Abstract
The clinical diagnosis of trichinellosis can be difficult due to lack of pathognomonic signs or symptoms. In Korea, since the first report of human infection by Trichinella spiralis in 1997 following the consumption of raw badger meat, there have been occasional trichinellosis outbreaks. We describe an outbreak of 12 cases of trichinellosis in Korea and implicate raw wild boar meat as the culprit. A total of 27 larvae of Trichinella (0.54 larvae per gram of meat) were recovered from the leftover raw wild boar meat.
Human trichinellosis is a parasitic infection caused by Trichinella roundworms. The traditional route of infection is by ingesting raw or improperly cooked pork from infected domestic swine. Eight species and three genotypic variants have been identified in various animal hosts (1), and Trichinella spiralis is the most common cause of human trichinellosis (2).
Trichinellosis is a globally distributed disease. In Asia, there have been reports of outbreaks from China, Japan, Thailand, Laos, Vietnam and other countries including Korea (3). Information on trichinellosis including the source of infection in Korea is limited. Eating raw badger meat was responsible for the first outbreak in Korea in 1997 (n = 3) (4), and raw wild boar meat was the source of outbreaks in 2001 (n = 5), 2003 (n = 4) and 2003 (n = 13) (5).
Dupouy-Camet et al. proposed an algorithm ranging from "very unlikely" to "confirmed" based on clinical setting and without parasitological diagnosis for determining the probability of acute trichinellosis (6). According to this algorithm, we report 2 cases of "confirmed trichinellosis", 1 case of "highly probable trichinellosis", 4 cases of "probable trichinellosis" and 5 cases of "suspected trichinellosis" and present raw wild boar (Sus scrofa) meat as the source of infection.
A 51-yr-old woman without any previous medical history was admitted to a local hospital in Gyeonggi-do, on December 23, 2010, complaining of fever and a chilling sense for 3 days. She also complained of myalgia, poor oral intake and facial edema. Her body temperature was 36.5℃. A complete blood count showed eosinophilia (1,960 cells/µL, normal = 50-450 cells/µL) without leukocytosis. Creatinine kinase levels were 315 U/L (normal range = 20-270 U/L) and LDH was 465 U/L (normal range = 218-472 U/L). Urinalysis was normal and chest radiography demonstrated no active lung lesion. No helminth ova were found in the stool examination for parasites. The patient was given 30 mg of prednisolone orally once a day starting December 24, 2010 due to fever and an uprising in eosinophilia (up to 3,900 cells/µL on December 27, 2010).
Her symptoms improved after the prednisolone was started, but she was transferred to Seoul National University Hospital for further evaluation of febrile eosinophilia on December 28, 2010. On arrival at Seoul National University Hospital, she had a fever (39.0℃) with chilling sense, myalgia and watery diarrhea. Her white blood cell count was 11.5 × 103 cells/µL with 44.0% eosinophils, and creatinine kinase levels were 494 U/L and LDH was 400 U/L. Aspartate aminotransferase was 48 IU/L (normal < 40 IU/L) and alanine aminotransferase was 91 IU/L (normal < 40 IU/L). She said that she, her husband and 10 more villagers had consumed raw wild boar meat which was obtained by hunting on December 2, 2010. An enzyme-linked immunosorbent assay (ELISA) using larval antigens of T. spiralis was done on December 29, 2010 and was negative (0.007 optical density [OD] units, positive control 0.355 OD units). A follow up ELISA performed on January 13, 2011 was also negative (0.021 OD units, positive control 0.351 OD units). Stored raw wild boar meat was recovered from the patient's freezer and was brought to the hospital for examination. The leftover boar meat was digested with artificial gastric juice to recover Trichinella larvae. After removing fat and fascia, muscle tissue was finely trimmed with scissor. Then, 50 g of muscle from the raw wild boar meat was digested at 37℃ for 1 hr in 1,000 mL of digestive solution constituted with 6 g of pepsin and 6 mL of HCl (37%) in distilled water. After eliminating the impurities with a 180 µm sieve, the worms were recovered by filtration with a flow-through using a 50 µm sieve. A total of 27 larvae of Trichinella (0.54 larvae per gram of meat) were recovered from digested wild boar meat (Fig. 1).
Based upon a putative diagnosis of trichinellosis, the patient's drug regimen was switched to 400 mg of albendazole taken orally twice a day and prednisolone was not given since December 27, 2010. Following the change in drug therapy, levels of muscle enzymes was decreased, the fever subsided and her chilling sense and myalgia improved. Seven days after the change in drug therapy, the patient was discharged to her home. Visiting an outpatient clinic seven days after discharge, the patient had mild myalgia and her laboratory tests showed a resolving state of eosinophilia.
Her husband was also admitted to the hospital on December 31, 2010 complaining of fever and chilling sense. He presented with chilling sense, periorbital swelling, and his eosinophil count was 7,399 cells/µL upon admission. ELISA was performed twice: the first test done on December 30, 2010 was negative (0.004 OD units, positive control 0.420 OD units) but the second done on January 13, 2011 was positive (0.262 OD units, positive control 0.351 OD units). Albendazole (400 mg) twice a day was given from December 31, 2010. He showed improvement in symptoms after starting the albendazole treatment and was discharged in 4 days.
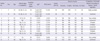
The wild boar was hunted at Gangwon-do and brought to Gyeonggi-do where the patients lived. A total of 12 villagers including the wife and husband consumed half of the wild boar meat, and the other half was given to a group of people living in a neighboring village. The 12 villagers who shared the wild boar meat were examined they presented at least one symptom of trichinellosis with a median of 20 days after the ingestion of the meat. Two of them were positive by ELISA for specific IgG antibodies to Trichinella antigens. Their clinical, epidemiological and laboratory features are presented in Table 1.
