Abstract
Accurate measurement of fat mass has become increasingly important with the increasing incidence of obesity. We assessed fat and muscle mass of Koreans with the Korea National Health and Nutrition Examination Survey IV (KNHANES IV). We studied 10,456 subjects (aged 20 to 85 yr; 4,476 men, 5,980 women). Fat and muscle mass were measured by dual-energy x-ray absorptiometry. Reference values of body compositions were obtained using the LMS method. The fat mass index (FMI, body fat mass/height2; kg/m2) of Korean men did not correlate with age (P = 0.452), but those of Korean women (P < 0.001) did. The ratio of percentage of fat in the trunk and legs was positively related with age in both the genders. The appendicular lean mass/height2 (kg/m2) of Korean men was negatively related to age (P < 0.001). In women, this ratio increased with age (P < 0.001). When we defined obesity according to the FMI classification, the rates of obesity were 6.1% (FMI > 9 kg/m2) in men and 2.7% (FMI > 13 kg/m2) in women. It is concluded that the muscle mass decreases and obesity increases with aging in Korean men, whereas both fat mass and obesity increase with aging in Korean women.
The incidence of obesity has increased rapidly over the past 3 decades, with the World Health Organization (WHO) recently issuing a warning that in the near future, obesity and diabetes will become serious issues, even for developing countries (1). Being overweight and in particular, obese is a major risk factor for several chronic diseases, including type 2 diabetes mellitus, cardiovascular diseases, hypertension, stroke, and certain types of cancer (2-4). As the incidence of obesity increases, the need for accurate measurements of adiposity in order to allow appropriate diagnosis and treatment also increases.
The body mass index (BMI) is the most popular tool for evaluation of obesity because of its simplicity and low cost. However, measurement of real adiposity is confounded by factors such as age, gender, and ethnicity (5, 6). Dual-energy x-ray absorptiometry (DXA) accurately detects adiposity and provides information on the total and regional percentages of fat (7). According to previous comparisons between the BMI and DAX methods, Asians, particularly of Indian ethnicity, have higher real levels of body fat and higher prevalence of metabolic syndrome at any given BMI than the Caucasians (8, 9). Therefore, it is necessary to map the ethnic characteristics of fat mass and changes in the body composition to better understand the relationship between adiposity and metabolic change. A number of studies have investigated age, gender, and ethnic group-specific differences in whole body and regional bone mineral density (BMD). Other studies compared the real percentage of body fat to BMI, waist circumferences, and waist-to-stature ratios in adults. More recently, Kelly et al. (10) reported body composition reference values from the United States' National Health and Nutrition Examination Survey (NHANES) and investigated discrepancies in the fat mass index (FMI; fat mass/height2). Until recently, no comprehensive source of body composition data representing the Korean population was available for analysis.
The Korea National Health and Nutrition Examination Survey (KNHANES), designed to assess the health and nutritional status of adults and children living in Korea, was initiated in 1998. The Korea Centers for Disease Control and Prevention administers this nationally representative survey. The KNHANES targets the non-institutionalized civilian Korean population and collects data through interviews, physical examinations, and medical tests. The KNHANES IV (2007-2009) survey began in July 2008, and it measures the bone mineral density of the spine and hip and the body composition by DXA in mobile examination centers.
In this study, we report age- and sex-specific differences between the body composition of Koreans and the reference values.
Through the KNHANES IV program, the parameters of 10,456 subjects aged between 20 and 85 yr (4,476 men and 5,980 women) were analyzed. The KNHANES IV was a nationwide cross-sectional survey conducted in Korea in 2007-2009. This survey used a stratified multi-stage clustered probability sampling to select a representative sample of the non-institutionalized civilian Korean population. DXA examinations were conducted on subjects over 20 yr of age. Pregnant women and subjects who had undergone a contrast agent-based examination within a week of the survey were excluded. Subjects were also excluded if their reported weight exceeded the weight limit of the DXA scan table (136 kg), or if their reported height was greater than the length of the DXA scan table (196 cm).
In the KNHANES, whole body DXA exams were conducted with a QDR Discovery (formerly, the QDR 4500A) fan beam densitometer (Hologic, Inc., Bedford, MA, USA), in accordance with the procedures recommended by the manufacturer. All subjects changed into light clothing and removed all jewelry and other things that could interfere with the DXA examination. The results of DXA were analyzed using industry standard techniques at the Korean Society of Osteoporosis. Analysis was performed using Hologic Discovery software (version 13.1) in its default configuration. The examinations that revealed items with the ability to affect the accuracy of DXA results, such as prosthetic devices, implants, or other extraneous objects, were recorded as missing in the dataset for regional and global DXA results.
