Abstract
Neonatal mortality rate (NMR) and infant mortality rate (IMR) are two of the most important indices reflecting the level of public health of a country. In this review, we investigated changes in NMR and IMR in Korea and compared the results with those of Japan, USA, and OECD nations. During the past 20 yr, NMR and IMR have lowered remarkably from 6.6 and 9.9 in 1993 to 1.7 and 3.2 in 2009, respectively, in Korea. It is an impressive finding that Korean IMR (3.2 in 2009) is lower than the average of OECD nations (4.7 in 2008), and USA (6.3 in 2009), although higher than Japanese IMR (2.8 in 2009). The proportion of NMR among the IMR calculation decreased from 66.7% in 1993 to 53.1% in 2009. The reason the value of Korea was higher than Japan but lower than USA was speculated to be an aspect of the health care service system. Several suggestions in perinatal, neonatal and infantile health care such as establishment of perinatal care center, research network system, regionalization, and new policies for care of pre-term and high risk pregnancy, are elucidated to achieve further improvement on NMR and IMR in Korea.
Infant mortality rate (IMR) is one of the most important indices that represent the level of economy, culture, and society, as well as the public health of a country. The importance of IMR has been well known for over one hundred years, based on the statement of Sir Arthur Newsholme, England, 1910, which highlighted that the IMR is the most sensitive index among the ones we have to reflect public welfare and hygiene (1). Among several public health indices, IMR and neonatal mortality rate (NMR) are very important because the improvement of NMR and IMR directly influences the survival rate of the pediatric population.
During the past 60 yr, NMR and IMR have improved greatly in Korea due to government support of various systems, including improvements in the level of health, social and economic development in terms of population health, socio-cultural and economic environment, health care and service system, and the medical system. The first nation-wide IMR and NMR were reported officially in 1993 by the Korea Ministry of Health and Welfare (KMHW), Republic of Korea Government. Before 1993, there were several private Korean reports.
In this review, the changes of NMR and IMR in Korea (last 60 yr) are observed and assessed (covering the last 20 yr of IMR data) in comparison with data from Japan, USA, and member nations in the Organization for Economic Cooperation and Development (OECD). Policies or factors of environmental change that have influenced changes of NMR and IMR in the national health care and service system of Korea, Japan and USA are also analyzed. Based on these factors, we have proposed developmental systems, items, and polices on heath care and disease treatment at the perinatal, neonatal (in particular pre-term infant) and infant stages for further improvement of NMR and IMR in Korea.
The first nation-wide IMR was reported officially in 1993 by the KMHW. Before 1993, there were several private Korean reports and estimation reports by the United Nations (UN). The data between 1941 and 1991 were collected from reports by Park and Park (1981) (1), Han et al. (1996) (2), KMHW (1996) (3), and Han and Kim (1996) (4) as well as the report by the UN for data from 1950 to 2010 (5).
IMR and NMR data after 1993 were sourced from several reports by the Korea Institute for Health and Social Affairs (KIHASA), and by Han et al. (2, 6-10). In addition, KMHW published official reports in 1993 (6), 1996 (11), 1999 (12), 2002 (9), and 2005 (10). The report of Choi et al. (13), the 2007-2008 KIHASA report and the publication of KMHW as 2007 and 2009 Yearbook of Health, Welfare and Family Statistics were also collected for IMR and NMR data (14, 15).
For calculating the IMR of 2007-2009 in Korea, we referred to the 2009 statistics for causes of death reported by Statistics Korea (the Statistical Office of Korea) (16). We also referred to the 2009 OECD statistics (17) and the OECD Health Data 2010 (18), and the IMR and NMR data of OECD. In addition, the WHO health statistics and health information systems (19), WHO mortality database (20), database of Japan Ministry of Health Labour and Welfare (21), and Index Mundi (22) were examined for the infant mortality for data from USA and Japan.
In the present study, the IMR was defined as (yearly number of deaths within 1 yr after birth/total number of births yearly) × 1,000, and the NMR is defined as (yearly number of death within 28 days after birth/total number of births yearly) × 1,000.
Korean IMR data were first published officially by KMHW in 1993. Before that year, most data were reported unofficially. Even in the annual reports of the KMHW yearbook of public health and social statistics, there was no description on IMR between 1955 and 1966. Park and Park (1) reported IMR in 1981 based on the fertility survey of KIHASA in 1971, 1974, and 1976.