A total of 21 human cases of trichinellosis have been reported in Korea so far (Table 2). There had been two case reports of trichinellosis after ingestion of raw wild badger and two case reports of trichinellosis after ingestion of raw wild boar meat.
The ELISA tests that include the T. spiralis excretory-secretory antigens allows for detection as early as 2 weeks after infection, reaching a sensitivity of 100% at 50 days (9). In this report, a total of 12 villagers who had consumed raw boar meat underwent serological tests. As a result, 2 (16.6%) were positive to T. spiralis after 4-6 weeks of their ingestion of the raw wild boar meat. The 10 patients were ELISA negative for specific antibodies in serum which was taken 4 weeks after the ingestion of the meat. Since the sensitivity reaches at highest level at 50 days after the ingestion of the meat, the serology test was made rather earlier and this may be the reason of the serology negative. The sensitivity and specificity of the ELISA test in this lab has not yet been established due to the low occurrence of trichinellosis test orders. The sensitivity and specificity of this ELISA for IgG antibodies to Trichinella antigens after 4-6 weeks of ingestion of the meat should be studied further.
Muscle biopsy was not done in all cases and ELISA was negative in the case of the admitted woman. According to the algorithm proposed by Dupouy-Camet et al. (6), the case of wife is classified as a "highly probable" case of trichinellosis, since she presented with fever, facial edema, myalgia, eosinophillia and increased levels of muscle enzymes. In the case of her husband, ELISA was positive after 41 days of consuming raw wild boar meat, which makes the case as a "confirmed" case. The 10 cases of villagers who ingested the wild boar meat were ranged from a confirmed case to a very unlikely case according to the algorithm proposed by Dupouy-Camet et al. (6). Their diagnosis and management of trichinellosis were made clinically.
The detection of the Trichinella larvae from the leftover raw wild boar is an important clue for the diagnosis in these cases. The prevalence of trichinellosis in wild boar (Sus scrofa) has been reported as 2.0% by the detection of antibodies with ELISA based testing for excretory/secretory antigens of Trichinella spiralis in France (10), and 11.4% by artificial digestion in Argentina (11). Detecting larvae from leftover meat can contribute to the early diagnosis of trichinellosis infection especially within two weeks of infection. On clinical suspicion, the leftover meat should be sought to confirm the source and species of the etiologic agent of disease (12).
In summary, we report 12 cases of clinically diagnosed trichinellosis associated with raw boar meat and suggest that worm recovery from the leftover meat could serve as an important clue for early diagnosis.
Figures and Tables
Fig. 1
A Trichninella spiralis larva recovered from the muscle of leftover raw boar meat after artificial digestion. Scale bar = 100 µm.

References
1. Pozio E, Zarlenga DS. Recent advances on the taxonomy, systematics and epidemiology of Trichinella. Int J Parasitol. 2005. 35:1191–1204.
2. Pozio E, Gomez Morales MA, Dupouy-Camet J. Clinical aspects, diagnosis and treatment of trichinellosis. Expert Rev Anti Infect Ther. 2003. 1:471–482.
3. Stehr-Green JK, Schantz PM. Trichinosis in Southeast Asian refugees in United States. Am J Public Health. 1986. 76:1238–1239.
4. Sohn WM, Kim HM, Chung DI, Yee ST. The first human case of Trichinella spiralis infection in Korea. Korean J Parasitol. 2000. 38:111–115.
5. Hur GY, Hwang BY, Lee JG, Lee MG, Cheong HJ, Cho SW, Joo KH. An outbreak of trichinellosis caused by ingestion of raw wild boar. Korean J Med. 2004. 67:S917–S922.
6. Dupouy-Camet J, Kociecka W, Bruschi F, Bolas-Fernandez F, Pozio E. Opinion on the diagnosis and treatment of human trichinellosis. Expert Opin Pharmacother. 2002. 3:1117–1130.
7. Lee HC, Kim JS, Oh HY, Kim JH, Kim HG, Lee MS, Kim WJ, Kim HT. A case of Trichinosis caused by eating a wild badger. Korean J Med. 1999. 56:134–138.
8. Kim E, Pyun RH, Park JH, Kim KH, Choi I, Park HH, Lee YH, Yong TS, Hong SK. Family outbreak of Trichinosis after eating a raw meat of wild swine. Infect Chemother. 2003. 35:180–184.
9. Capó V, Despommier DD. Clinical aspects of infection with Trichinella spp. Clin Microbiol Rev. 1996. 9:47–54.
10. Richomme C, Lacour SA, Ducrot C, Gilot-Fromont E, Casabianca F, Maestrini O, Vallée I, Grasset A, van der Giessen J, Boireau P. Epidemiological survey of trichinellosis in wild boar (Sus scrofa) and fox (Vulpes vulpes) in a French insular region, Corsica. Vet Parasitol. 2010. 172:150–154.
11. Cohen M, Costantino SN, Calcagno MA, Blanco GA, Pozio E, Venturinello SM. Trichinella infection in wild boars (Sus scrofa) from a protected area of Argentina and its relationship with the presence of humans. Vet Parasitol. 2010. 169:362–366.
12. Madariaga MG, Cachay ER, Zarlenga DS. A probable case of human neurotrichinellosis in the United States. Am J Trop Med Hyg. 2007. 77:347–349.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download