Abstract
This study was performed to describe the patterns of healthcare switching with overlapping use of anti-diabetic medication in the elderly using the Korea Health Insurance Review and Assessment Service's claims data. The study subjects were ambulatory elderly diabetic patients (ICD-10, E10-14) receiving at least one oral anti-diabetic drug or insulin, and visiting healthcare facilities more than two times between January and December 2005. A total of 457,975 elderly diabetic ambulatory care patients were identified. The mean of visiting frequencies was 9.0 ( ± 3.6) and switching frequencies was 1.5 ( ± 0.8) during 2005. Switching group consisted of 33% of total study subject. Healthcare switching was common in female patients who were older, and had treated polytherapy more in rural areas. The movement among primary care medical services was very common among the patients in the switching group (52.6%). A statistically significant correlation was observed between the healthcare switching and concomitant drug use (rho = 0.96), and overlapping days (rho = 0.57). The use of overlapping anti-diabetic medication increased with the extent of healthcare switching. Further, frequent switching of healthcare between primary clinics was observed. Efforts should be made to establish continuity for the elderly diabetic patients with the identification of frequent switching with overlapping medication.
Korea is a rapidly aging society with persons over the age of 65 accounting for 10.7% of the total population during mid 2010; population projections predict 14.3% by 2018 and 20.8% by 2026 (1). Diabetes in the elderly has been reported as a growing problem; a larger proportion of newly diagnosed diabetics are older (2). Elderly diabetic patients need continuous monitoring for tight glycemic control and treatment with anti-diabetic drugs, for the prevention of diabetes related complications (3).
Healthcare switching is referred to as the switching healthcare facilities without a professional referral in the same illness. It may contribute to the increased risk of overlapping medication among elderly patients (4, 5). With a culture that prefers taking medicines and health supplements, in Asian countries, such behaviour had been a problem reported in several countries and is considered a serious public health concern (6, 7). In addition, patients do not need to register with a primary care physician, and they can visit any healthcare provider in Korea (8). Under the current health care delivery system, all of primary, secondary, tertiary hospital can provide ambulatory care. Under such circumstances, overlapping drug use associated with healthcare switching can result in serious health problems including polypharmacy, higher cost, overlapping medication and adverse outcome such as acute hypoglycemia (9, 10); prescriptions might be duplicated without the knowledge of all healthcare providers (11). This can lead to drug-drug interactions and drug-disease interactions that can cause adverse drug events (12).
However, limited information on the patterns of healthcare switching is known in the elderly diabetic patients. There has been no published epidemiologic study on overlapping drug use associated with switching healthcare institutions in a population-based setting. Therefore, this study was performed to describe the patterns of healthcare utilization over one year and the association between the frequency of healthcare switching and overlapping use of anti-diabetic medication among the elderly diabetic patients.
The Korean Health Insurance Review and Assessment Service (HIRA) database was used for this study. The National Health Insurance (NHI) program was initiated in Korea in 1977 and achieved universal coverage of the population by 1989 (13). All Koreans are covered by the National Health Insurance System. Accordingly, the HIRA database contains all information on healthcare utilization and prescribed medications for approximately 50 million Koreans.
The claims data for elderly patients (aged 65 yr or older) that had been submitted by healthcare providers in 2005 were obtained. The HIRA offered the claims data with the individual identity of patients concealed. The database included an unidentifiable code representing each individual together with age, gender, diagnosis, and ambulatory care utilization at clinics and/or hospitals, dates of visits, types of medical care facilities, region and specialty. In addition, prescribed drug information included the brand name, generic name, prescription date, duration and route of administration. The diagnosis was coded according to the International Classification of Disease, Tenth Revision (ICD-10). The database contained information regarding 4,159,305 elderly patients and 100,838,744 prescriptions.
We performed the population-based cross-sectional study. The study subjects were elderly diabetic patients older than 65 yr of age that presented to clinics and/or hospitals for ambulatory care from January 1, to December 31, 2005. A diabetic patient was defined as a patient with a diagnosis consistent with ICD-10 (E10-E14) and who had received prescriptions of insulin and/or oral anti-diabetic drugs (OAD). The OAD were selected on the treatment guideline for diabetes (14, 15): sulfonylureas, metformin, meglitinides, thiazolidinedion, and alpha glucosidase inhibitors. Patients that presented to clinics and/or hospitals only one time in 2005 were excluded.