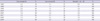
KIHASA performed a survey three times for IMR in 1971, 1974, and 1976 and this has been published in 1981 (1). Table 1 summarizes the Korean IMR reports before 1991. We can recognize the slowly lowering trends of IMR; 350 before 1920, 240-250 in the 1920s, 180-200 in the 1930s, 160 in the 1940s, 150 in the early 1940s, 160 in the late 1940s, 100 during the Korean War, 60 in the early 1960s, 50 in the late 1960s, 30-40 in the 1970s, and 15 in the late 1980s.
Fig. 1 demonstrates the Korean IMR estimate reported by the UN between 1950 and 1990; 138 and 107 in the early and late 1950s, 93 and 81 in the early and late 1960s, 58 and 34 in the early and late 1970s, 27 and 17 in the early and late 1980s, and 9 in the early 1990s.
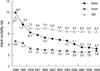
The IMR and NMR in Korea since 1993 are summarized in Fig. 2. A remarkable lowering in IMR was found; 9.9 in 1993, 6.2 in 1999, 5.3 in 2002, 4.7 in 2005, and 3.2 in 2009. Similar changes were found in NMR as well; 6.6 in 1993, 3.8 in 1999, 3.3 in 2002, 2.8 in 2005, and 1.7 in 2009. The pattern of IMR in Korea was shown to be lowering in both of NMR and IMR in the 1-12 month age.
The early NMR (death before 7 days after birth) and the late NMR (death between 7 days and 28 days after birth) from 1993 to 2009 is shown in Table 2. The early NMR is higher than the late NMR implicating that the management of neonates is particularly important in the early neonatal period. The importance of perinatal care and intensive care for babies aged less than 7 days could not be overemphasized.
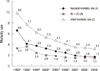
The ratio of NMR in IMR is shown in Fig. 3. The ratio has been decreasing slowly; 66.7% in 1993, 53.2% in 1996, 61.3% in 1999, 62.3% in 2002, 59.6% in 2005, 61.0% in 2006, 57.1% in 2007, 52.9% in 2008, and 53.1% in 2009. According to this data, the NMR still consists of approximately half of IMR, implicating the reduction in NMR could be one of the most important factors of improving IMR in Korea.
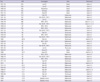
By January 2011, there were a total of 33 member nations in the OECD. In 2010, OECD Health Data for 2008 on the IMR were reported and demonstrated in Fig. 4. We found that the IMR (3.4) of Korea was lower than the mean IMR (4.7) in OECD member nations. In addition, a similar pattern was found throughout 1996, 1999, 2002, 2005, 2006, and 2008 (Fig. 5). The IMR, which is one of the most important health indices, has been lowered in Korea and has been steadily lower than the mean IMR of OECD member nations for the past 15 yr, which is very encouraging data for the national health status.
Changes of IMR in Korea, Japan, and USA for the past 20 yr are compared in Fig. 6. Despite the higher IMR in Korea than in Japan, it is clear that the impressive improvement has been achieved in the view of NMR and IMR in Korea even showing slightly better outcome than those of USA. Recent data on the ratio of NMR in IMR in Korea (53.1%), Japan (46.2%), and USA (71.4%) are shown in Fig. 7. The proportion of NMR in IMR in Korea is slightly lower than the data of USA but higher than the data of Japan.
Over the years, the KMHW of the Korean government has established nationwide programs to promote improved health care for pregnant women, childbirth newborns, and infants (23) such as a test for inborn error of metabolism and care for sick infants (1991), registration of pre-term and congenital abnormal neonates and medical expense support (2000), early diagnosis of deafness (2007), campaign for preventing blindness of preschoolers (2000), prevention of maternal hepatitis B infection (2002), nationwide neonatal intensive care unit (NICU) installation support campaign (2008-2011: project for installing 130 NICU beds in 13 hospitals nationwide), health care for pregnant women and children (2008, provision of providing iron supplements and standard mother-child health record book), project for enhancing health of women at the childbearing age (2005), female reproductive health enhancement program providing information on pregnancy, delivery, infant care, breast feeding clinic, creation of healthy maternal environment (2006), day of pregnant woman, pregnant woman care campaign, medical expense support for pregnancy and delivery of teen-aged pregnant mothers (2011), prevention of artificial abortion, visiting obstetrics and gynecology, prevention of infection and safety accidents at postnatal care houses (2005), post-care for contraception procedure (2005), and infertile couple support project (2006). A project for managing an integrated medical center for high-risk mothers and newborns (e.g. perinatal care center) is also expected to be executed in the following year (2012). Also, Korean Centers for Disease Control and Prevention (Korean CDC) has supported several programs to promote health care for children such as data service, registration, prevention, and control of infectious diseases in children, vaccination support program, survey surveillance, and service for chronic diseases in children.
