Abstract
This study was designed to identify the causes of the development of carpal tunnel syndrome (CTS) associated with end stage kidney disease (ESKD). A total of 112 patients with ESKD, 64 on hemodialysis (HD) and 48 on peritoneal dialysis (PD), were enrolled. The duration of ESKD and dialysis, the site of the arteriovenous (A-V) fistula for HD, laboratory data such as blood urea nitrogen, creatinine, and beta-2-microglobulin were determined. Clinical evaluation of CTS and electrophysiological studies for the diagnosis of CTS and peripheral neuropathy were performed. The electrophysiological studies showed that the frequency of CTS was not different in the HD and PD groups (P = 0.823) and the frequency of CTS was not different in the limb with the A-V fistula compared to the contralateral limb (P = 0.816). The frequency of HD and PD were not related to beta-2-microglobulin levels, an indicator of amyloidosis. The frequency of CTS did not increase as the severity of the peripheral neuropathy and the duration of ESKD and dialysis increased (P = 0.307). The results of this study do not support that microglobulin induced amyloidosis or placement of an A-V fistula are associated with an increase in CTS.
Neuropathy is a common complication of end stage kidney disease (ESKD), typically presenting with a distal symmetric pattern with greater involvement of the lower extremities compared to the upper extremities (1). However, in addition to the distal symmetric peripheral neuropathy (PN), mononeuropathies have been reported to occur with increased frequency in patients with ESKD, and most typically affect the median, ulnar, and femoral nerves (2). Carpal tunnel syndrome (CTS) is the most common mononeuropathy in patients with ESKD with a frequency of 8% to 31% (3, 4). Microglobulin amyloidosis has been reported as the major cause of the development of CTS (5). Amyloid deposits have been identified in synovial specimens from dialysis patients with CTS. In addition, there is an increase in the frequency of CTS associated with increasing durations of hemodialysis (HD) (5). Other factors proposed as causes of CTS include: uremic tumoral calcinosis (6) and placement of an arteriovenous (A-V) fistula inducing diversion of blood from the distal limbs (7, 8). In a recent study (9), the frequency of CTS was 30.5% in the limbs with a fistula and 12.2% in the contralateral limb. However, the exact causes of the development of CTS in ESKD are not known. In addition, many prior studies did not perform electrophysiological studies for the diagnosis of CTS and did not consider the differential diagnosis for coexisting PN and CTS.
This study was designed to identify the mechanisms of the development of CTS using electrophysiological studies in patients with ESKD.
One hundred twelve patients with ESKD were prospectively evaluated for CTS. Sixty four patients were on HD and 48 were on peritoneal dialysis (PD). There were 34 females and 30 males with a mean age of 57.8 ± 13.0 (range: 24-78 yr) in the HD group and 23 females and 25 males (mean age, 52.7 ± 12.4; range, 25-79 yr) in the PD group. Exclusion criteria were: 1) a history of fracture or trauma of an upper limb that could cause focal nerve injury, 2) metabolic disease other than diabetes mellitus, 3) patients that could not tolerate electrical stimulation.
Data on the duration of ESKD and dialysis, site of the A-V fistula in the patients on HD and additional medical illness were noted after review of the medical records. In addition, laboratory data such as blood urea nitrogen, creatinine, and beta-2-microglobulin were recorded. Clinical evaluation included the symptoms and signs of CTS and electrophysiological studies for diagnosis of CTS and PN were performed in less than 2 weeks after the laboratory examinations. The clinical and electrophysiological evaluations were conducted by two experienced physiatrists. For the clinical evaluation, subjective symptoms such as numbness of lateral four fingers, pain and stiffness of the hands were assessed. Muscle strength of the abductor pollicis brevis (APB), sensory impairment of median nerve distribution, and the Tinel's sign and Phalen test were assessed objectively. The patients who had more than two symptoms and/or signs of five (numbness of lateral four fingers, APB weakness, hypesthesia of median nerve distribution, Tinel sign, Phalen test) were considered to have 'clinical CTS'. The patients who also had numbness and hypesthesia of little finger and those revealed the provocative tests only were not diagnosed with clinical CTS.