The precision of the DXA instrument has been previously reported. The results of body composition measurements can vary according to the technology employed and calibration of the instrument used. The DXA instruments used in the NHANES surveys were calibrated according to the methods proposed by Schoeller et al. (11). The reference values of the NHANES are obtained using this calibration method (10). For appropriate comparison between the present and previous data, the NHANES calibrations were applied. DXA calibrations were maintained through an internal referencing system, which periodically measures bone and soft tissue equivalent reference standards during the examination of the patients. The KNHANES data sets include whole body DXA measurements of bone mineral content (BMC, g), bone mineral density (BMD, g/cm2), fat mass (g), lean mass including BMC (g) and percentage fat (fat mass/total mass × 100), along with demographic information each subject. Data were also collected for a number of pre-defined anatomical regions, including the head, arms, legs, trunk, pelvic regions, subtotal of the whole body (excluding only the head), and the whole body. From these data, the following derivative values were calculated: FMI (body fat mass excluding the head area/height2), lean mass/height2, appendicular lean mass/height2, and appendicular lean mass/total lean mass. The total body and sub-total body reference values and the above derivative reference values were generated. As fat distribution may be as important as total fat mass, 2 indices of fat mass distribution were included in the analysis: percentage of fat in the trunk/percentage of fat in the legs, and fat mass of the trunk/fat mass of the limbs (fat mass of the arms and legs). These latter indices may have a role in defining metabolic syndrome or lipodystrophy (12, 13).
This study analyzed publicly available data sets, and was, therefore, exempted from institutional review board approval.
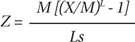
The data were divided into subgroups according to gender. A curve-fitting procedure called LMS (lmsChartMaker Pro Version 2.3, Medical Research Council, UK) (14) was used to generate the reference curves, because it is capable of handling situations wherein the underlying reference data are skewed (not normally distributed). It normalizes the underlying reference data through a division of independent characteristics (e.g., age) to form groups, and then applies an extension to 1 tail of the distribution and a contraction to the other, thus eliminating any skew in the variable under analysis. A smooth curve is fitted to the normalizing power transformation for each age group, generating an optimum "L" (power) curve that normalizes the dependent measure, e.g., fat percentage, over the entire age range. The procedure also fits the median (M) and coefficient of variation (S) curves, and together, these 3 curves (L, M, and S) fully describe the reference data. We have reported the more commonly used population standard deviation, s, which is S times M. The z-scores can be calculated by the following equation:
where X is the physical measurement (e.g., DXA total body BMD, DXA fat percentage, etc.), L is the power transformation, M is the median value, and s is the population standard deviation (14). Percentiles can be obtained from z-scores. For example, z-scores of -1.881, -1.645, -0.674, 0, 0.674, 1.645, and 1.881 correspond to the 3rd, 5th, 25th, 50th, 75th, 95th, and 97th percentiles respectively.
During the curve-fitting process, weighted observations from the KNHANES data sets were fitted by selecting more parsimonious models over more complex models, as long as there was similarity in the fit in an attempt to avoid over fitting the curves. Further, we employed careful visual inspection of the Q statistic, a plot of standardized residuals in which the data are split into groups, and the non-random group variations in the estimated z-scores are plotted against the equivalent degrees of freedom used to fit the curve. The Q statistic is considered satisfactory at or below a value of 2 for the L, M, and S curves, if the fitted curve was plausible for the data being fitted (14).
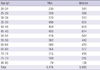
The number of subjects in the reference database according to the age groups and gender is listed in Table 1. The reference curves were developed from whole body DXA measurements and derivative values from the 2008-2009 KNHANES data set. Reference values by sex for each of the DXA measurements are provided in Table 2. Scatter plots with fits, including the mean, 3rd, 10th, 25th, 75th, 90th, and 97th percentiles, are superimposed on the raw data values and are illustrated in Fig. 1.
