Abstract
The purpose of this study was to investigate the association between body mass index (BMI) and the prevalence of wheeze using nation-wide cross-sectional study in Korean children. Total 50,200 children from 427 elementary schools were randomly selected according to residential areas (metropolitan, provincial, rural, and industrial areas) by the cluster sampling method. The International Study of Asthma and Allergies in Childhood (ISAAC) questionnaires were used to measure the prevalence of wheeze. Among 31,026 respondents, 25,322 were analyzed. BMI was classified into quartiles based on BMI-for-age percentile. In all residential areas, pets at home and visible mold or moisture were associated with an increased prevalence of wheeze in both genders. However, other living environment factors were not consistently associated among residential areas and gender. Among girls, lowest BMI was negatively associated with prevalence of wheeze and highest BMI was positively associated in all residential areas. In multilevel logistic regression analysis, environmental tobacco smoking exposure, pets at home, visible mold or moisture, and being in the lowest and highest BMI quartile were significantly associated with the prevalence of wheeze in both genders. BMI has become an important risk factor for asthma symptoms among Korean children.
The prevalence of asthma and obesity has increased substantially during the last several decades in many countries. In the Republic of Korea (ROK), the prevalence of childhood obesity (5.4% in 1998 to 11.3% in 2001) and asthma (2.7% in 1995 to 5.3% in 2000) also have increased (1-3). Due to their increased prevalence, both obesity and asthma were recognized as a major public health issue in the ROK. Many epidemiologic studies have shown an association between obesity and asthma in both adults and children (4-6). However, obesity-asthma link or the underlying mechanism remains still controversial (5).
In the ROK, few studies have investigated the association between childhood obesity and asthma or asthma symptoms (1, 7, 8): these studies had several limitations in study design and analysis because most were hospital-based, case-control studies with small sample sizes. Furthermore, in cross-sectional studies, the contextual effect of residential areas was not considered in the sampling method and analysis. Since both lifestyle and indoor or outdoor environment associated with a residential area may also confound any association between obesity and asthma (9, 10), factors associated with the residential area must be considered in the study design and analysis.
In the present study, we investigated the association between childhood obesity based on body mass index (BMI) and self reported asthma symptoms among elementary school children (mostly 8-11 yr old) using nation-wide cross-sectional data that includes characteristics of residential areas in the ROK.
Data on the geographic location and number of students of all elementary schools (6,279 schools) in 2006 were acquired from the Ministry of Education, Science and Technology (MEST) of the ROK. To obtain a representative population from elementary schools in each residential area, a clustered random sampling method was used. Residential areas were divided into four groups: metropolitan, provincial, rural, and industrial areas. Ten percent of elementary schools in each group, of which the number in a class was over three, were randomly selected, with the exception of schools in industrial area. Details of the study design have been described previously (3). In each elementary school, one class from each grade (from grades 3 to 5; 8-11 yr old) was randomly selected.
Letters of invitation, informed consent requests, and questionnaires were mailed to the selected elementary schools from October through November 2006. Parents or caregivers of the children were asked to complete the questionnaire. Among 50,200 participants from 427 elementary schools, a total of 31,026 (61.8%) students from 363 (85.0%) elementary schools responded to the mailing survey.
In this study, the Korean version of the International Study of Asthma and Allergies in Childhood (ISAAC) written questionnaire (WQ) for asthma following the guidelines suggested by ISAAC was used. Detailed characteristics of the Korean version of the ISAAC WQ have been reported previously (1, 7). ISAAC WQ was validated and used to identify the children currently suffering from the symptoms of asthma. In this study, prevalence of wheeze is defined as a history of at least 1 attack of wheezing during the last 12 months. The questionnaire included questions on demography (age, gender, height, and weight), monthly electricity bill (as a proxy indicator of socio-economic status), environmental tobacco smoking (ETS) exposure, and potential allergens (pets at home, presence of visible mold or moisture) including experiences over one's lifetime and in the last 12 months. Questions on living environments such as residential area, history of moving to new house, and construction year of the residence also were included.