Nerve conduction studies were performed using a Counterpoint MK2 (Dantec, Copenhagen, Denmark). The median, ulnar, peroneal, and tibial motor nerves and median, ulnar, and sural sensory nerves were evaluated using standard conduction techniques. The distance between the recording electrode and stimulation was 8 cm in all of the compound muscle action potential (CMAP) recordings and was 14 cm for the sensory nerve action potential (SNAP) recordings. The F waves of all the motor nerves and the H reflex were also evaluated. Skin temperature was maintained at 32℃ or above in the upper extremity nerves and 30℃ or above in the lower extremity nerves. PN was diagnosed and graded I to IV based on the criteria of our laboratory, a modification of the diabetes control and complication trial (DCCT) research group (10). CTS was diagnosed when the findings met at least one of the following regardless of the presence or absence of a PN: 1) ratio of median sensory latency of a 7 cm wrist segment to a 7 cm palm segment > 2.0, 2) ratio of distal latency of a median SNAP to that of an ulnar SNAP > 1.2, 3) ratio of the amplitude of a median sensory SNAP with wrist stimulation to that with palm stimulation < 0.5, 4) ratio of the distal latency of a median CMAP to an ulnar CMAP > 1.5, 5) ratio of the amplitude of a median CMAP to an ulnar CMAP < 0.6. These cut off values are obtained from the 50 healthy volunteers aging from 26 to 75 (mean age, 55.2 ± 12.0 yr).
The frequency of CTS was compared between PD and HD groups using the chi-square test. The correlation between beta-2-microglobulin levels and the duration of ESKD was analyzed; the levels of beta-2-microglobulin were analyzed using the independent t-test. The software used for statistical analysis was SPSS 12.0 (SPSS Inc., Chicago, IL, USA) and the significance level was set at a P < 0.05.
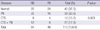
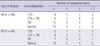
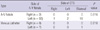
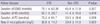
The mean duration on HD and PD was 45.6 ± 41.9 and 59.4 ± 44.7 months, respectively. The duration of dialysis, BUN, creatinine, potassium, and uric acid were not significantly different between HD and PD groups. On clinical evaluation, 18 patients were categorized as having clinical CTS in the patients on HD and 11 in patients on PD. Based on the electrophysiological studies, 42 out of 64 patients on HD were classified with a PN and/or CTS; 22 with a PN only, 8 with CTS only; and 12 with both. Among the 48 patients on PD a PN developed in 16, CTS in 4, and both in 8 (Table 1). The frequency of CTS was not different in comparisons between the HD and PD groups (P = 0.823). Among the patients with 'clinical CTS', three in the HD group and four in the PD group had no electrophysiological abnormalities; the other patients were electrophysiologically diagnosed with CTS and/or a PN (Table 2). The frequency of CTS was not different between the limb with an A-V fistula and the contralateral limb (Table 3) (P = 0.816). The duration of ESKD, dialysis and beta-2-microglobulin levels were not significantly different between the CTS group and non-CTS group (Table 4).
The development of uremic neuropathy has been related previously to the retention of neurotoxic molecules in the middle molecular range. Nerves of uremic patients have shown to exist in a chronically depolarized state prior to dialysis, with subsequent improvement and normalization of resting membrane potential after dialysis. The degree of depolarization correlates with serum potassium, suggesting that chronic hyperkalemic depolarization plays an important role in the development of nerve dysfunction in ESKD (1).
Patients with ESKD frequently complain of a numbness and tingling sensation of the hands and feet. The potential causes of these symptoms are numerous. Distal symmetric PN may cause symptoms more frequently in the feet; the symptoms in the upper extremity may be caused by an A-V fistula or mononeuropathies. Recently, mononeuropathies in patients on dialysis, caused by entrapment at sites that are physiologically prone to stenosis, has become a topic of interest, such as ulnar neuropathy at the elbow and median neuropathy at the carpal tunnel (11, 12). However, the etiology remains unknown and the frequency varies widely according to the criteria and methods used for the diagnosis.