The medical insurance system began in Korea in 1963. Children under the age of 6 have received a 90% insurance discount from hospital bills, paying only 35% of the insurance salary for outpatient cost, and gaining complete exemption during the neonatal period from 2007. The figures regarding NMR and IMR were presented by the KMHW from 1993 and passed on to Statistics Korea from 2007. In 2007, surveys and statistical analysis methods for infant and maternal death were revised and complemented (24) to develop into a method for calculating more concrete, accurate numbers for NMR and IMR. Such revision and supplementation of the statistics calculation method facilitated a more accurate calculation of NMR and IMR in Korea. Improvement of NMR and IMR in Korea is stipulated to have been achieved by diverse factors, such as the prevention of diseases for newborns and infants (e.g. vaccination), the development of various medical technologies, medicine, tools, and improved nutritional environment, along with the introduction of the previously mentioned programs in Korea. The development of NICUs for preterm, low birth weight infants, and high-risk neonates observed in the past 30 yr in the Korean medical community (25) has also contributed to improvements of NMR and IMR, with the support of activities conducted by related academic societies.
The development of health care policies for improving healthcare of infants presented by the Japan Ministry of Health, Labour and Welfare in Japan (26) show that the following systems have been executed as national projects: the introduction of health care system for raising pre-term babies (1958), medical care expenses for tuberculosis infected children (1958), national health screening program for infants and children (1961), project for researching and treating chronic illness of children and providing health record books for children with certain illnesses (1974), congenital metabolic disorder test and special milk support programs (1977), support for nursing in gestational toxicology (1979), perinatal medical facilities support system (technical operation was achieved by the NICU medical facility repair business of 1979, maternal and fetal ICU and NICU medical facility repair programs of 1984, supporting operative expenses for perinatal medical facility (1996), construction, management, regionalization of complex regional perinatal center, prevention of maternal hepatitis B infection (1985), infant development counseling project (1991), project for providing health care information to mothers and children living abroad (1994), infant health support programs (1994), chronic illness child care support (1996), model for promoting arrangement of nannies in ward (1998), system for raising medical expenses for infants (1990), publication of mother-child health record book (2004), and the New Angel Plan (2000-2004). Furthermore, various health care statistics on perinatal period, neonates, and infants are being accurately analyzed and presented by the bureau of statistics affiliated with the Japanese Ministry of Health, Labour and Welfare. In addition to the activities performed by various academic societies on the perinatal period, newborns, infants, and various diseases, Neonatal Research Network (1999) (27) and Perinatal Care Center Research Network (2003) (28) are being actively managed as networks for conducting and promoting clinical studies on newborns and perinatal period, and are contributing to the registration of patients, data collection, statistics, education, research, and quality improvement. Furthermore, the decrease in the mortality rate of low and extremely low birth weight infants contributed to the improvement of NMR, IMR in Japan (29, 30). It is believed that such factors have helped Japan develop as the nation with the best NMR and IMR in the world (25, 31). Although most systems of Korea have reached a similar level to that of Japan, Korea falls behind in several aspects, such as the installation, operation, and regionalization of perinatal care centers, and lack of installation of a center for co-managing high-risk mothers with neonates. Nationwide networks for infants, newborns, and perinatal period are also lacking. Such aspects must be complemented to achieve greater improvement of NMR and IMF in Korea.
National system support for promoting infantile health in the USA is as follows (26): execution of Medicaid (1965), Medicare (1965), Supplemental Security Income (social health care security programs for children and pregnant women of the lower income group), provision of State Children's Health Insurance Program, Children Vaccine Program, Health Start Program (1991, Early Head Start Program, full day care service, parent education, case management, Community Resource Assistant), Early and Periodic Screening, Diagnostic and Treatment (EPSDT) Service Program (1967), folic acid intake program, and health education and campaign (supine position, HIV infection in mother, teenaged pregnancies, folic acid intake). Along with various activities conducted by diverse related institutes, such as National Institute of Health, a research group for decreasing neonatal and infant mortality, National Institute of Child Health and Human Development, National Heart, Lung, and Blood Institute, and Center for Diseases Control, various statistics have been analyzed and presented on the health status of perinatology, neonates, and infants by the National Vital Statistics System of the National Center for Health Statistics. Moreover, NMR is greatly improved through the enhanced survival rate of pre-term babies and low birth weight infant achieved by the nationwide institute on National Institute of Child Health and Human Development (NICHD), Neonatal Research Network (1986) (32), and Vermont Oxford Network (1988) (33) (25, 34-36).