If there were missing or outlier values in informed consent or crucial items such as age ( ≤ 5 or ≥ 15 yr), gender, height, weight, and answers for symptom questions, those questionnaires were excluded from the analysis. The final number of students included in the analysis was 25,322 (10,555 boys and 14,767 girls). Survey weights for respondents were constructed beginning with reciprocals of inclusion probabilities for differential probabilities of selection and non-response.
BMI was calculated by self-reported height and weight, and classified into four groups ( ≤ 25 percentile, 26-50 percentile, 51-75 percentile, and > 75 percentile) based on BMI-for-age percentiles of Korean growth charts that were developed based on data from national growth surveys for children and adolescents (27,403 boys and 25,657 girls) in 1998 and 2005 (11). In this study, we evaluated the association between demographic or environmental characteristics and wheeze using a two-stage hierarchical model because of the possibility of a contextual effect of residential area on the risk of wheeze. In the first stage, univariate or multiple logistic regression analysis was conducted to investigate any independent association between potential confounders and wheeze in each residential area. In the second stage, to combine residential area-specific estimates, multilevel logistic regression analysis using the GLIMMIX procedure (SAS version 9.2, SAS Institute Inc, Cary, NC, USA) was used; the usual two-level random-intercept model, with factors associated with demographics or living environment as level-1 units and with residential areas as level-2 units were used. All analyses were conducted separately by gender.
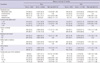
Among 25,322 students, 4.9% (6.0% in boys and 4.1% in girls) reported having wheeze symptoms in the last 12 months. In univariate logistic regression analysis, demographic characteristics such as age, birth weight, BMI, prematurity, and physician-diagnosed disease were significantly associated with the prevalence of wheeze among boys (Table 1). In girls, all variables with the exception of age and birth weight were significantly associated with the prevalence of wheeze. In both boys and girls, the lowest BMI ( ≤ 25 percentile) was negatively associated with the prevalence of wheeze compared with the 26-50 percentile, and the 51-75 percentile. Conversely, the highest BMI ( > 75 percentile) was positively associated with the prevalence of wheeze.
Table 2 shows the association between living environments and the prevalence of wheeze. Factors such as ETS exposure, history of moving to new house, presence of visible mold and moisture, pets at home, and construction year of the residence (10-19 or ≥ 20 vs 3-4 yr) were positively associated with the prevalence of wheeze in both boys and girls. The prevalence of wheeze was significantly higher in industrial area compared with provincial area among girls but not among boys. The prevalence of wheeze was significantly lower in rural area compared with provincial area among boys.
In multivariate logistic regression analysis after stratification of the respondents by residential areas (Table 3), birth weight was negatively associated with the prevalence of wheeze across all residential areas among boys. In metropolitan area, the lowest BMI ( ≤ 25 percentile) was negatively associated with the prevalence of wheeze compared with the 26-50 percentile, and the 51-75 percentile and the highest BMI ( > 75 percentile) was positively associated. Another area has partially significant association between the prevalence of wheeze and BMI.
In girls, the prevalence of wheeze was negatively associated with lowest BMI in all residential areas (Table 4). However, the association between the prevalence of wheeze and highest BMI was positively in all residential areas.
For boys, the prevalence of wheeze among boys was positively associated with pets at home and visible mold or moisture in multivariate logistic regression analysis (Table 3). The association between the prevalence of wheeze and age, ETS exposure, moving to new house, and electricity bill was different among residential areas. In multilevel logistic regression analysis, ETS exposure, pets at home, visible mold or moisture, and moving to new house were positively associated with the prevalence of wheeze among boys.
In girls, the association between the prevalence of wheeze and pets at home, and presence of visible mold and moisture was positively in all residential areas (Table 4). The association between potential confounding factors such as ETS exposure, moving to new house, construction year of the residence, and electricity bill and the prevalence of wheeze was not consistent across residential areas. In multilevel logistic regression analysis, the prevalence of wheeze was positively associated with ETS exposure, pets at home, visible mold or moisture, and construction year of the residence, whereas, age, birth weight, and middle electricity bill were negatively associated with the prevalence of wheeze.
