Abstract
Health risk appraisal (HRA) is a tool for determining health risk factors and motivating individuals to maintain a healthy lifestyle. We performed this study to describe the HRA algorithm and evaluate the accuracy of an HRA program for 10-yr mortality prediction in Korean men. We used data derived from periodic health examinations of 116,927 male public officials and school personnel aged 20 or older. Risk age and the difference between risk age and calendar age were calculated. We obtained the hazard ratio (HR) of 10-yr mortality according to the calculated age difference. Of the 116,927 subjects, 1,900 (1.6%) died during the 10 yr after the 1992 medical examinations. The HR of 10-yr mortality increased significantly with age difference. Compared with the HR in the reference group (age difference below 2 yr), the HR in the group with a 2- to 6-yr age difference was 1.20 (95% confidence interval [CI]: 1.05 to 1.38) and HR in the group with more than 7-yr age difference was 1.35 (95% CI: 1.14 to 1.75). Risk age is a relatively good predictor of 10-yr mortality in Korean men and may be useful in identifying high-risk middle-aged men for health interventions.
A healthy lifestyle plays an important role in lowering all-cause and cause-specific mortality, such as mortality due to heart disease, cancer, or stroke. The combination of smoking, being overweight, lack of physical activity, and poor diet was associated with 55% to 60% of deaths from all causes in several cohort studies (1, 2). Nevertheless, researchers have found that public awareness of the impact of lifestyle on cancer and heart disease is low (3-5).
Unhealthy lifestyle factors such as smoking, alcohol abuse, physical inactivity, and poor diet frequently co-occur, and clustering of multiple risk behaviors can be more harmful to health. Given the increase in efforts to change multiple risk behaviors, methods are needed to quantify and evaluate health behaviors within individuals and population (6).
One method for evaluating multiple health risks is health risk appraisal (HRA), developed by Alexander (7). The original purpose of HRA was to educate people about their health risks and change their unhealthy behaviors. HRA uses risk factors identified from various epidemiological studies, such as family history, blood pressure, and smoking habits, to assess an individual's 10-yr mortality risk in the form of "risk age", defined as the age that corresponds to an individual's risk of death within 10 yr.
In 2003, the HRA committee of the Korean Academy of Family Medicine developed an HRA program for Koreans based on domestic epidemiological studies and mortality data (8-11). The Korean National Health Insurance Corporation (KNHIC) is a public health insurer that arranges for periodic medical examinations of the insured. Since 1989, most Koreans have been insured by the social health insurance system and encouraged to participate in periodic health examination. However, the overall rate of medical examination is only about 20%, with the exception of public officials and school personnel, for whom the health examinations are mandatory. The KNHIC adopted the HRA program to encourage people to undergo medical examinations and to increase individuals' motivation to change their risk factors.
Though HRA was originally developed as an educational tool, establishing its validity is important if it is to be used for healthcare program planning and evaluation, identifying high-risk populations, and recruiting participants for health promotion programs. Use of HRA in designing benefit plans and managing and evaluating programs will likely continue to increase as organizations seek to control costs.
The purpose of this study was to describe the HRA program of KNHIC and evaluate the predictive accuracy of HRA using periodic health examination data from Korean men.
The KNHIC provides health insurance to Koreans and their dependents. All insured workers are recommended to undergo a physical examination once every 2 yr. The HRA program is performed at the same time as the examination, and HRA findings are given to patients along with results of the health checkup.
We developed the HRA program according to the methods of Alexander (7) in the book "SPM handbook of Health Assessment Tools". Though concrete evidence was at first lacking for using the methods, the US Centers for Disease Control and Prevention established the validity of HRA by using the above methods to predict 10-yr mortality (18, 19).
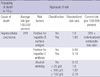
The top 10 leading causes of death for an individual's age and sex group were identified according to the Korean death statistics by cause (103 items), sex, and age in 2000. We especially focused on common, but important and preventable diseases among identified causes of death. Table 1 represents the disease selection process in defining the HRA program.