Nevertheless, USA IMR has been presented as 6.3 in 2009, which is far higher than 4.7, the average rate of OECD in 2008. Also, NMR occupies a much larger portion of IMR in the USA when compared to that of Korea or Japan. The specific reasons for such phenomena are that, unlike Korea or Japan, USA presents problems regarding its different and complex race, sociality, and health care system.
The high IMR of the USA is due to the large IMR differences between races (37). IMR according to race and ethnicity (2008) is presented as 13.35 for non-Hispanic blacks, 8.28 for American Indians or Alaska natives, 8.01 for Puerto Ricans, 5.58 for non-Hispanic whites, 5.34 for Mexicans, 5.08 for Cubans, 4.55 for Asians or Pacific Islanders, and 4.52 for Central and South Americans, thus presenting at least 3 fold deviation between races. These figures have not changed greatly since 2000. Such differences can be partly explained by the individually different standards of risk factors between races, such as pre-term, low birth weight infant, socioeconomic status, and access to medical care. The second reason is related to the increase in pre-term babies (37). Pre-term is an important cause of IMR. In 2005, 36.5% of infant deaths were caused by factors related with pre-term (38). Pre-term rate has gradually increased in the USA. From 2000 to 2007, pre-term babies less than 34 weeks increased from 3.4% to 3.6%, while pre-term babies of 34-36 weeks increased from 8.1% to 9.1% among total live births (39). In the same period, preterm babies of less than 34 weeks increased from 55.7% to 58.2%, while the pre-term babies of 34-36 weeks increased from 9.4% to 10.0% for IMR (39). The rates were different depending on each race. Whereas nearly half of infant deaths (46%) of non-Hispanic black women (37) are related with pre-term, only 32% are related to non-Hispanic white women (38). The third reason is related to change of maternal conditions, such as the increase in single mothers (37). The IMR of single mothers was rated 9.7% in 2007, which made it 78% higher than the IMR of married mothers (38). However, the birth rate of single mothers increased from 43.7 in 2002 to 52.9 in 2007, and the ratio of total childbirths increased from 39.7% in 2007 to 40.6% in 2008. In this aspect, the gradual increase of IMR can also be expected. The fourth reason was related to the difficulty in accessing health care due to high medical expenses (37). The medical expenses in the USA occupied 15.3% of total GDP (40). Although this was significantly higher than Korea (6.2%) and Japan (8.2%), the number of doctors and the average days of hospitalization were below the OECD average. In the medical system of the USA, approximately 14.3%-20.0% of the population is not registered in Medicare, Medicaid, or private insurance, consequently prevented from receiving medical insurance benefits (40, 41). In particular, 8.6% of children under the age of 18 are unable to receive medical insurance benefits (41). In addition, the infantile non-insurance ratio in the poverty class and the second highest class is measured to be far higher than the average, at 11.6% and 17.4%, respectively. Thus, such information is in sharp contrast to Korea or Japan, where almost all children receive medical benefits through the medical insurance and medical care system (41). To improve such pitfalls in the infantile medical system, Children's Health Insurance Program Re-authorization Act (CHIPRA) was enacted in 2009. This act expands the previously existing Children's Health Insurance Program (CHIP) or Medicaid to provide medical support to more children (42). However, as such efforts are being strongly resisted by parties of opposing states, it remains ambiguous whether or not such efforts will effectively reduce IMR in the USA.
