, Post WS. American Society of Echocardiography Carotid Intima-Media Thickness Task Force. Use of carotid ultrasonography to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force. Endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr. 2008. 21:93–111.
3. Stein JH, Fraizer MC, Aeschlimann SE, Nelson-Worel J, McBride PE, Douglas PS. Vascular age: integrating carotid intima-media thickness measurements with global coronary risk assessment. Clin Cardiol. 2004. 27:388–392.
4. Gepner AD, Keevil JG, Wyman RA, Korcarz CE, Aeschlimann SE, Busse KL, Stein JH. Use of carotid intima-media thickness and vascular age to modify cardiovascular risk prediction. J Am Soc Echocardiogr. 2006. 19:1170–1174.
5. Greenland P, Abrams J, Aurigemma GP, Bond MG, Clark LT, Criqui MH, Crouse JR 3rd, Friedman L, Fuster V, Herrington DM, Kuller LH, Ridker PM, Roberts WC, Stanford W, Stone N, Swan HJ, Taubert KA, Wexler L. Prevention conference V: beyond secondary prevention; identifying the high-risk patient for primary prevention: noninvasive tests of atherosclerotic burden: Writing Group III. Circulation. 2000. 101:E16–E22.
6. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002. 106:3143–3421.
7. Naghavi M, Falk E, Hecht HS, Jamieson MJ, Kaul S, Berman D, Fayad Z, Budoff MJ, Rumberger J, Naqvi TZ, Shaw LJ, Faergeman O, Cohn J, Bahr R, Koenig W, Demirovic J, Arking D, Herrera VL, Badimon J, Goldstein JA, Rudy Y, Airaksinen J, Schwartz RS, Riley WA, Mendes RA, Douglas P, Shah PK. SHAPE Task Force. From vulnerable plaque to vulnerable patient--Part III: executive summary of the Screening for Heart Attack Prevention and Education (SHAPE) Task Force report. Am J Cardiol. 2006. 98:2H–15H.
8. Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Struijker Boudier HA, Zanchetti A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Kjeldsen SE, Erdine S, Narkiewicz K, Kiowski W, Agabiti-Rosei E, Ambrosioni E, Cifkova R, Dominiczak A, Fagard R, Heagerty AM, Laurent S, Lindholm LH, Mancia G, Manolis A, Nilsson PM, Redon J, Schmieder RE, Struijker-Boudier HA, Viigimaa M, Filippatos G, Adamopoulos S, Agabiti-Rosei E, Ambrosioni E, Bertomeu V, Clement D, Erdine S, Farsang C, Gaita D, Kiowski W, Lip G, Mallion JM, Manolis AJ, Nilsson PM, O'Brien E, Ponikowski P, Redon J, Ruschitzka F, Tamargo J, van Zwieten P, Viigimaa M, Waeber B, Williams B, Zamorano JL. The task force for the management of arterial hypertension of the European Society of Hypertension. The task force for the management of arterial hypertension of the European Society of Cardiology. 2007 Guideline for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2007. 28:1462–1536.
9. O'Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK Jr. Cardiovascular Health Study Collaborative Research Group. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. N Engl J Med. 1999. 340:14–22.
10. Thaulow E, Erikssen J, Sandvik L, Erikssen G, Jorgensen L, Cohn PF. Initial clinical presentation of cardiac disease in asymptomatic men with silent myocardial ischemia and angiographically documented coronary artery disease (the Oslo Ischemia Study). Am J Cardiol. 1993. 72:629–633.
11. Chambless LE, Heiss G, Folsom AR, Folsom AR, Rosamond W, Szklo M, Sharrett AR, Clegg LX. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) study, 1987-1993. Am J Epidemiol. 1997. 146:483–494.
12. Bae JH, Seung KB, Jung HO, Kim KY, Yoo KD, Kim CM, Cho SW, Cho SK, Kim YK, Rhee MY, Cho MC, Kim KS, Jin SW, Lee JM, Kim KS, Hyun DW, Cho YK, Seong IW, Jeong JO, Park SC, Jeong JY, Woo JT, Koh G, Lim SW. Analysis of Korean carotid intima-media thickness in Korean healthy subjects and patients with risk factors: Korea multi-center epidemiological study. Korean Circ J. 2005. 35:513–524.
13. Cho YL, Kim DJ, Kim HD, Choi SH, Kim SK, Kim HJ, Ahn CW, Cha BS, Lim SK, Kim KR, Lee HC, Huh KB. Reference values of carotid intima-media thickness and association with atherosclerotic risk factors in healthy subjects in Korea. Korean J Med. 2003. 64:275–283.
14. Muscelli E, Kozàkovà M, Flyvbjerg A, Kyriakopoulou K, Astiarraga BD, Glintborg D, Konrad T, Favuzzi A, Petrie J. RISC investigators. The effect of menopause on carotid artery remodeling, insulin sensitivity, and plasma adiponectin in healthy women. Am J Hypertens. 2009. 22:364–370.
15. Brindle PM, McConnachie A, Upton MN, Hart CL, Davey Smith G, Watt GC. The accuracy of the Framingham risk-score in different socioeconomic groups: a prospective study. Br J Gen Pract. 2005. 55:838–845.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download