Insured individuals are recommended to undergo standardized health examinations every 2 yr at local hospitals. Participants in the study reported their family histories of stroke, cardiovascular disease, diabetes, and hypertension as well as their own alcohol consumption, smoking habits, and exercise frequency. Examiners recorded height, weight, and blood pressure while subjects were wearing light clothing. Serum glucose and total cholesterol levels were obtained after a 12-hr fast. Each hospital followed internal and external quality control procedures in accordance with the Korean Association of Laboratory Quality Control.
We selected risk factors from the national health examination data because HRA was developed for complementary presentation in health examination result counseling. Risk factors were body mass index (kg/m2); smoking; drinking; lack of exercise; family history of stroke, cardiovascular disease, or diabetes; and elevated blood pressure, serum glucose, or cholesterol levels.
We then searched relative risks of risk factors in each cause of death. A systemic search of literature from January 1990 to 2005 on relative risks of each factor was performed by the HRA committee of the Korean Academy of Family Medicine. We searched cohort studies, systemic reviews, and meta-analyses between risk factors and causes of death through MEDLINE, EMBASE, Web of Science, KoMCI, KoreaMED, Korean Medical Database, and Korean studies Information Service System. We gave priority to Korean cohort studies, but if we could not find the relative risks in domestic studies, we searched other cohort studies or case control studies. It took 4 months for seven family physicians to search and review relative risk of risk factors on each causes of death. Table 2 shows a sample of an identified risk factor and its relative risk.
Total mortality risk and cause-specific mortality risk per 100,000 were arranged by sex and age according to Korean death statistics in 2003. This is called Geller-Gesner table, which compiles the average 10-yr mortality rates for leading causes of death. The reference population for the HRA was an average age- and sex-matched Korean population, so reference state was not always ideally healthy. For example, if a 45-yr-old man is a 10 pack year smoker, then his relative risk for developing ischemic stroke is 2.2 compared with a nonsmoking 45-yr-old man. If his risk is compared with the population average risk in 45-yr-old men and the average smoking prevalence in the population is 69.3%, then his standardized risk is 1.01. The standardized risk is calculated by log transformation of relative risk and setting the average population risk to zero (10). Prevalence of each risk factor was derived from the Korea National Health and Nutrition Examination Survey in 2001. If the standardized risk of each risk factor was lower than 1.0, then it was multiplied to yield a composite risk ratio. If the standardized risk was greater than 1.0, 1.0 was subtracted from standardized risk to yield composite risk ratios. In the example presented in Table 3, if a man is a hepatitis B antigen carrier, but negative for the hepatitis C antibody, and drinks 30 g per day of alcohol, each risk ratio is as follows: 1.82, 0.98, and 1.82. His composite risk ratio is calculated by (1.82-1) + 0.98 + (1.82-1) = 2.62.
The 10-yr predicted risk of mortality was calculated for each leading cause of death by multiplying the individual's relative risk by the population's average risk as presented in Table 3. Probabilities were then summed to yield the total risk of dying during the next 10 yr, which was called appraised risk (12). Appraised risk is the 10-yr predicted mortality risk, presented as the number of deaths per 100,000 persons. If data on important risk factors, such as being a carrier of hepatitis B viral antigen for liver cancer, were needed to calculate appraised risk but were not available, the HRA program assigned population norms.
Health examination findings are presented by risk age and modifiable age. Risk age was defined as the age of the average population with the same total appraised risk as an individual's appraised risk calculated by HRA program. To arrive at risk age, an individual's appraised risk was compared with the population average risk for the same age and sex. If the appraised risk equaled the population average, then the risk age was the same as the calendar age. A higher appraised risk yielded an older risk age, and a lower appraised risk yielded a younger risk age. The age difference was calculated from risk age minus calendar age.
Modifiable age was defined as achievable risk age by modifying risk factors. For example, if a 45-yr-old man is a smoker, his risk age calculated by the HRA program would be 48 yr, an age difference of 3 yr older. If he quits smoking, his modifiable age could be 43 yr, 2 yr less than his calendar age. HRA motivates people to change their unhealthy behaviors and to stay young by giving risk age and modifiable age.