Almost all parameters exhibited correlations with age, except FMI in men (Table 3). As anticipated, significant differences were observed between the genders for the different measures, and these differences varied with age. The BMI and FMI of men increased rapidly until 40 yr of age, and then showed a gentle upward slope until 55 yr of age (Fig. 1). However, the same parameters in women increased steadily until 65 yr of age (Fig. 1). The means of fat percentages in women were greater than those in men (Fig. 1). Fat percentages in women steadily increased until 40 yr of age, and then increased sharply. In men, fat percentages increased rapidly until 30 yr of age, and then showed only a gradual increase (Fig. 1). Waist circumference, percentage of fat in the trunk/percentage of fat in the leg, and trunk/limb fat mass ratios increased with age in both genders, with the values peaking in women around 65 yr of age (Fig. 1). In men, lean mass/heightheight2 and appendicular lean mass/height2 decreased with age, and this decrease accelerated after 40 yr of age. However, lean mass/heightheight2 and appendicular lean mass/height2 in women increased with age, peaking at around 55 yr of age. Appendicular lean mass/total lean mass decreased with age in both the genders (Fig. 1).
We employed the BMI classification reported in the WHO technical report (15) to establish similar classifications for FMI by calculating the prevalence for each of the WHO BMI classification thresholds (e.g., mild thinness, normal, overweight, obese class 1, etc.) at the age of 25 yr, as in a previous study (10). We have included the results of the present study to a table (Table 3) published in the article by Kelly et al. (10). The prevalence of the BMI classification thresholds varied widely in the 4 ethnic groups (from the NHANES and KNHANES) (Table 4). However, FMI classification ranges were similar for the 4 ethnic groups (from the NHANES and KNHANES). Interestingly, there were large differences in the FMI between genders. Women had higher FMI for all classification categories. When we defined overweightness and obesity according to FMI classification (Table 5) (10), the prevalence rates of overweightness and obesity in men were 50.6% (FMI > 6 kg/m2) and 6.1% (FMI > 9 kg/m2), respectively. In women, the prevalence rates of overweightness and obesity were 36.6% (FMI > 9 kg/m2) and 2.7% (FMI > 13 kg/m2) (Fig. 2).
Many studies have assessed body compositions, but a standard and nationally representative source of body composition reference values for Korea and other nations is not available. Therefore, the practical application of these studies is limited. Recently, Kelly et al. (10) reported reference values based on a nationally representative NHANES data set for the United States. Data for these reference values were acquired using well-established DXA technology. In the present study, we report references values for Korean body composition based on a nationally representative KNHANES data set that were acquired using equally well-established DXA technology, and utilizing the same parameters established by Kelly et al. The references values from the NHANES data set did not include an Asian ethnic population, but did include non-Hispanic Whites, non-Hispanic Blacks, and Mexican-Americans. In addition to its significance as a Korean national data set, our study builds on an established standard to help create a body of comparable data in the field of body composition analysis, and acts as a standard reference value for an Asian population.
Previous studies showed that Asian populations have higher fat mass and lower lean mass than other ethnic populations (16-18). We compared the FMI, fat percentage, lean mass/height2, and appendicular lean mass/height2 of the Korean population with those of the populations categorized in the NHANES data (10). The Korean population was found to have a relatively lower FMI, fat percentage, lean mass/height2, and appendicular lean mass/height2 than the other ethnic populations. From the NHANES references values, the FMI and fat percentage in both the genders increased with increasing age (10). However, in a previous study, the fat percentages of Asian Indian women weakly correlated with age, while those of Asian Indian men was unrelated to age (16). In this study, age had no correlation with FMI, but it was positively correlated with the fat percentage in men. In Korean women, fat mass/height2 and fat percentage showed positive correlation with age, in agreement with a previous study (19) (Fig. 1, Table 2).
Our data demonstrate significant differences in lean mass and appendicular lean mass between Korean men and women. In Korean men, appendicular lean mass (R = -0.324, P < 0.001) was strongly negatively correlated with age. Appendicular lean mass decreased sharply after 40 yr of age. In Korean women, age was positively related to appendicular lean mass (R = 0.068, P < 0.001). Fat percentages in men increased with age. In men, age was negatively related to lean mass and unrelated to fat mass. We concluded that the correlation between fat percentage and age in men was mainly due to changes in the lean mass.
Recently, Kelly et al. (10) introduced a classification scheme called FMI. The prevalence rates of obesity and overweightness by BMI according to the WHO technical classifications were different from those of other ethnicities included in the NHANES (Table 4). In Korea, overweightness and obesity are defined by BMI values of > 23 and > 25, respectively, according to the Asia-Pacific obesity guidelines, which are based on ethnic differences. However, when we define overweightness and obesity according to FMI classification (10), the prevalence rate of obesity and overweightness were similar to those of other ethnicities in the NHANES (Fig. 2) than those according to BMI classification. However, the metabolic significance of FMI classification was not studied. Therefore, further studies are needed.