In the present study, we used a two-stage hierarchical model to control contextual effect of residential areas, and observed a significant association between the prevalence of wheeze and BMI and living environmental factors such as ETS exposure, pets at home, and presence of visible mold or moisture among elementary school children. The association was evident in the highest BMI percentile group, and stronger in girls. In the ROK, two cross-sectional studies were conducted to investigate the prevalence of asthma and other allergic diseases in 1995 and 2000. Although limitations on the data analysis exist, they also showed the association between increased prevalence of wheeze and BMI in the 2000 but not in the 1995 survey (1). These results suggest that BMI has become a triggering factor for asthma symptoms in Korean children, which is consistent with previous studies conducted in western countries (12, 13). Many studies have proposed the potential underlying mechanisms for the relationship between obesity and asthma symptoms; systemic inflammation (14, 15), airway hyper-responsiveness (16), common genetic pathways (17), changes in diet and physical activity, and mechanical factors: gastro-esophageal reflux, obstructive sleep apnea, and reduced lung volumes. However, some studies failed to show an association, while others showed as association in one gender (18, 19). Due to issues in the measurement of obesity in children and many potential confounding factors such as environment, allergens, and genotypes, large prospective birth cohort studies will be required to identify temporal relationships between obesity and asthma or asthma symptoms and plausible mechanisms to explain this relationship. The lowest BMI and birth weight were associated with the decreased prevalence of wheeze in the present study. Although results regarding birth weight are still contradictory (20), epidemiologic studies consistently have suggested a positive relationship between these factors and development of asthma among children (21).
We classified in quartiles of BMI-for-age percentiles of Korean growth charts. Similar results were obtained when BMI were classified into underweight ( < 5th percentile), normal ( ≥ 5th and < 85th percentile), overweight ( ≥ 85th and < 95th percentile), obese ( ≥ 95th percentile). In multilevel logistic regression analysis, odds ratio (OR) underweight, overweight and obese on prevalence of wheeze among boys were 0.93 (95% confidence interval [CI], 0.82-1.06), 1.43 (95% CI, 1.32-1.54) and 1.46 (95% CI, 1.30-1.63), respectively. Among girls, higher BMI was also significantly associated with higher prevalence of wheeze; OR of underweight, 0.89 (95% CI, 0.79-0.99); OR of overweight, 1.40 (95% CI, 1.29-1.53); OR of obese, 1.86 (95% CI, 1.65-2.10).
In the present study, poor living environments such as ETS exposure, pets at home, presence of visible mold or moisture, history of moving to new house, and construction year of the residence ( ≥ 20 vs 3-4 yr) were associated with an increase in the prevalence of wheeze among both boys and girls in multilevel logistic regression analysis. ETS and mold are known to be strong allergens and the possibility of the presence of mold, moisture and other allergens such as endotoxin, house dust mites, and microorganisms is high in older houses. Therefore, these factors might play a role in an increase in the prevalence of wheeze, particularly among children. Moving to new house and residing in a newly constructed house, especially at an early age, may also increase the risk of developing asthma or asthma symptoms due to exposure to new allergens such as volatile organic compounds, particulate matter, sulfur dioxide, and nitrogen species (22). However, across residential areas, these associations were not consistent with the exception of pets at home and presence of visible mold or moisture.
Compared with other residential areas, moving to new house was negatively associated with the prevalence of asthma symptoms in rural area; in provincial area, construction year of the residence (old vs new house) also were negatively associated with the prevalence of wheeze among boys and ETS exposure was negatively associated among girls; in industrial area, construction year of the residence (old vs new house) also were negatively associated with the prevalence of wheeze among girls only. Although the possibility of a reverse association might exist due to the cross-sectional nature of our study, we think that risk factors associated with residential areas such as sedentary life style, exposure to microbes, food intake, car transportation, and exposure to indoor or outdoor air pollution also might affect study results because early-life exposures may interact with genotype and response to environmental factors (23). Previous studies have shown the protective effect of exposure to livestock or poultry, stables, allergens, and endotoxin in rural areas against the development of asthma and allergies, which was different from those observed in urban areas (24).