We used periodic health examination data obtained in 1992 from 121,261 male public officials and school personnel ages 20 to 63 yr-a large enough sample to calculate risk age. We excluded female participants because women ages 20 to 29 yr accounted for 52% of all female participants and because the number of women who smoked or drank alcohol was too small for statistical analysis. Also the most common cause of death in young women was suicide, and its risk factors are stressful life events, depression, or family history of mental illness, which were not available in our data.
HRA is usually intended to be used in persons without acute disease or uncontrolled chronic illness. However, information on disease status was not available in this study, thus we excluded subjects with laboratory data that were objectively assessed to indicate the possibility of acute or uncontrolled chronic disease. Exclusion criteria were total cholesterol level above 300 mg/dL (13), fasting blood glucose level above 250 mg/dL (13), systolic blood pressure above 180 mmHg, and diastolic blood pressure above 110 mmHg (14). Among 121,262 men, 4,335 men were excluded by the above criteria. A total of 116,927 men were included in the final analysis.
We calculated the predicted 10-yr mortality risk and risk age for each individual from data gathered during the 1992 periodic health examinations. The following age groups were used: 20 to 29 yr, 30 to 39 yr, 40 to 49 yr, 50 to 59 yr, and 60 yr or more. To determine whether risk age was a good predictor of mortality, we calculated age differences using the difference between individual risk age and 1992 calendar age. If the age difference was 0, the person was considered to have average risks compared with the same age and sex population. If the age difference was positive, the person had higher risks than the average population.
Age differences were also categorized as follows: 2 yr or less, 2 to 6 yr, and 7 yr or more. Actual mortality data were linked with health checkup data using national mortality statistics in 2002 (15) and identification numbers were deleted so we could assess de-identified data.
To identify predictors of death, Cox proportional hazards analysis was performed, and if variables achieved a P value < 0.10 on univariate analysis, they were tested in a stepwise multiple regression model with 95% confidence intervals (CIs). All analyses were performed using SPSS for Windows (Version 11.0, SPSS Inc., Chicago, IL, USA), and P < 0.05 was considered statistically significant.
This study was exempted from review by the institutional review board of the Seoul National University Bundang Hospital (B-0604/032-021) because researchers only accessed a de-identified database that included age, sex, health checkup examination results, and death date with diagnosis of cause of death.
Of the 116,927 subjects in the study, 1,900 (1.6%) died in the 10-yr period following the 1992 medical examinations. Mean (standard deviation [SD]) age for the total study population was 40.2 (9.5) yr, and the average age difference was -0.1 (4.1) yr (i.e., calendar age was greater than risk age). High percentages of the population had alcohol problems (43.2%) or smoked (60.5%). Only 26% of the total population engaged in regular exercise. Mean body mass index was 23.2 (2.5).
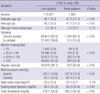
Table 4 shows the differences in risk factors between subjects who remained alive after 10 yr (live subjects) and subjects who died within that time (dead subjects). Mean age in the latter group was 47.2 (10.1) yr, significantly higher than that of the former group, whose mean age was 40.1 (9.5) yr. Blood pressure, serum glucose level, and total cholesterol level were also slightly higher in the group of dead subjects, but the differences were clinically insignificant. Health behavior risk factors such as smoking, heavy drinking, and lack of exercise showed similar distributions, but the differences were statistically significant.
Table 5 presents the results of the Cox hazard regression analysis relating the likelihood of death to increasing age and age difference. The table shows the distribution of risks (hazard ratio [HR]) of death adjusted by risk factors associated with mortality. The reference group had the lowest age difference (less than 2 yr).
Compared with the referent group, HR in the group with an age difference of 2 to 6 yr was 1.20 (95% CI: 1.05 to 1.38) and HR of age difference group more than 7 yr was 1.35 (95% CI: 1.14 to 1.75). As age difference increased, there was increased tendency of HR for 10-yr mortality (P = 0.015).
