Abstract
A single measurement of serum 17α-hydroxyprogesterone (17OHP) level can be unreliable because of its marked diurnal variation. We investigated the relationship of serum level of 17OHP with that of androstenedione (AD), which shows a smaller diurnal variation. And we tested whether the responses of these two hormones to low-dose ACTH stimulation are correlated in patients with 21-hydroxylase deficiency. Baseline serum 17OHP and AD levels were measured in 87 patients and a low-dose ACTH stimulation test was performed in 41 patients. The basal 17OHP level correlated positively with the basal AD level independently of sex, type of 21-hydroxylase deficiency, and the time of day of blood sampling (n = 87, R2 = 0.75, P < 0.001). The area under the curve of 17OHP and AD correlated positively with their respective basal levels. The fold-change increase in 17OHP after ACTH injection correlated negatively with the basal 17OHP level, but that of AD did not correlate with the basal AD level. The random serum 17OHP level, used in the clinic, is a reliable guide and a low-dose ACTH stimulation test provides no extra benefit for assessing the treatment adequacy in patients with 21-hydroxylase deficiency.
21-Hydroxylase deficiency is the most common cause of congenital adrenal hyperplasia (CAH), which accounts for about 95% of all forms of CAH. The inability to convert 17α-hydroxyprogesterone (17OHP) to 11-deoxycortisol causes cortisol deficiency and the accumulation of 17OHP. From 1940, 24 hr urine samples were analyzed to measure the levels of the 17-ketogenic steroids, such as 17-ketosteroid and 17-hydroxycorticosteroid, to diagnose this disorder and to monitor the adequacy of therapy (1). However, 24 hr urine samples was difficult to collect, and measurement of these urinary hormones was often unreliable in those days (2). Measurement of serum 17OHP was introduced in 1968 (3), and it is now used most widely for the diagnosis and assessment of the adequacy of treatment (4). Measurement of serum androstenedione (AD) level was introduced at a similar time (5) and has been used to monitor the adequacy of treatment in some studies since the late 1970s (2, 6, 7).
A single determination of serum 17OHP level does not always reflect the adequacy of therapy in CAH patients because of its marked diurnal variation (8) and rapid changes in its concentration after a single dose of oral or intramuscular glucocorticoid (2). By contrast, serum AD level has a smaller diurnal variation than serum 17OHP and is not affected immediately by a single dose of oral or intramuscular glucocorticoid (2). Some studies have reported that serum AD level gives a more accurate parameter for assessing the adequacy of therapy for this disorder (2, 6, 7). However, measurement of serum AD level is not available in practice because of the national medical insurance uncoverage in Korea. It is measured in a private laboratory or the blood samples are sent to foreign laboratories for testing.
Adrenal stimulation with adrenocorticotropic hormone (ACTH) is the principal challenge test used to estimate the relative activity of adrenocortical enzymes (9) and is used in the biochemical diagnosis of CAH (10). Low-dose (1 µg) ACTH stimulation test is accepted as the standard test of the pituitary-adrenal function and to investigate physiologic adrenal sensitivity (11). However, there are insufficient data about the response of adrenal steroidogenesis to low-dose ACTH stimulation in patients with CAH who take glucocorticoid medication. We hypothesized that the exaggerated serum 17OHP and AD responses to 1 µg ACTH might reflect poor control of the adrenal enzyme defect in CAH patients (12).
We performed this study to observe the relationship between serum 17OHP and AD levels, and to investigate whether these two hormonal responses to low-dose ACTH stimulation correlate with each other in patients with CAH caused by 21-hydroxylase deficiency.
Eighty-seven patients (46 males and 41 females) being treated for CAH caused by 21-hydroxylase deficiency were included. The patients, who were not reached to their final adult height, were excluded. Of the 87 patients, 57 (65.5%) had the salt-wasting (SW) type and 30 (34.5%) had the simple virilizing (SV) type. Their mean age at the time of the study was 19.1 ± 4.5 yr. No patient had clinical or biochemical evidence of hepatic or renal diseases, and none was taking medications except for glucocorticoid and mineralocorticoid drugs.