In a report on the association between CTS and A-V fistulas in patients on HD (13), clinical CTS was more frequently diagnosed in the wrist with an A-V fistula; however, electrodiagnostic studies did not indicate any significant association between the frequency of CTS and the A-V fistula or its duration. Such reports raise questions about the validity of electrodiagnostic results in patients with an A-V fistula, because of the discrepancy between the clinical and electrodiagnostic findings. However, only median and ulnar motor conduction studies were performed for the diagnosis of CTS. In this study, precise criteria for the diagnosis of PN and CTS, with or without a PN, were used. The frequencies of clinical and electrodiagnostic CTS were similar: 24/4, 20/64 and 13/48, 12/48 in the HD and PD groups, respectively. However, there was some discrepancy between the clinical and electrophysiological diagnosis; the patients with clinical CTS had PN due to ESKD but some of the patients diagnosed electrophysiologically were asymptomatic. The electrophysiological findings are more objective than the clinical symptoms and/or signs; the clinical findings of PN can be due to ESKD even with normal electrodiagnostic findings. Therefore, we investigated the frequency and correlation of CTS with the clinical variables based on the electrodiagnosis.
A prior study found no difference in the frequency of CTS in patients undergoing PD or HD (14). Similarly, the electrodiagnostic confirmation of CTS was not associated with the type of dialysis in this study. Many investigators have reported a positive correlation between the frequency of CTS and the duration of HD (3, 5), and have also reported that the side of the A-V fistula could affect the frequency of CTS (12, 13). However, the results of this study do not reveal the relationship between the frequency of electrodiagnostic CTS and the duration of ESKD, dialysis, and the side of the A-V fistula. These differences could be explained by the fact that most of the prior investigators used the clinical findings only for the diagnosis of CTS.
Since both PN and CTS can cause pain and/or numbness of the hands, the differentiation of the two entities is important in the management of patients. We used separate electrodiagnostic criteria to diagnose the PN and the CTS, because ESKD can induce uremic neuropathy. We also investigated the frequency of CTS according to the severity of the PN, and found no significant association. This might in part be due to the difficulty in the differentiation of the two entities in severe cases with a PN.
The effect of cervical complications such as spondyloarthropathy, common in patients on long term HD, can induce cervical radiculopathy or myelopathy (15). These factors are also an important consideration in patients with symptoms and/or signs without evidence of CTS or a PN. We performed nerve conduction studies without needle electromyography in this study, to avoid patient discomfort, the cases with clinical CTS and normal electrophysiological findings might have had a cervical radiculopathy.
In the reports on patients receiving long-term HD, the frequency of beta-2-microglobulin related osteoarthropathy increased steadily with the length of survival, and the frequency of CTS increased with the number of years on dialysis (5). Another investigation on patients undergoing HD reported no correlation between CTS and the site of vascular access and synovial biopsy of the flexor tendons demonstrated edema without inflammation. These findings suggest that extracellular fluid volume excess in the presence of flexion and immobility during dialysis may be important to the pathogenesis rather than osteoarthropathy (16). In this study, we did not find an association between the frequency of CTS and the level of beta-2-microglobulin or between the side of A-V fistula and the development of CTS. In this investigation, we considered the effect of diabetes mellitus on PN and/or CTS in patients with diabetes and ESKD. We also analyzed the patients without diabetes mellitus separately, however, the results neither revealed the correlations between the variables. We do not think that the development of CTS in patients with preexisting uremic peripheral neuropathy is a special condition, but rather think that the patients with generalized peripheral neuropathy are prone to the development of entrapment neuropathy.
Bicknell et al. (4) reported that nerve dysfunction was independent of the disease underlying renal failure, the side of dialysis access shunt, and the presence or absence of osteodystrophy. They recommended that dialysis patients need frequent nerve conduction studies from the beginning of dialysis to identify CTS early and to avoid irreversible nerve damage. In a report on the management of patients with entrapment neuropathy, surgical intervention successfully relieved all symptoms, but return of normal renal function does not reverse the problem (12). Based on the results of previous recommendations and investigations on the management of entrapment neuropathy in patients with ESKD, early and accurate diagnosis of CTS is important in planning the treatment of such patients.