Studies focusing on the validity of HRA have concentrated on the ability of HRA to accurately predict death within the next 10 to 20 yr (16-21). Thus, a focus is placed on the accuracy of the algorithms used. These algorithms depend on three sources of data: death certificate data for establishing the average probability of each cause of death for every combination of age and sex, epidemiological and clinical data for assigning values to risk factors, and respondents' self-reports of risk factors (16).
In this study, we found that predicted mortalities were independently associated with actual mortalities in Korean men. When the age difference increased, the HR of 10-yr mortality also increased significantly. These results suggest that age differences can be useful for placing people in risk categories. This idea is reflected in findings of the Tecumseh Community Health Study (19), in which 3,135 persons were followed from 1959 to 1974. The authors classified individuals into one of five categories, defined by taking the 1959 calendar age and subtracting the calculated risk age (which is the reverse of our age difference). The five categories were +2 to +5, -1 to +1, -5 to -2, -10 to -6, and less than -10. The percentages of women who died within 20 yr in these five categories were 3.0%, 2.8%, 8.9%, 15.5%, and 30.5%, respectively; and the percentages of men were 0.0%, 2.8%, 9.8%, 29.0%, and 36.2%. In our study, HRA was also found to accurately classify individuals into appropriate categories. We also performed sensitivity analysis in grouping age differences and the results showed no significant differences in predicting 10-yr mortality. But trends in hazard ratio showed a better correlation with mortality for the groups with less than 2 yr, +2 to +6 yr, and more than 6 yr age differences.
HRA tended to underestimate actual risk in another study (16), which compared HRA mortality prediction derived from six populations and found that although the HRA program predicted better than chance, it underestimated actual mortality. Other studies indicated that the HRA program is more accurate for predicting future events than age, sex, or race tables (18, 19).
In our study, age difference was not different between live and dead subjects. The HRA program was designed to screen high risk groups within a population and motivate individuals to change their risk behaviors. Most people had the same risk age with calendar age, and its difference was negligible in most people. But in the high risk group with more than 2 yr age difference, HRA program was a relatively good predictor of actual mortality.
A recent study showed that if risk age by the HRA program is lower, health-related quality of life is better among middle-aged men (22). Consequently, the HRA program can also be used as an indicator of health-related quality of life.
When investigating the accuracy of HRA, the validity of self-reported risk factors should be considered. A number of studies have assessed the validity of self-report questionnaire data (23, 24). Self-reported physical activity levels have been found to show good correlation with physiological measures of maximal oxygen consumption and energy expenditure (25), especially metabolic equivalent values of 6 or more and vigorous activity. Moreover, cotinine analysis of urine among the US Navy recruits showed only a 1% discrepancy with self-reported smoking status (26).
Another study found good correlations between self-reported risk scores for cigarette smoking and relative weight but found that reports on physical activity, blood pressure, and cholesterol were frequently inaccurate (21, 27). Our study depended on a self-report questionnaire for smoking, alcohol consumption, and exercise data, but objective laboratory data were used for height, weight, blood pressure, fasting blood glucose, and cholesterol.
Limitations of our study are as follows. The HRA program was created in 2003 and uses 10-yr mortality for computing risk age. To perform validity testing with available data, we had to use 1992 health examination data and death statistics until 2002, which did not exactly reflect causes of death or relative risks. We searched trends of changing causes of death in 1992 and 2003 by Korean death statistics. The greatest surge was seen in coronary heart disease, which increased by 58% during the 11 yr. Also, lung cancer showed a 48% rate of increase. On the other hand, cerebrovascular disease showed a slight decline (17%) during the same period. Consequently our HRA program possibly overestimated risk age. Further, we used a limited occupational group because data from other population were not available. This could affect generalizability of the study. Additionally, our data did not include disease status or medical care data, and thus we were unable to exclude individuals with chronic disease, although we excluded those with extreme laboratory values.