Contrary to the results in boys, the prevalence of wheeze among girls was positively associated with construction year of the residence ( ≤ 2 vs 3-4 yr) as determined by multilevel logistic regression analysis. Across residential areas, the association between potential confounding factors and the prevalence of wheeze was not consistent with the exception of highest BMI, pets at home and presence of visible mold or moisture, and differed from those observed among boys. It was difficult to interpret these findings because of study limitations. However, one possible explanation is that because the prevalence of asthma or asthma symptoms in childhood is more common in boys with a switch to increased prevalence in girls by adolescence (25), the association between risk factors and asthma symptoms among girls might not have been appropriately explored. Gender differences on these issues are not fully understood, and further investigations are still needed.
This study has some important limitations. First, BMI was calculated based on reported height and weight. We cannot exclude the possibility of measurement error. Since elementary students measure anthropometry once a year at school, they know relatively accurate their height and weight. Although previous studies have suggested that BMI calculated from self-reported height and weight may be a valid indicator of obesity (26), self-reported data may underestimate the true prevalence of obesity and vice versa. Because self-reported heights are higher than measured heights and self-reported weights are smaller (27), the misclassification of BMI is non-differential. Thus, our results are biased toward the null and underestimate the true effect. Second, the prevalence of asthma symptoms might not be accurately estimated. In this study, we used the Korean version of the ISAAC WQ to investigate the prevalence of asthma symptoms. However, results from the ISAAC study showed that both WQ and a video questionnaire (AVQ) should be used in order to better define asthma in a population survey, regardless of translation or interpretation problems (28). A previous cross-sectional study conducted in Korea also showed that the prevalence of asthma symptoms was generally high using the WQ compared to AVQ (1). Although like other epidemiologic studies, ISAAC WQ was used in this study. Thus, the prevalence of asthma symptoms might be overestimated. Third, non-response bias might have occurred due to a relatively low response rate. In this study, the overall response rate was 61.8%, which was the marginal response rate recommended by the ISAAC protocol (over 60%-70% in children). However, among respondents, only 81.6% were included in the analysis due to outlier or missing values in major independent variables such as age, gender, height, and weight. Although we used a weighting adjustment to compensate for survey non-response, weighting adjustment for non-response cannot compensate for bias that is attributable to differences in the underlying population means or frequencies for respondents and non-respondents. To acquire an unbiased estimate of risk ratio, further investigations considering an increase in response rate and acquisition of the information on the characteristics of non-respondents are needed. Finally, we used self-reported questionnaire data. A recent study showed that BMI does not represent the fat distribution in children (29). Although it is an indirect measurement of body fat, it is thought to be a valid proxy for fat mass in children because of its strong association with total body fat. BMI is easily calculated and convenient to use in large-scale epidemiological studies (30). Moreover, we estimated the environmental factors by questionnaire in the current study. Therefore, further studies involving more detailed data on the clinical characteristics of asthma and potential confounding factors such as socioeconomic status, residential areas, and indoor or outdoor environment also must be considered.
In conclusion, we observed that BMI has become an important factor for asthma or asthma symptoms among children in the ROK, and the associations between living environments and asthma symptoms were different between gender and among residential areas. Despite several limitations, our results suggest that a prevention strategy and implementation plan to reduce asthma or asthma symptoms should be considered according to differences between types of residential areas.
Figures and Tables
Table 1
Demographic characteristics of study participants and association with wheeze in the last 12 months by gender

Table 2
Environmental characteristics of study participants and association with wheeze in the last 12 months by gender
ACKNOWLEDGMENTS
We thank the Korean Academy of Pediatric Allergy and Respiratory Disease for providing the Korean version of ISAAC written questionnaire; and all the children and parents who participated.