Patients visited the outpatient clinic for regular follow up, and standard anthropometric measurements were obtained. In general, most patients with CAH achieve a final adult height (FAH) less than their target height (13). Therefore, the FAH, expressed as a standard deviation score (SDS), was corrected for genetic potential (FAH SDS minus midparental height SDS). We also reviewed the medical records to check the time of diagnosis, dose of medications at the time of blood sampling, and recent plasma renin activity (PRA) levels. Disease duration was calculated as time of diagnosis to the time of blood sampling.
Between July 2010 and August 2010, blood was drawn in all patients at random times, regardless of the timing of the medications, for analysis of baseline serum 17OHP and AD concentrations. The low-dose ACTH stimulation test was performed in 41 patients who agreed to participate with the test protocol. We arbitrarily divided the sampling time into two sessions, 0900-1200 hr (morning) and 1200-1600 hr (afternoon), because serum 17OHP concentration was expected to be high in the morning (14). Blood samples were collected from 31 patients in the morning and 56 patients in the afternoon.
An indwelling catheter was inserted at least 10 min before sampling to allow a period of adaptation. One microgram of tetracosactide acetate (Synacthen®, Ciba Geigy, Basle, Switzerland) was given intravenously to stimulate adrenal steroidogenesis and release. Blood was collected immediately before and after 1 hr the injection of Synacthen. The samples were centrifuged and separated, and the serum was stored at -20℃ until the assays.
17OHP concentration was measured using the Coat-A-Count assay (Siemens Medical Solutions Diagnostics, Los Angeles, CA, USA). This is a solid-phase radioimmunoassay (RIA) with a sensitivity of 0.07 ng/mL. The intraassay coefficient of variation (CV) was 7.1% at a serum concentration of 1.4 ng/mL, and the interassay CV was 7.3% at a serum concentration of 1.5 ng/mL.
AD concentration was measured using the Coat-A-Count assay (Siemens Medical Solutions Diagnostics). This is a solid-phase RIA with a sensitivity of 0.04 ng/mL. The intraassay CV was 5.0% at a serum concentration of 1.0 ng/mL, and the interassay CV was 7.0% at a serum concentration of 1.0 ng/mL.
The biochemical data are presented as median and range (minimum, maximum) and the other continuous data are shown as mean ± SD. Statistical analyses were performed using SPSS 17.0 for Windows (SPSS Inc., Chicago, IL, USA). The biochemical data, 17OHP and AD concentrations, and PRA levels, were transformed to logarithmic values to make them parametric. The two groups were classified according to sex, type of CAH, and the time of blood sampling, and were then compared by Student's t test and the chi-square test. Pearson's correlation coefficient was used to identify correlations between biochemical variables. Fisher's Z transformation was used to compare two correlation matrices. The response to ACTH stimulation was calculated two ways: 1) the fold-change increment, determined as the ratio of the peak level to basal value and 2) the overall response, determined by the area under the curve (AUC) for the response to ACTH of 17OHP and AD concentrations. Simple comparisons between the basal and peak biochemical values were analyzed using a paired t test. Because of the unbalanced distribution of the main serum predictors, we did not adjust for other variables (for example, by using a logistic regression model). P values < 0.050 were considered significant.
At the time of blood sampling, the mean age was greater in the patients with the SV type than in those with the SW type, but the disease duration did not differ significantly according to type of disease. Except for the sex ratio, the corrected FAH SDS, body mass index (BMI) SDS, and dose of medications did not differ between the SV and SW patients (Table 1). However, the mean corrected FAH SDS was lower in males than in females (male, -1.72 ± 1.27 vs female, -0.93 ± 1.05; P = 0.002). BMI SDS did not differ between males and females (Table 2).
The median basal concentrations of serum 17OHP, AD, and PRA in the 87 patients were 28.00 (0.10, 608.00) ng/mL, 3.18 (0.15, 36.85) ng/mL, and 11.1 (0.1, 86.0) ng/mL/h, respectively. These values did not differ significantly between males and females (Table 2), between SV and SW patients, or between different blood sampling times.
The basal 17OHP concentration correlated positively with the basal AD concentration (n = 87, R2 = 0.75, P < 0.001). The correlation coefficient was bigger in the morning samples (n = 31, R2 = 0.81, P < 0.001) than in the afternoon samples (n = 56, R2 = 0.70, P < 0.001), although this difference was not significant (Fig. 1). The correlation between basal serum levels of 17OHP and AD was not related to sex or type of CAH.