The healthcare utilization patterns of the ambulatory care visits are described as the visiting frequency (VF) and the switching frequency (SF) during the study period. The 'VF' was the total number of visit for the patient during 2005. The 'SF' was the number of times that the patient changed institutions; that is, how frequently the patient changed healthcare facilities during one year. The VF and SF referred to all ambulatory care visits for the oral anti-diabetic drugs. Healthcare utilization patterns are displayed in a cross-table that matches the VF and SF.
The study population was divided into two groups: the non-switching group and switching group. The non-switching group included patients who visited one healthcare facility regardless of the VF. The switching group included patients who changed medical institutions more than one time during the study period. Each group was compared including the patient characteristics (age and gender) and healthcare provider's characteristics (location and type of medical service: primary clinics, secondary hospital, and tertiary hospital). In addition, the frequency and proportion of the patients that had insulin therapy and/or OAD therapy, that is, mono- or polytherapy was calculated for each group.
The institutional visiting patterns were determined by describing the movements from primary (P) to other primary clinics, or from primary to secondary (S) or tertiary facilities (T). According to the SF, the frequency of switching patterns for anti-diabetic medications in 2005 was determined. 'P1→P2' meant sequential movement from one primary clinic to another. 'P1→S1→P2' meant that an elderly diabetic patient visited one primary clinic, moved to a secondary healthcare facility first, and then to other primary clinics during 2005.
Overlapping anti-diabetic medication was assessed as follows: total prescription days (TPD), total prescription days longer than 365 days (TPD365), concomitant drug use (CDU), and overlapping days (OD). The 'TPD' was defined as the total number of days of anti-diabetic prescriptions during 2005. The TPD was estimated using the "prescription duration" from the HIRA database. The days for the diabetic prescription were added from the healthcare provider (one or more). The TPD365 was defined as the patient who was prescribed anti-diabetic medication longer than 365 days.
The 'CDU' was defined as a prescription from a different healthcare provider overlapping in duration the anti-diabetic medication (16). To assess the CDU, subjects were identified according to whether they had been prescribed a diabetic drug simultaneously from different healthcare providers. When the dates of the prescriptions overlapped, from different healthcare providers, it was considered a CDU. The starting date was recorded when the healthcare provider issued the prescription for the first course of anti-diabetic therapy. The end date of one anti-diabetic therapy course was calculated using the information on the prescription date and duration.
The 'OD' was defined as the number of days that anti-diabetic drugs were duplicated from different healthcare providers. The OD was calculated by adding the days duplicated from the study subjects that had CDUs. According to the SF, mean number of TPD, the proportion of TPD356, the proportion of CDU, mean number of OD was calculated.
Descriptive data including frequencies, proportions, means (SD), median, and range (min, max) are presented. The Cochran-Armitage test was used to identify statistically significant trends in age, region, type of medical service and drug therapy. To compare the gender proportions, the chi-square test was used. Associations between both healthcare switching and non-switching group and demographic factors and other indicators were quantified by adjusted odds ratios (ORs) and corresponding 95% confidence intervals (CIs) using the multivariate logistic regression.
Spearman's rank test was used for the SF to determine the correlation with the each drug assessment indicator: TPD, TPD365, CDU, and OD. The significance level was set at P < 0.05 and all tests were two tailed. All data were analyzed using SAS 9.1 (SAS Institute Inc, Cary, NC, USA).
A total of 457,975 elderly diabetic ambulatory care patients were identified from the HIRA database that had visited healthcare facilities and were coded with ICD-10 (E10-E14), and received more than one course of prescribed anti-diabetic medication. Their mean age (standard deviation [SD]) was 71.5 yr (± 5.3) and 61.6% were female.
The median number of VF among Korean elderly diabetic patients was 10 with a mean of 9.0 (± 3.6) during 2005 (range 2-62). The median number of SF was one with a mean of 1.5 (± 0.8) during 2005 (range 1-17) (Fig. 1A). Fig. 1B shows the distribution of individuals receiving anti-diabetic prescriptions by the number of SF and VF. Most individuals (91.4%) used either one or two healthcare providers; 6.3% of individuals used two, 1.7% of individuals visited three different healthcare providers, and less than 1% used more than five providers. Overall, 191 (0.05%) individuals used six or more healthcare providers.
Among all Korean elderly diabetic patients who were prescribed more than one anti-diabetic medication, the healthcare switching group included 151,143 (33%), and the non-switching group 306,832 (67%). The switching group consistently decreased among each successive age group (chi-square for trend, P < 0.001). Comparison of the group aged 65 yr through 69, showed that an older age group was associated with healthcare switching (31.1% vs 30.0%; 18.3% vs 16.7%; 7.7% vs 6.9%; 2.1% vs 2.0%). In addition, female patients were significantly more likely to switching healthcare institutions than male patients (65.5% vs 59.7%; ORadj, 1.26; 95% CI, 1.24-1.27) (Table 1).