In conclusion, the results of this study do not support that microglobulins, involved in the development of amyloidosis, and placement of an A-V fistula, are associated with the development of CTS in patients with ESKD.
Figures and Tables
AUTHOR SUMMARY
Carpal Tunnel Syndrome and Peripheral Polyneuropathy in Patients with End Stage Kidney Disease
Hee-Kyu Kwon, Sung-Bom Pyun, Won Yong Cho and Chang Su Boo
Neuropathy is a common complication of end stage kidney disease (ESKD), and carpal tunnel syndrome (CTS) is most common. This study was designed to identify the mechanisms of the development of CTS in patients with ESKD. The electrophysiological studies do not support that microglobulin induced amyloidosis or placement of an A-V fistula are associated with an increase in CTS. The cause of CTS in patients with ESKD is supposed to be a vulnerability of nerves for the development of entrapment neuropathy in the cases with preexisting peripheral neuropathy.
References
1. Krishnan AV, Kiernan MC. Uremic neuropathy: clinical features and new pathophysiological insights. Muscle Nerve. 2007. 35:273–290.
2. Brouns R, De Deyn PP. Neurological complications in renal failure: a review. Clin Neurol Neurosurg. 2004. 107:1–16.
3. Hirasawa Y, Ogura T. Carpal tunnel syndrome in patients on long-term haemodialysis. Scand J Plast Reconstr Surg Hand Surg. 2000. 34:373–381.
4. Bicknell JM, Lim AC, Raroque HG Jr, Tzamaloukas AH. Carpal tunnel syndrome, subclinical median mononeuropathy, and peripheral polyneuropathy: common early complications of chronic peritoneal dialysis and hemodialysis. Arch Phys Med Rehabil. 1991. 72:378–381.
5. Gejyo F, Narita I. Current clinical and pathogenetic understanding of beta2-m amyloidosis in long-term haemodialysis patients. Nephrology (Carlton). 2003. 8:Suppl. S45–S49.
6. Cofan F, Garcia S, Combalia A, Segur JM, Oppenheimer F. Carpal tunnel syndrome secondary to uraemic tumoral calcinosis. Rheumatology (Oxford). 2002. 41:701–703.
7. Harding AE, Le Fanu J. Carpal tunnel syndrome related to antebrachial Cimino-Brescia fistula. J Neurol Neurosurg Psychiatry. 1977. 40:511–513.
8. Kumar S, Trivedi HL, Smith EK. Carpal tunnel syndrome: a complication of arteriovenous fistula in hemodialysis patients. Can Med Assoc J. 1975. 113:1070–1072.
9. Gousheh J, Iranpour A. Association between carpal tunnel syndrome and arteriovenous fistula in hemodialysis patients. Plast Reconstr Surg. 2005. 116:508–513.
10. Diabetes Control and Complications Trial Research Group. The effect of intensive diabetes therapy on the development and progression of neuropathy. Ann Intern Med. 1995. 122:561–568.
11. Jebsen RH, Tenckhoff H, Honet JC. Natural history of uremic polyneuropathy and effects of dialysis. N Engl J Med. 1967. 277:327–333.
12. Delmez JA, Holtmann B, Sicard GA, Goldberg AP, Harter HR. Peripheral nerve entrapment syndromes in chronic hemodialysis patients. Nephron. 1982. 30:118–123.
13. Namazi H, Majd Z. Carpal tunnel syndrome in patients who are receiving long-term renal hemodialysis. Arch Orthop Trauma Surg. 2007. 127:725–728.
14. Benz RL, Siegfried JW, Teehan BP. Carpal tunnel syndrome in dialysis patients: comparison between continuous ambulatory peritoneal dialysis and hemodialysis populations. Am J Kidney Dis. 1988. 11:473–476.
15. Kuntz D, Naveau B, Bardin T, Drueke T, Treves R, Dryll A. Destructive spondylarthropathy in hemodialyzed patients: a new syndrome. Arthritis Rheum. 1984. 27:369–375.
16. Jain VK, Cestero RV, Baum J. Carpal tunnel syndrome in patients undergoing maintenance hemodialysis. JAMA. 1979. 242:2868–2869.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download