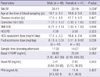
The median peak serum 17OHP concentration was 77.80 (1.46, 486.00) ng/mL and the peak serum AD concentration was 4.20 (0.72, 40.75) ng/mL in 41 patients. Both peak levels were significantly higher than their basal levels (17OHP, P < 0.001; AD, P = 0.015) (Fig. 2) and for each markers, the basal and peak levels correlated significantly (17OHP, R2 = 0.82, P < 0.001; AD, R2 = 0.89, P < 0.001). The AUC of 17OHP and AD correlated positively with their respective basal levels (17OHP, R2 = 0.93, P < 0.001; AD, R2 = 0.97, P < 0.001) (Fig. 3A, B). The peak levels and AUC of these biochemical markers did not differ between males and females, according to the type of CAH, or between blood sampling times (Table 3).
The fold-change increment in 17OHP concentration after the low-dose ACTH injection correlated negatively with the basal 17OHP concentration (R2 = 0.50, P < 0.001) but did not differ between males and females, between type of CAH, or between blood sample times. The median increment in AD concentration was 1.13-fold, and this value did not correlate significantly with the basal AD concentration (Fig. 3C, D).
The recent clinical guidelines suggest the target levels of multiple adrenal hormones, such as 17OHP and AD, and recommend glucocorticoid dose titration according to the target levels (15-17). In our study, the basal serum 17OHP concentration correlated well with that of serum AD irrespective of sex, CAH type, and the time of blood sampling. This result suggests that measuring serum AD concentration gives no additional information for assessing the treatment in these patients.
Cavallo et al. (2) reported that serum AD level correlates well with urinary 17-ketosteroid level and with clinical control in CAH patients. In their study, serum AD level was normal in most patients with good control, regardless of the time of the day when the blood sample was obtained, but it was elevated in all patients with poor control. Conway et al. (12) showed that the serum AD response was normal in adequately treated patients. Ilondo et al. (18) reported that serum 17OHP level varies widely irrespective of the degree of control and can be abnormally high even in patients with good clinical and biochemical control. All of these researchers suggested that the serum AD level is better than the serum 17OHP level for monitoring therapy in patients with CAH. However, a single serum determination of androgen level may not reflect total daily androgen secretion because of the known episodic and diurnal variation of secretion (19). Some recommend that three or four determinations are needed throughout the day to provide a reliable indicator of the control of treatment (20). By contrast, one study that used continuous 24 hr sampling suggested that serum AD level exhibits relatively small fluctuations and that random samples are likely to be representative (7). The question whether a single measurement of serum AD level is adequate remains controversial. Because we did not apply a clinical standard of disease control in our study, we could not directly compare the accuracy of serum 17OHP and AD levels. However, our data suggest that information about the disease control status based on the serum 17OHP level is the same as that based on both serum 17OHP and AD levels.
The correlation between basal 17OHP and AD concentrations tended to be strongest in the morning. This observation is similar to that reported by Charmandari et al. (14), who also found that the morning sample, taken before the oral dose of hydrocortisone, is most accurate for assessing disease control status. In our study, we could not accurately predict the degree of suppression of the pituitary-adrenal axis by glucocorticoids because of variable sampling times. Further investigation of the glucocorticoid effect should be needed.
We expected that patients with poor control would have a high basal level and an exaggerated peak response of 17OHP after low-dose ACTH administration and vice versa. In contrast to our expectation, the fold-change increment in serum 17OHP level after ACTH administration correlated negatively with the basal level, suggesting that ACTH stimulation test provides no additional information for assessing the adequacy of treatment. The patients with low serum 17OHP level had a greater fold-change increment in serum 17OHP level. However, we could not interpret this clinical meaning because of the absence of normal data for the control group. The fold-change increment was smaller for serum AD level than for serum 17OHP level, although the peak AD level was significantly higher than the basal AD level. These data suggest that the low-dose ACTH stimulation test was not effective in assessing the degree of disease control in CAH patients in our study.