Of all prescriptions among the elderly diabetic patients, the visits in rural areas were associated with healthcare switching (23.1% vs 15.6%; ORadj, 1.43; 95% CI, 1.41-1.45). Relative to other types of medical service, visits to the primary medical clinic were associated with a significantly increased ratio of healthcare switching (69.6% vs 68.9%; ORadj, 1.90; 95% CI, 1.85-1.94). Anti-diabetic drug therapy was categorized as OAD mono, poly or any insulin therapy; the proportion of patients that had any insulin therapy was high in the switching group (7.7% vs 5.2%; ORadj, 1.65; 95% CI, 1.63-1.72). Small medical service units, rural healthcare, an older age group, and the severity of diabetes were all associated with increased odds of healthcare switching in a linear trend (χ2 for trend, P < 0.001) (Table 1).
The 'P1→P2' type was the most common healthcare switching pattern among patients who changed one time (55.2%); 'P1→P2→P3' was the most common pattern among patients who changed two times (47.1%); ''P1→P2→P3→P4' among patients that changed three times (42.1%), and 'P1→P2→P3→P4→P5' among patients that changed more than four times (38.8%). Almost half of the patients moved among primary medical services in the switching group during 2005 (52.6%).
The 'P1→T1' type was the second most frequent pattern consisting of 15.8% of patients who changed once; 'P1→P2→T1' of patients who changed twice (10.7%); 'P1→P2→P3→T1' of patients who changed three times (7.7%), and 'P1→P2→P3→P4→T1' of patients who changed more than four times (4.8%). Healthcare switching among primary medical services and final movement to a tertiary healthcare facility was commonly observed and was the second most common pattern (Table 2).
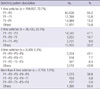
Fig. 2 shows the statistically significant correlation between the number of SF, and drug use assessment indicators: TPD, TPD365, CDU, and OD (Spearman's rho = 0.99, P < 0.001; 0.92, P < 0.001; 0.96, P < 0.001; 0.57, P = 0.04).
The mean number of TPD among elderly diabetic patients during 2005 increased rapidly from 264.9 days in the non-switching group to 275.4 days in three time switchers and 331.2 days in eight time switchers. The proportion of TPD365 was 7.4% among non-switching group, 11.1% for the one time switcher, 15.7% for the four time switcher, 22.9% for the seven time switcher; it increased rapidly according to the SF.
The proportion of patients who had a CDU was 47% for the one time switchers, 69.6% for the two time switchers, 83.2 % for the three time switchers, and 90.5% for the four time switchers; it also increased dramatically according to an increase in the SF. Similarly, the OD was 6.2 days for one time switchers, 8.4 for two time switchers, 10.3 for six time switchers (Fig. 2).
This study showed that the healthcare switching was not a common problem among elderly diabetic patients during one year. However, compared to the non-switching group, the switching group was more likely to be prescribed anti-diabetic drugs concomitantly. In addition, switching among primary medical institutions was very common; considering the very low proportion of referral (17), this suggests that clinician referrals may be infrequent, self referral among patients is common reflecting inefficient healthcare delivery system in Korea.
In addition, the findings of this study showed that switching behavior occurred more frequently in female patients, older patients, rural areas, and included more severe diabetic patients. These findings are consistent with previous studies that reported that the extent of healthcare switching was related to multiple healthcare providers, low continuity of care, and was more common in older female patients (18). Gender differences are well known with regard to healthcare behavior as consistently shown by numerous reports from previous research (5, 12, 19). However, the findings of frequent switching behavior in severe diabetic patients, in rural areas had not been previously reported. Severe diabetic patients were particularly vulnerable to adverse events such as hypoglycemia or failure to maintain blood sugar levels. Therefore, the results suggest that prevention of inappropriate behavior in such populations is needed. It also suggests where to target the frail population for the prevention of frequent healthcare switching and its associated risks.