The worldwide concern about sarcopenia, i.e., the degenerative loss of skeletal muscle mass with age, has increased. A study involving elderly subjects showed that sarcopenia was an indicator of self-reported physical disability in elderly men and women, independent of other covariates such as age, obesity, ethnicity, and income levels (18). DXA is the only widely available method to provide regional measurements of fat and lean mass. Therefore, DXA measure of appendicular lean mass/height2 is a useful tool for the diagnosis of sarcopenia. Sarcopenia was previously defined as a value of appendicular lean mass/height2 less than 2 standard deviations (SD), below the sex-specific normal mean of a younger reference group (19), or the 2 lower quintiles in the study population (16, 18). The reference curves for appendicular lean mass/height2 are presented in this study. According to our reference curves, sarcopenia in Korea is defined as an appendicular lean mass below 5.748 kg/m2 in men when the young reference group is defined as a group of 25-yr-old men. If the young reference group is defined as 20-39-yr-old men (mean, 7.952 ± 0.887, n = 1,456), sarcopenia in Korea is defined as an appendicular lean mass below 5.519 kg/m2. When we compared the Korean male sarcopenia value (< 5.75 kg/m2) with those of the NHANES (White male < 6.8 kg/m2, Black male < 7.0 kg/m2, and Hispanic male < 7.0 kg/m2), the former was significantly lower than the values for the other ethnicities studied in the NHANES. In women, the sarcopenia values were defined as an appendicular lean mass less than 3.956 kg/m2 (the young reference group was a group of 25-yr-old women) or 4.244 kg/m2 (the young reference group was a group of 20-39-yr-old women). These values were also significantly lower than those of the other ethnicities included in the NHANES (White male < 5.2 kg/m2, Black male < 6.0 kg/m2, and Hispanic male < 5.3 kg/m2). The lean mass of the trunk is primarily composed of solid organ matter, while the appendicular lean mass is primarily composed of muscles. Therefore, appendicular lean mass/trunk lean mass could indicate muscular changes in the body's composition, which are independent of stature. According to the ratio of appendicular lean mass to trunk lean mass, sarcopenia is defined as being < 0.834 in men and 0.710 in women (less than 2 SD below the means of the young reference groups defined as groups of 25-yr-old men and women, respectively). However, validation of these results requires further studies.
In the percentile curve, the data regarding BMI, FMI, waist circumference, and fat percentage were skewed, especially in the 20-40-yr-old age group (Fig. 1). These trends were more prominent in the FMI and fat percentage data of the young population (Fig. 1). By contrast, the data regarding the ratio of percentage of fat in the trunk to that in the leg, trunk/limb fat mass ratio, and appendicular lean mass/height2 were not skewed in the 20-40 yr old population (Fig. 1). These patterns possibly reflect the increase in the prevalence rate of severe obesity among the Korean youth.
This study represents the first nationally representative analysis conducted in Asia. The results clearly illustrate a divergence from the results found in the NHANES, and can be explained to be caused by ethnicity, and thus, genetic differences or perhaps other yet undefined causes. Korean populations have relatively lower lean mass as well as "not-high" fat mass compared to other ethnic populations. Fat mass gain is not a prominent finding, but central distribution of fat is a prominent finding associated with age. In addition, lean mass parameters, in particular, appendicular lean mass/trunk lean mass, decrease with age. It is plausible that these changes might be related to metabolic changes. We hope that the findings of this study help improve our understanding of the relationships between body composition and metabolic changes.
Figures and Tables
Fig. 1
Percentile curves; the mean, 3rd, 10th, 25th, 75th, 90th, and 97th percentiles superimposed on raw data values. BMI (kg/m2), waist circumference (cm), FMI (kg/m2), fat percentage (%), trunk/legs fat percentage ratio, trunk/limb fat mass ratio, appendicular lean mass/height2, and appendicular/trunk lean mass ratio are considered. BMI, body mass index; FMI, fat mass index.

Fig. 2
Prevalence of overweightness and obesity in Korea, based on FMI as a function of age (A, men; B, women). FMI values are listed in Table 4. FMI, fat mass index.

Table 2
Mean and standard deviation values of body composition parameters according to gender and age
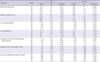
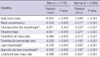
Table 3
List of reference curves generated from the 2008 KNHANES DXA whole body data set and correlated with age (years)
ACKNOWLEDGMENTS
The authors thank the Korea Centers for Disease Control and Prevention, who performed the KNHANES.