A limitation of our study was the absence of a gold standard to assess disease control in our patients. In prepubertal and pubertal patients, growth velocity and bone age advancement are key components for determining the degree of clinical control. However, there are no clinical criteria that can be used for postpubertal patients in the outpatient clinic. Some have used 24 hr urinary 17-ketosteroid excretion (6, 7) but this test cannot be performed practically. And because the insufficiency of glucocorticoid and/or mineralocorticoid therapy may take several months to appear as virilization and hyperpigmentation, serum 17OHP and/or AD levels may increase before these clinical signs become obvious. Another limitation of our study was the absence of data from the ACTH stimulation test in a normal control group to compare with the results in the patients.
In conclusion, serum 17OHP concentration correlates well with serum AD concentration independently of sex, type of CAH, and the time of day of blood sampling. The low-dose ACTH stimulation test does not provide additional information for assessing the treatment adequacy in patients with CAH. Therefore the random serum 17OHP level, as currently measured in the clinic, appears to be a reliable guide for the management of patients with CAH.
Figures and Tables
Fig. 1
The relationship between basal levels of serum 17OHP and AD. The basal hormone levels were correlated positively with each other in all patients (A). The correlation coefficient was higher in the morning samples (B) than in afternoon samples (C). Conversion factors: 17OHP, ng/mL × 3.02 → nM/L; AD, ng/mL × 3.49 → nM/L.
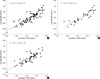
Fig. 2
The basal and peak hormone levels after the low-dose ACTH stimulation test. (A) 17OHP. (B) AD. Both peak levels were significantly higher than their respective basal levels (17OHP, P < 0.001; AD, P = 0.015). Conversion factors: 17OHP, ng/mL × 3.02 → nM/L; AD, ng/mL × 3.49 → nM/L.

Fig. 3
Simple correlations of the basal hormone levels with their responses to ACTH stimulation. (A, B) Overall responses. (C, D) The fold-change increments. Conversion factors: 17OHP, ng/mL × 3.02 → nM/L; AD, ng/mL × 3.49 → nM/L.
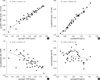
Table 2
Comparison of clinical characteristics and basal levels of serum 17OHP and AD between males and females
Data are expressed as mean ± standard deviation or median (range). *by chi-square test. SW, salt-wasting CAH; SV, simple virilizing CAH; FAH, final adult height; SDS, standard deviation score; BMI, body mass index; HCS, hydrocortisone; PD, prednisolone; 17OHP, 17α-hydroxyprogesterone; AD, androstenedione, PRA, plasma renin activity. Conversion factors: 17OHP, ng/mL × 3.02 → nM/L; AD, ng/mL × 3.49 → nM/L.
ACKNOWLEDGMENTS
We acknowledge the assistance of Tae Hun Kim, a senior technologist at the Department of Nuclear Medicine at Seoul National University Hospital, in the measurements of serum 17-hydroxyprogesterone and androstenedione levels.
AUTHOR SUMMARY
Relationships of Basal Level of Serum 17-Hydroxyprogesterone with that of Serum Androstenedione and Their Stimulated Responses to a Low Dose of ACTH in Young Adult Patients with Congenital Adrenal Hyperplasia due to 21-Hydroxylase Deficiency
Min Jae Kang, Shin Mi Kim, Young Ah Lee, Choong Ho Shin and Sei Won Yang
Because a single measurement of serum 17α-hydroxyprogesterone (17OHP) level can be unreliable due to its diurnal variation, we investigated the relationship between serum level of 17OHP and androstenedione (AD). Our results indicate that the basal 17OHP level correlated positively with the basal AD level that has smaller diurnal variation. However, the foldchange increase of both hormones after ACTH injection showed no consistent result. The random serum 17OHP level may be a reliable guide and a lowdose ACTH stimulation test provides no extra benefit for assessing the treatment adequacy in patients with 21-hydroxylase deficiency.
References
1. Gardner R, Snaith AH. The urinary excretion of 17-hydroxysteroids in children. Arch Dis Child. 1958. 33:305–306.
2. Cavallo A, Corn C, Bryan GT, Meyer WJ III. The use of plasma androstenedione in monitoring therapy of patients with congenital adrenal hyperplasia. J Pediatr. 1979. 95:33–37.
3. Strott CA, Lipsett MB. Measurement of 17-hydroxyprogesterone in human plasma. J Clin Endocrinol Metab. 1968. 28:1426–1430.