We also excluded female participants because the questionnaire used was limited in terms of women's mortality risk factors (e.g., it did not include questions about menstrual history, family history of breast cancer, or use of oral contraceptives). Pregnancy can affect women's mood and cognition, which can in turn affect fetal health (28). In particular, women's motivation for healthy behaviors needs to be evaluated with a psychosocial appraisal because this part of health differs from men's health risk (29). Thus, risk factors concerning the health and diseases of women, adolescents, and the elderly should be addressed in HRA questionnaires before studies on HRA validity in these population groups are conducted. Moreover, this should be linked to the development of a comprehensive HRA program for Koreans.
Continued development of technology and feedback concerning behavioral changes will be necessary before HRA can reach its full potential. Also required will be efforts to study HRA's effectiveness in health promotion, in predicting health-care costs, and as an indicator of health-related quality of life.
In conclusion, risk age calculated in the KNHIC HRA program is a relatively good predictor of 10-yr mortality in Korean men and may be a useful tool for identifying high-risk middle-aged men for health interventions. Further efforts will be needed to develop a comprehensive HRA program and establish its validity.
Figures and Tables
ACKNOWLEDGMENTS
The authors thank Professor Emeritus Bong-Yul Huh of Seoul National University for his helpful comments on the first draft of this manuscript. We thank the Korean National Health Insurance Corporation (KNHIC) for permitting us to use the periodic health examination data.
AUTHOR SUMMARY
Predictive Accuracy of a Health Risk Appraisal Program Using Mortality Risk Age in 116,927 Korean Men
Ju-Young Kim, Byung-Joo Park, Yoon Kim, Jin-Ho Park, and Be-Long Cho
Health risk appraisal (HRA) developed by Korean National Health Insurance Corporation (KNHIC) is a tool for evaluating health risk factors and motivating individuals to maintain a healthy lifestyle. Here we describe the HRA algorithm of KNHIC and evaluate the predictive accuracy of an HRA program for 10-yr mortality prediction in Korean men. Of the 116,927 subjects, 1,900 (1.6%) died during the 10 yr after the 1992 medical examinations. As the difference between risk age and actual age increases, the 10 yr mortality increased significantly. The risk age in HRA is a relatively good predictor of 10 yr mortality in Korean men.
References
1. Knoops KT, de Groot LC, Kromhout D, Perrin AE, Moreiras-Varela O, Menotti A, van Staveren WA. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA. 2004. 292:1433–1439.
2. van Dam RM, Li T, Spiegelman D, Franco OH, Hu FB. Combined impact of lifestyle factors on mortality: prospective cohort study in US women. BMJ. 2008. 337:a1440.
3. Inoue M, Iwasaki M, Otani T, Sasazuki S, Tsugane S. Public awareness of risk factors for cancer among the Japanese general population: a population-based survey. BMC Public Health. 2006. 6:2.
4. Wardle J, Waller J, Brunswick N, Jarvis MJ. Awareness of risk factors for cancer among British adults. Public Health. 2001. 115:173–174.
5. Breslow RA, Sorkin JD, Frey CM, Kessler LG. Americans' knowledge of cancer risk and survival. Prev Med. 1997. 26:170–177.
6. Prochaska JJ, Velicer WF, Nigg CR, Prochaska JO. Methods of quantifying change in multiple risk factor interventions. Prev Med. 2008. 46:260–265.
7. Alexander G. Hyner GC, Peterson KW, Travis JW, editors. Health Risk Appraisal. SPM Handbook of Health Assessment Tools. 1999. Pittsburgh: Society of Prospective Medicine;139–142.
8. Shin HC. Health Risk Appraisal-Need assessment and general health status appraisal tool for adults. J Korean Acad Fam Med. 2003. 24:4 Suppl. S339–S348.
9. Baek YJ. Definition of health risk appraisal. J Korean Acad Fam Med. 2002. 23:11 Suppl. S260–S267.
10. Kim CH. Methods of health risk appraisal. J Korean Acad Fam Med. 2002. 23:11 Suppl. S286–S290.
11. Lee JH. Issues and improvements in development of Korean health risk appraisal. J Korean Acad Fam Med. 2002. 23:11 Supple. S291–S295.