Healthcare switching is a universal and dynamic process where each patient seeks a doctor for the optimum service and treatment. Further, it reflects a patient's various concerns with regard to individual healthcare utilization (20). Additionally, diabetes care is complex as it involves both patient self-care and the administering of care by the provider (21). Healthcare switching in diabetic patients raises questions about the quality of the doctor-patient relationship. This may represent the absence of a stable relationship between patients and doctors, or dissatisfaction with the heathcare as well as a result of a poor healthcare delivery system (22). Previous research reports that diabetic patients in early stages tend to move institutions in order to find their own doctor (23). However, our study results indicated that severe diabetic patients with a prescription of polytherapy tended to switch healthcare providers frequently. In terms of doctor-patient relationships, they moved institutions for better service related to cost, kindness, patient participation, communication, or different therapeutic regimens (24, 25). There is also a possibility that patients deliberately switch healthcare providers in order to obtain services they would not receive otherwise, such as overlapping or unnecessary medications (22). Such behavior has led to duplication of services, higher costs, and a risk of adverse outcome such as acute hypoglycemia (12, 26, 27).
Of particular note, we observed one patient who had switched healthcare providers 17 times, and another 80% of patients who had switched more than three times all exhibited overlapping medication. From the perspective of patient safety and cost-containment, efforts should be made to study how continuity of care could be established to better address the needs of these patients. However, up to now, there has been little information about the reasons some patients switch healthcare providers due to overlapping medication. Based on the data, not much can be done to help them. Ultimately, changes in the behavior of diabetic patients are needed to improve health care delivery through the introduction of a registered family physician system (21).
Our study focused on describing their patterns including sequential changes and drug prescription patterns among institutions. With regard to drug use, the results showed that SF was highly correlated with the following drug exposure indicators: TPD, TPD365, CDU, and OD. Four drug exposures showed the increase according to the increase of extent of healthcare switching. The correlation coefficient might be near linear, and statistically significant. This result shows that a substantial number of anti-diabetic drugs were prescribed without mutual recognition among the treating institutions; such patients could be exposed to significant risks and adverse events, and the society subject to wasted medical resources.
In this study, healthcare visits were described as the distribution of individuals by SF and VF. According to the SF, the overlapping of anti-diabetic medication could be described. The CDU was defined as overlapping of prescribing by different healthcare providers during the course of the medication; this provided an assessment of the differences in anti-diabetic drugs prescribed among institutions. Previous research used measures such as 'the number of drugs prescribed' and 'the number of days of medication' based on the aggregate of the unit of service (12, 18, 22). In this study, the 'CDU' was used to represent both multiple providers and anti-diabetic drugs simultaneously.
In this study, prevalent cases were included; that is chronic and newly diagnosed, severe and mild patients. This had the advantage of reflecting real clinical practice. However, confounding might be generated by the difference in the initial state when performing further study to evaluate the outcome. An approach to identify incident cases should be adopted in future research. For policy decisions, both descriptive and in-depth investigation should be performed together.
This study had several strengths. First, this study included a large population representing diabetic patients nationwide in Korea. An entire targeted population was studied rather than a sampled one using the claims database for ambulatory visits collected by the NHI program in Korea, which covers nearly all inhabitants of Korea. Second, a large national claims database was used to investigate the patient's health related behavior. This database includes comprehensive information on more than 50 million patients in Korea, and provides information on both the patient visit patterns and providers' prescribing information. Third, it is the first nationwide epidemiological study regarding healthcare utilization among elderly diabetic patients to date. Both the healthcare visit pattern and it associated drug use were comprehensively investigated. The findings provided descriptive information about elderly diabetic patients' healthcare switching and its associated overlapping use for anti-diabetic medication. Fourth, this study adopted the latest assessment methods for drug exposure to determine the extent of overlapping drug associated with healthcare switching. The results showed inappropriate drug use with overlapping prescriptions and suggests the risk of adverse outcome associated with healthcare switching behaviour (12, 26, 27).
The limitations of this study include the following. First, referrals could not be identified because the HIRA database did not include this information. Therefore, clinician referral and self-referral may have been mixed in the switching group. However, previous research has reported a very low proportion of referrals: the proportion of referral cases was only 0.7% of the total office visits in a Cheonan practice-based research network study composed of 10 clinics (17). Additionally, a few studies have reported that there has been no change in healthcare utilization patterns after referral requirement were instituted for insurance patients on July 1, 1989 (28). Therefore, our research showed the sequential changing pattern between institutions, which has provided useful information about healthcare switching. However, to obtain more accurate results, information on referrals should be included in the database. Second, diabetic patients were defined according to the diagnosis reported to the HIRA, which might differ from the patients' actual diagnosis. A validation study compared the diagnosis derived from the HIRA database with the actual diagnosis in the patient medical records (29). The positive predictive value (PPV) was calculated according to the disease group. The PPV was 72.3% for diabetes mellitus in the cases identified by ambulatory prescriptions.