4. Barnes ND, Atherden SM. Diagnosis of congenital adrenal hyperplasia by measurement of plasma 17-hydroxyprogesterone. Arch Dis Child. 1972. 47:62–65.
5. Horton R, Frasier SD. Androstenedione and its conversion to plasma testosterone in congenital adrenal hyperplasia. J Clin Invest. 1967. 46:1003–1009.
6. Korth-Schutz S, Virdis R, Saenger P, Chow DM, Levine LS, New MI. Serum androgens as a continuing index of adequacy of treatment of congenital adrenal hyperplasia. J Clin Endocrinol Metab. 1978. 46:452–458.
7. Keenan BS, McNeel R, Barrett GN, Holcombe JH, Kirkland RT, Clayton GW. Plasma androgens in congenital adrenal hyperplasia: androstenedione concentration as an index of adrenal androgen suppression. J Lab Clin Med. 1979. 94:799–808.
8. Strott CA, Yoshimi T, Lipsett MB. Plasma progesterone and 17-hydroxyprogesterone in normal men and children with congenital adrenal hyperplasia. J Clin Invest. 1969. 48:930–939.
9. Colak R, Keleştimur F, Unlühizarci K, Bayram F, Sahin Y, Tutuş A. A comparison between the effects of low dose (1 microg) and standard dose (250 microg) ACTH stimulation tests on adrenal P450c17alpha enzyme activity in women with polycystic ovary syndrome. Eur J Endocrinol. 2002. 147:473–477.
10. Unlühizarci K, Keleştimur F, Güven M, Bayram F, Colak R. The value of low dose (1 microg) ACTH stimulation test in the investigation of non-classic adrenal hyperplasia due to 11beta-hydroxylase deficiency. Exp Clin Endocrinol Diabetes. 2002. 110:381–385.
11. Luboshitzky R, Ishai A, Shen-Or Z, Herer P. Evaluation of the pituitary-adrenal axis in hyperandrogenic women with polycystic ovary syndrome. Neuro Endocrinol Lett. 2003. 24:249–254.
12. Conway DI, Anderson DC, Bu'lock DE. The steroid response to controlled adrenal stimulation in congenital adrenal hyperplasia. Clin Endocrinol (Oxf). 1982. 16:215–226.
13. Yi KH. Effect on final height of gonadotropin-releasing hormone agonist (GnRHa) in children with congenital adrenal hyperplasia. J Korean Soc Pediatr Endocrinol. 2005. 10:50–56.
14. Charmandari E, Matthews DR, Johnston A, Brook CG, Hindmarsh PC. Serum cortisol and 17-hydroxyprogesterone interrelation in classic 21-hydroxylase deficiency: is current replacement therapy satisfactory? J Clin Endocrinol Metab. 2001. 86:4679–4685.
15. Hindmarsh PC. Management of the child with congenital adrenal hyperplasia. Best Pract Res Clin Endocrinol Metab. 2009. 23:193–208.
16. Speiser PW, White PC. Congenital adrenal hyperplasia. N Engl J Med. 2003. 349:776–788.
17. Speiser PW, Azziz R, Baskin LS, Ghizzoni L, Hensle TW, Merke DP, Meyer-Bahlburg HF, Miller WL, Montori VM, Oberfield SE, Ritzen M, White PC. Endocrine Society. Congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010. 95:4133–4160.
18. Ilondo MM, Vanderschueren-Lodeweyckx M, Pizarro M, Vlietinck R, Malvaux P, Eggermont E, Eeckels R. Plasma levels of androgens and 17 alpha-OH-progesterone as an index of the adequacy of treatment in congenital adrenal hyperplasia. Horm Res. 1983. 18:175–185.
19. Ghizzoni L, Bernasconi S, Virdis R, Vottero A, Ziveri M, Volta C, Iughetti L, Giovannelli G. Dynamics of 24-hour pulsatile cortisol, 17-hydroxyprogesterone, and androstenedione release in prepubertal patients with non-classic 21-hydroxylase deficiency and normal prepubertal children. Metabolism. 1994. 43:372–377.
20. von Schnakenburg K, Bidlingmaier F, Knorr D. 17-hydroxyprogesterone, androstenedione, and testosterone in normal children and in prepubertal patients with congenital adrenal hyperplasia. Eur J Pediatr. 1980. 133:259–267.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download