12. Alexander G. Health risk appraisal. Int Electron J Health Educ. 2000. 3(special):133–137.
13. Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL. Harrison's Principles of Internal Medicine. 2005. 16th ed. New York: McGraw Hill.
14. Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Boudier HA, Zanchetti A. ESH-ESC Task Force on the Management of Arterial Hypertension. 2007 ESH-ESC practice guidelines for the management of arterial hypertension: ESH-ESC task force on the management of arterial hypertension. J Hypertens. 2007. 25:1751–1762.
15. Hagihara A, Kusaka Y, Morimoto K, Tamura T, Matsuura Y. Health risk appraisal (HRA) and its educational effect on bank employees. Ind Health. 1992. 30:61–64.
16. Safer MA. An evaluation of the health hazard appraisal based on survey data from a randomly selected population. Public Health Rep. 1982. 97:31–37.
17. Katz D, Foxman B. How well do prediction equations predict? Using receiver operating characteristic curves and accuracy curves to compare validity and generalizability. Epidemiology. 1993. 4:319–326.
18. Gazmararian JA, Foxman B, Yen LT, Morgenstern H, Edington DW. Comparing the predictive accuracy of health risk appraisal: the Centers for Disease Control versus Carter Center program. Am J Public Health. 1991. 81:1296–1301.
19. Foxman B, Edington DW. The accuracy of health risk appraisal in predicting mortality. Am J Public Health. 1987. 77:971–974.
20. Smith KW, McKinlay SM, Thorington BD. The validity of health risk appraisal instruments for assessing coronary heart disease risk. Am J Public Health. 1987. 77:419–424.
21. Smith KW, McKinlay SM, McKinlay JB. The validity of health risk appraisals for coronary heart disease: results from a randomized field trial. Am J Public Health. 1991. 81:466–470.
22. Jang JI, Kim CH, Shin HC, Park YW, Sung EJ, Lee EJ, Choi DH, Paik YJ, Kim AJ. The relationship between health risk appraisal and health-related quality of life among middle-aged men. J Korean Acad Fam Med. 2006. 27:534–539.
23. Edington D, Berlin J. Correlates of selected health risk appraisal input questions with physiological and psychosocial indicators. Proceedings of the 18th Annual Meeting of the Society of Prospective Medicine. 1982. Sewickley, PA: Society of Prospective Medicine.
24. Berlin J, Edington D. Predicting physiological parameters from questionnaire data. Proceedings of the 19th Annual Meeting of the Society of Prospective Medicine. 1983. Sewickley, PA: Society of Prospective Medicine.
25. Kurtze N, Rangul V, Hustvedt BE, Flanders WD. Reliability and validity of self-reported physical activity in the Nord-Trøndelag Health Study: HUNT 1. Scand J Public Health. 2008. 36:52–61.
26. Pokorski TL, Chen WW, Bertholf RL. Use of urine cotinine to validate smoking self-reports in U.S. Navy recruits. Addict Behav. 1994. 19:451–454.
27. Smith KW, McKinlay SM, McKinlay JB. The reliability of health risk appraisals: a field trial of four instruments. Am J Public Health. 1989. 79:1603–1607.
28. DiPietro JA, Ghera MM, Costigan K, Hawkins M. Measuring the ups and downs of pregnancy stress. J Psychosom Obstet Gynaecol. 2004. 25:189–201.
29. Ho R, Davidson G, Ghea V. Motives for the adoption of protective health behaviours for men and women: an evaluation of the psychosocial-appraisal health model. J Health Psychol. 2005. 10:373–395.
30. Jee SH, Ohrr H, Sull JW, Samet JM. Cigarette smoking, alcohol drinking, hepatitis B, and risk for hepatocellular carcinoma in Korea. J Natl Cancer Inst. 2004. 96:1851–1856.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download