AUTHOR SUMMARY
Characteristics of Body Fat, Body Fat Percentage and Other Body Composition for Koreans from KNHANES IV
Sangmo Hong, Han Jin Oh, Hoon Choi, Jung Gu Kim, Sung Kil Lim, Eun Kyung Kim, Eun Young Pyo, Kyungwon Oh, Young Taek Kim, Kevin Wilson and Woong Hwan Choi
We made the reference of Korean body composition from KNHANES IV. When we defined obesity according to the FMI classification, the rates of obesity were 6.1% (FMI > 9 kg/m2) in men and 2.7% (FMI > 13 kg/m2) in women. It is concluded that the muscle mass decreases and obesity increases with aging in Korean men, whereas both fat mass and obesity increase with aging in Korean women.
References
1. Prentice AM. The emerging epidemic of obesity in developing countries. Int J Epidemiol. 2006. 35:93–99.
2. WHO. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000. 894:i–xii. 1–253.
3. Cho M, Park JS, Nam J, Kim CS, Nam JH, Kim HJ, Ahn CW, Cha BS, Lim SK, Kim KR, Lee HC, Huh KB. Association of abdominal obesity with atherosclerosis in type 2 diabetes mellitus (T2DM) in Korea. J Korean Med Sci. 2008. 23:781–788.
4. Kim JY, Chang HM, Cho JJ, Yoo SH, Kim SY. Relationship between obesity and depression in the Korean working population. J Korean Med Sci. 2010. 25:1560–1567.
5. Kennedy AP, Shea JL, Sun G. Comparison of the classification of obesity by BMI vs. dual-energy X-ray absorptiometry in the Newfoundland population. Obesity (Silver Spring). 2009. 17:2094–2099.
6. Heymsfield SB, Gallagher D, Mayer L, Beetsch J, Pietrobelli A. Scaling of human body composition to stature: new insights into body mass index. Am J Clin Nutr. 2007. 86:82–91.
7. Prior BM, Cureton KJ, Modlesky CM, Evans EM, Sloniger MA, Saunders M, Lewis RD. In vivo validation of whole body composition estimates from dual-energy X-ray absorptiometry. J Appl Physiol. 1997. 83:623–630.
8. Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, Zimmet P, Son HY. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006. 368:1681–1688.
9. Wulan SN, Westerterp KR, Plasqui G. Ethnic differences in body composition and the associated metabolic profile: a comparative study between Asians and Caucasians. Maturitas. 2010. 65:315–319.
10. Kelly TL, Wilson KE, Heymsfield SB. Dual energy X-Ray absorptiometry body composition reference values from NHANES. PLoS One. 2009. 4:e7038.
11. Schoeller DA, Tylavsky FA, Baer DJ, Chumlea WC, Earthman CP, Fuerst T, Harris TB, Heymsfield SB, Horlick M, Lohman TG, Lukaski HC, Shepherd J, Siervogel RM, Borrud LG. QDR 4500A dual-energy X-ray absorptiometer underestimates fat mass in comparison with criterion methods in adults. Am J Clin Nutr. 2005. 81:1018–1025.
12. Bonnet E, Delpierre C, Sommet A, Marion-Latard F, Hervé R, Aquilina C, Labau E, Obadia M, Marchou B, Massip P, Perret B, Bernard J. Total body composition by DXA of 241 HIV-negative men and 162 HIV-infected men: proposal of reference values for defining lipodystrophy. J Clin Densitom. 2005. 8:287–292.
13. Law M, Puls R, Cheng AK, Cooper DA, Carr A. Evaluation of the HIV lipodystrophy case definition in a placebo-controlled, 144-week study in antiretroviral-naive adults. Antivir Ther. 2006. 11:179–186.
14. Pan H, Cole TJ. A comparison of goodness of fit tests for age-related reference ranges. Stat Med. 2004. 23:1749–1765.
15. WHO. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995. 854:1–452.
16. Rush EC, Freitas I, Plank LD. Body size, body composition and fat distribution: comparative analysis of European, Maori, Pacific Island and Asian Indian adults. Br J Nutr. 2009. 102:632–641.
17. Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr. 2000. 72:694–701.
18. Wulan SN, Westerterp KR, Plasqui G. Ethnic differences in body composition and the associated metabolic profile: a comparative study between Asians and Caucasians. Maturitas. 2010. 65:315–319.
19. Chung S, Song MY, Shin HD, Kim DY, He Q, Heshka S, Wang J, Thornton J, Laferrère B, Pi-Sunyer FX, Gallagher D. Korean and Caucasian overweight premenopausal women have different relationship of body mass index to percent body fat with age. J Appl Physiol. 2005. 99:103–107.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download