AUTHOR SUMMARY
Association Between Body Mass Index and Asthma Symptoms Among Korean Children: A Nation-Wide Study
Mina Suh, Ho-Hyun Kim, Dong Phil Choi, Kyung Won Kim, Myung Hyun Sohn, Kyoung Hwa Ha, Won Ju Hwang, Changsoo Kim, Kyu-Earn Kim and Dong Chun Shin
The prevalence of asthma and obesity is increasing worldwidely, and their association has been suggested. We observed significantly association between highest BMI quartile and prevalence of wheeze in all residential areas using nation-wide cross-sectional data in Korea. Some living environment factors (ETS exposure, pets at home, visible mold or moisture, moving to new house, and construction year of the residence) were significantly associated with the prevalence of wheeze.
References
1. Hong SJ, Lee MS, Sohn MH, Shim JY, Han YS, Park KS, Ahn YM, Son BK, Lee HB. Korean ISAAC Study Group. Self-reported prevalence and risk factors of asthma among Korean adolescents: 5-year follow-up study, 1995-2000. Clin Exp Allergy. 2004. 34:1556–1562.
2. Kim HM, Park J, Kim HS, Kim DH, Park SH. Obesity and cardiovascular risk factors in Korean children and adolescents aged 10-18 years from the Korean National Health and Nutrition Examination Survey, 1998 and 2001. Am J Epidemiol. 2006. 164:787–793.
3. Suh M, Kim HH, Sohn MH, Kim KE, Kim C, Shin DC. Prevalence of allergic diseases among Korean school-age children: a nationwide cross-sectional questionnaire study. J Korean Med Sci. 2011. 26:332–338.
4. von Mutius E, Schwartz J, Neas LM, Dockery D, Weiss ST. Relation of body mass index to asthma and atopy in children: the National Health and Nutrition Examination Study III. Thorax. 2001. 56:835–838.
5. Scholtens S, Wijga AH, Seidell JC, Brunekreef B, de Jongste JC, Gehring U, Postma DS, Kerkhof M, Smit HA. Overweight and changes in weight status during childhood in relation to asthma symptoms at 8 years of age. J Allergy Clin Immunol. 2009. 123:1312–1318.
6. Hjellvik V, Tverdal A, Furu K. Body mass index as predictor for asthma: a cohort study of 118,723 males and females. Eur Respir J. 2010. 35:1235–1242.
7. Lee SI, Shin MH, Lee HB, Lee JS, Son BK, Koh YY, Kim KE, Ahn YO. Prevalences of symptoms of asthma and other allergic diseases in Korean children: a nationwide questionnaire survey. J Korean Med Sci. 2001. 16:155–164.
8. Hong SJ, Lee MS, Lee SY, Ahn KM, Oh JW, Kim KE, Lee JS, Lee HB. for the Korean ISAAC Study Group. High body mass index and dietary pattern are associated with childhood asthma. Pediatr Pulmonol. 2006. 41:1118–1124.
9. Nordling E, Berglind N, Melén E, Emenius G, Hallberg J, Nyberg F, Pershagen G, Svartengren M, Wickman M, Bellander T. Traffic-related air pollution and childhood respiratory symptoms, function and allergies. Epidemiology. 2008. 19:401–408.
10. Basagaña X, Sunyer J, Kogevinas M, Zock JP, Duran-Tauleria E, Jarvis D, Burney P, Anto JM. Socioeconomic status and asthma prevalence in young adults: the European Community Respiratory Health Survey. Am J Epidemiol. 2004. 160:178–188.
11. Lee SY, Kim YN, Kang YJ, Jang MJ, Kim J, Moon JS, Lee CG, Oh K, Kim YT, Nam CM. The methodology for developing the 2007 Korean growth charts and blood pressure nomogram in Korean children and adolescents. Korean J Pediatr. 2008. 51:26–32.
12. Tai A, Volkmer R, Burton A. Association between asthma symptoms and obesity in preschool (4-5 year old) children. J Asthma. 2009. 46:362–365.
13. Ginde AA, Santillan AA, Clark S, Camargo CA Jr. Body mass index and acute asthma severity among children presenting to the emergency department. Pediatr Allergy Immunol. 2010. 21:480–488.