An online decision support system is planned to help prevent overlapping drug use and concurrent drug utilization review between institutions are in the process of being implemented in since December, 2010 (30). It will help avert contraindicated drug-drug interaction or overlapping drug use with the detection of healthcare switching behavior such as doctor-shopping. From the long-term perspective, an integrated healthcare delivery system, and an effective data exchange might be the solution for switching behaviour and the prevention for overlapping medication.
Figures and Tables
 | Fig. 1The distribution of individuals by the number of visiting frequency (VF), and switching frequency (SF) per year (A) The number of patients in 2005 was plotted as a function of the number of VF and SF. (B) Distribution crosstable. Data are the VF and SF in 2005. (1A): Visiting frequency (VF) among Korean elderly diabetic patients. Total N=457,975, median=10; mean = 9.0; starndard deviation = 3.6; range: 2-62. (2A): The switching frequency (SF) among Korean elderly diabetic patients. Total N = 457,975, median = 1; mean = 1.5; starndard deviation = 0.8; range: 0-17. |
 | Fig. 2Trends in antidiabetic medication according to the number of switching frequency (SF) among elderly diabetic patients during 2005. (A) Y1 = Mean number of total prescription days (TPD), Y2 = The proportion of the patients who had TPD longer than 365days (TPD365) (B) Y1 = The proportion of the patients that had concomitant drug use (CDU), that is, those with prescriptions from different who healthcare providers during the same period overlapping more than two days, Y2 = The extent of the overlapping days (OD), all were plotted as a function of the number of SF; Spearman's rho (TPD) = 0.99, P < 0.001; Spearman's rho (TPD365) = 0.92, P < 0.001; Spearman's rho (CDU) = 0.96, P < 0.001; Spearman's rho (OD) = 0.57, P = 0.05. |
Table 1
The characteristics of elderly diabetic patients in the healthcare switching group and non-switching group

*P value for trend was calculated by using Cochran-Armitage test; †P value was calculated by using chi-square test; ‡Urban area included metropolitan cities and cities in the province that had a population of over 500,000; §Rural area included the towns that had a population of under 50,000. OAD, Oral Antidiabetic Drugs.
AUTHOR SUMMARY
Overlapping Medication Associated with Healthcare Switching among Korean Elderly Diabetic Patients
Ju-Young Shin, Nam-Kyong Choi, Sun-Young Jung, Ye-Jee Kim, Jong-Mi Seong and Byung-Joo Park
This study was performed to describe the patterns of healthcare switching with overlapping use of anti-diabetic medication in the elderly using the Korea Health Insurance Review and Assessment Service's claims data. Healthcare switching was common in female patients that were older, and had treated polytherapy more in rural areas. A significant correlation was observed between healthcare switching and concomitant drug use, and overlapping days. Efforts should be made to establish continuity for the elderly diabetic patients with the identification of frequent switching with overlapping medication.
References
1. Korean Statistical Information System (KOSIS). Korea National Statistical Office. accessed on 1 December 2010. Available at http://www.kosis.kr.
2. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004. 27:1047–1053.
3. The Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008. 358:2545–2559.
4. Chen TJ, Chou LF, Hwang SJ. Patterns of ambulatory care utilization in Taiwan. BMC Health Serv Res. 2006. 6:54.
5. Sato T, Takeichi M, Shirahama M, Fukui T, Gude JK. Doctor-shopping patients and users of alternative medicine among Japanese primary care patients. Gen Hosp Psychiatry. 1995. 17:115–125.
6. Lo AY, Hedley AJ, Pei GK, Ong SG, Ho LM, Fielding R, Cheng KK, Daniel L. Doctor-shopping in Hong Kong: implications for quality of care. Int J Qual Health Care. 1994. 6:371–381.
7. Bates DW, Boyle DL, Vander Vliet MB, Schneider J, Leape L. Relationship between medication errors and adverse drug events. J Gen Intern Med. 1995. 10:199–205.
8. Hong JS, Kang HC, Kim J. Continuity of care for elderly patients with diabetes mellitus, hypertension, asthma, and chronic obstructive pulmonary disease in Korea. J Korean Med Sci. 2010. 25:1259–1271.
9. Juurlink DN, Mamdani M, Kopp A, Laupacis A, Redelmeier DA. Drug-drug interactions among elderly patients hospitalized for drug toxicity. JAMA. 2003. 289:1652–1658.