14. Huang F, del-Río-Navarro BE, Monge JJ, Torres Alcántara S, Ontiveros JA, Olivos EN, Martinez de Castro NG, Zhao L, Hong E. Endothelial activation and systemic inflammation in obese asthmatic children. Allergy Asthma Proc. 2008. 29:453–460.
15. Kim KW, Shin YH, Lee KE, Kim ES, Sohn MH, Kim KE. Relationship between adipokines and manifestations of childhood asthma. Pediatr Allergy Immunol. 2008. 19:535–540.
16. Jang AS, Lee JH, Park SW, Shin MY, Kim DJ, Park CS. Severe airway hyperresponsiveness in school-aged boys with a high body mass index. Korean J Intern Med. 2006. 21:10–14.
17. Thomsen SF, Ulrik CS, Kyvik KO, Sørensen TI, Posthuma D, Skadhauge LR, Steffensen I, Backer V. Association between obesity and asthma in a twin cohort. Allergy. 2007. 62:1199–1204.
18. Hancox RJ, Milne BJ, Poulton R, Taylor DR, Greene JM, McLachlan CR, Cowan JO, Flannery EM, Herbison GP, Sears MR. Sex differences in the relation between body mass index and asthma and atopy in a birth cohort. Am J Respir Crit Care Med. 2005. 171:440–445.
19. Beckett WS, Jacobs DR Jr, Yu X, Iribarren C, Williams OD. Asthma is associated with weight gain in females but not males, independent of physical activity. Am J Respir Crit Care Med. 2001. 164:2045–2050.
20. Villamor E, Iliadou A, Cnattingius S. Is the association between low birth weight and asthma independent of genetic and shared environmental factors? Am J Epidemiol. 2009. 169:1337–1343.
21. Metsälä J, Kilkkinen A, Kaila M, Tapanainen H, Klaukka T, Gissler M, Virtanen SM. Perinatal factors and the risk of asthma in childhood: a population-based register study in Finland. Am J Epidemiol. 2008. 168:170–178.
22. Kim H, Bernstein JA. Air pollution and allergic disease. Curr Allergy Asthma Rep. 2009. 9:128–133.
23. Wong GW, Chow CM. Childhood asthma epidemiology: insights from comparative studies of rural and urban populations. Pediatr Pulmonol. 2008. 43:107–116.
24. Adler A, Tager I, Quintero DR. Decreased prevalence of asthma among farm-reared children compared with those who are rural but not farm-reared. J Allergy Clin Immunol. 2005. 115:67–73.
25. Tantisira KG, Colvin R, Tonascia J, Strunk RC, Weiss ST, Fuhlbrigge AL. Childhood Asthma Management Program Research Group. Airway responsiveness in mild to moderate childhood asthma: sex influences on the natural history. Am J Respir Crit Care Med. 2008. 178:325–331.
26. Banach A, Wade TJ, Cairney J, Hay JA, Faught BE, O'Leary DD. Comparison of anthropometry and parent-reported height and weight among nine year olds. Can J Public Health. 2007. 98:251–253.
27. Krul AJ, Daanen HA, Choi H. Self-reported and measured weight, height and body mass index (BMI) in Italy, the Netherlands and North America. Eur J Public Health. 2011. 21:414–419.
28. Crane J, Mallol J, Beasley R, Stewart A, Asher MI. International Study of Asthma and Allergies in Childhood Phase I Study Group. Agreement between written and video questions for comparing asthma symptoms in ISAAC. Eur Respir J. 2003. 21:455–461.
29. Musaad SM, Patterson T, Ericksen M, Lindsey M, Dietrich K, Succop P, Khurana Hershey GK. Comparison of anthropometric measures of obesity in childhood allergic asthma: central obesity is most relevant. J Allergy Clin Immunol. 2009. 123:1321–1327.
30. Lindsay RS, Hanson RL, Roumain J, Ravussin E, Knowler WC, Tataranni PA. Body mass index as a measure of adiposity in children and adolescents: relationship to adiposity by dual energy x-ray absorptiometry and to cardiovascular risk factors. J Clin Endocrinol Metab. 2001. 86:4061–4067.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download