10. Gurwitz JH, Field TS, Harrold LR, Rothschild J, Debellis K, Seger AC, Cadoret C, Fish LS, Garber L, Kelleher M, Bates DW. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA. 2003. 289:1107–1116.
11. Tamblyn RM, McLeod PJ, Abrahamowicz M, Laprise R. Do too many cooks spoil the broth? Multiple physician involvement in medical management of elderly patients and potentially inappropriate drug combinations. Can Med Assoc J. 1996. 154:1177–1184.
12. Wang MJ, Lin SP. Study on doctor shopping behavior: insight from patients with upper respiratory tract infection in Taiwan. Health Policy. 2010. 94:61–67.
13. Kwon S. Payment system reform for health care providers in Korea. Health Policy Plan. 2003. 18:84–92.
14. Oh JY. Treatment guideline for diabetes. Korean J Med. 2008. 75:249–256.
15. Nathan DM, Buse JB, Davidson MB, Heine RJ, Holman RR, Sherwin R, Zinman B. Management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2006. 29:1963–1972.
16. Tobi H, Faber A, van den Berg PB, Drane JW, de Jong-van den Berg LT. Studying co-medication patterns: the impact of definitions. Pharmacoepidemiol Drug Saf. 2007. 16:405–411.
17. Lee R, Cheong YS, Park EW, Choi EY, Kim KS, Sim SK, Park JY, Yeoum HT, Jeong EJ, Kim SY, Suhmoon S, Lee SJ, Kim JT, Kang KH. Referral patern of family practitioners: Cheonan practice-based research network study. J Korean Acad Fam Med. 2007. 28:286–291.
18. Chen YC, Hwang SJ, Lai HY, Chen TJ, Lin MH, Chen LK, Lee CH. Potentially inappropriate medication for emergency department visits by elderly patients in Taiwan. Pharmacoepidemiol Drug Saf. 2009. 18:53–61.
19. Kandrack MA, Grant KR, Segall A. Gender differences in health related behaviour: some unanswered questions. Soc Sci Med. 1991. 32:579–590.
20. Kasteler J, Kane R, Olsen DM, Thetford C. Issues underlying prevalence of "doctor-shopping" behavior. J Health Soc Behav. 1976. 17:329–339.
21. Chin MH, Cook S, Jin L, Drum ML, Harrison JF, Koppert J, Thiel F, Harrand AG, Schaefer CT, Takashima HT, Chiu SC. Barriers to providing diabetes care in community health centers. Diabetes Care. 2001. 24:268–274.
22. Demers M. Frequent users of ambulatory health care in Quebec: the case of doctor-shoppers. Can Med Assoc J. 1995. 153:37–42.
23. Drivsholm T, de Fine Olivarius N. General practitioners may diagnose type 2 diabetes mellitus at an early disease stage in patients they know well. Fam Pract. 2006. 23:192–197.
24. Speedling EJ, Rose DN. Building an effective doctor-patient relationship: from patient satisfaction to patient participation. Soc Sci Med. 1985. 21:115–120.
25. Delbanco TL. Enriching the doctor-patient relationship by inviting the patient's perspective. Ann Intern Med. 1992. 116:414–418.
26. Katz N, Panas L, Kim M, Audet AD, Bilansky A, Eadie J, Kreiner P, Paillard FC, Thomas C, Carrow G. Usefulness of prescription monitoring programs for surveillance: analysis of Schedule II opioid prescription data in Massachusetts, 1996-2006. Pharmacoepidemiol Drug Saf. 2010. 19:115–123.
27. Hall AJ, Logan JE, Toblin RL, Kaplan JA, Kraner JC, Bixler D, Crosby AE, Paulozzi LJ. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA. 2008. 300:2613–2620.
28. Han D, Kim B, Lee Y, Bae S, Kwon S. An evaluative analysis of the referral system for insurance patients. Korean J Prev Med. 1991. 24:485–495.
29. Park IB, Kim DJ, Kim J, Kim H, Kim H, Min KW, Park SW, Park JH, Baik SH, Son HS, Ahn CW, Oh JY, Lee S, Lee J, Chung CH, Choi I, Choi KM. Current status of aspirin user in Korean diabetic patients using Korean health insurance database. J Korean Diabetes Assoc. 2006. 30:363–371.
30. Online Prospective DUR Program. Korea Health Insurance Review and Assessment Servie. accessed on 1 May 2011. Available at http://www.hira.or.kr/common/dummy.jsp?pgmid=HIRAA030030000000.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download