The number of total annual live births in Korea has been: 715,020 in 1995, 634,501 in 2000, 435,031 in 2005, and 469,900 in 2010. The crude birth rate has been: 16 in 1995, 13.3 in 2000, 8.9 in 2005, and 9.4 in 2010. And total fertility rate has been: 1.63 in 1995, 1.47 in 2000, 1.08 in 2005, and 1.22 in 2010; indicating that we are in the era of a low birth rate (43). The total number of births has decreased, but the number of births of high-risk pre-term infants or low birth weight infants has been gradually increasing. In Korea, the birth incidence of low birth weight infants has been increasing from 3.0%, 3.7%, 4.2% to 4.9%, in 1995, 2000, 2005, and 2009, respectively. While the birth incidence of pre-term infants has also has been increasing from 2.5%, 3.8%, 4.7% to 5.7%, respectively (43, 44). According to the report of the KMHW in 2008, births by mothers with high-risk pregnancy accounted for 22% of the total births. Regarding the factor of high-risk mothers, the average age of mothers at birth has been increasing from 27.9 in 1995 to 31.0 in 2009. Particularly, the proportion of births by advanced maternal aged group beyond the age of 35 at birth has significantly increased as from 4.7% in 1995, 6.7% in 2000, 10.8% in 2005 to 15.3% in 2009 (44). Also, the multiple birth rates have been increasing as 13.2, 16.9, 21.7, and 27, in 1995, 2000, 2005, and 2009, respectively (45). In addition, the number of births from assisted reproductive technology, which is one of the major causes of multiple births, has been increasing since the second half of 1990's from 2,475 neonates in 1996, 2,232 in 2000 to a 3,255 in 2006. 53.2%, 47.1%, and 53.0% of the births from assisted reproductive technology were multiple births implying that approximately half of such births result in multiple births (46). Among births from assisted reproductive technology in 2006, 43.5% were by mothers of advanced age. This was a much greater percentage in comparison to the 11.8% of the total live births (46). The escalating number of teen-aged pregnancies is another reason for the increase in high risk pregnancies. The percentage of deliveries by women under the age of 20 has been increasing from a 4.2% in 1995, 5.3% in 2000, 3.9% in 2005, to a 5.5% in 2009 (43). According to a report from the Korean Women's Development Institute by Kim et al. (47), 40% of single mothers who had entered 43 of the nationwide adoption institutes in July-August of 2009 were teen-aged pregnancies. Among these single mothers, 40.6% were under 19, 31.8% in the age group of 20-24, 20.9% in the age group of 25-29, and 16.7% were over 30 yr of age. In consideration of these trends, KMHW has made efforts by supporting the registration of neonates born of pre-terms or with congenital anomalies along with medical expense support, holding campaigns for the nationwide installation of NICU, promoting improved health care for pregnant women and children, developing projects for improving the general health of women of childbearing age, and providing medical expense support for pregnancy and delivery of teen-aged pregnancies. Korea Ministry of Gender Equality and Family has aspired to establish and enhance the management systems for single mothers as well. With these accomplishments as a foundation, further nationwide support will be required. This along with upgraded management of the increasing number of pre-terms and low birth weight infants and management of high risk pregnancies will lead to improved NMR and IMR in Korea.
During the past 20 yr, NMR and IMR in Korea have been lowered remarkably from 6.6 and 9.9 in 1993 to 1.7 and 3.2 in 2009, respectively. These figures, though still higher than those of Japan, are quite impressive as they are lower than the mean values of OECD nations and the USA.
In the discussion above, various factors related to the health and medical care, service system of prinatology, neonates (especially pre-terms) and infants affecting the NMR and IMR in Korea, Japan, and in the USA, have been analyzed. The current status of such related factors were reviewed, showing the reasons for the developed status of Japan and the developmental delay of the USA. The establishment of perinatal care center systems and regionalization, along with a nationwide neonatal research system was suggested as aspects which should be introduced into the Korean system with Japan as its role model for further improvement in NMR and IMR. Significant gaps in the provision of adequate health care due to racial differences and high medical costs, increase in pre-term babies and teen-aged mothers, and increase in high-risk maternal factors such as advanced maternal aged-pregnancy were considered to be the mainstay of causes for the retention of high NMR and IMR in the USA. In contrast, Korea's strong points lie in that there is no significant racial discrimination among races, as well as a wide range of beneficiaries for medical care due to the national medical insurance system, although governmental support is yet in need for further development, with long-term measures for increased incidence of pre-term and low birth weight infant, and the number of high-risk pregnancies such as advanced maternal aged-pregnancy group, multiple births, teen-aged pregnancies, births conceived by assisted reproductive technology.
NMR and IMR, with their significant decrease in the past 60 yr of Korean history, have served as indicators for the extensive improvement of national healthcare. For further development in this area, persistent efforts are anticipated in the perinatal, neonatal and infantile health and medical care system.
In order to overcome the low birth rate facing Korean society, nationwide encouragement for childbirth while providing a better environment for raising our children healthily will be crucial. Improved child care is an investment in the future generation's human resources directly having impact on a nation's power and status. Caring for women throughout pregnancy and childbirth and managing the health of neonates, infants, and children are not only the responsibility of health care personnel and government agencies but also belongs to Korean society, as a whole.
Figures and Tables
Fig. 1
Estimates of Korean infant mortality rate reported by the United Nations (Sources: reference 5).

Fig. 3
The proportion of neonatal mortality rate in infant mortality rate in Korea from 1993 to 2009. Even though recently the ratio of neonatal mortality rate to infantile mortality rate shows decreasing tendency, it still occupies more than half of infantile mortality rate. *data from the Korea Ministry of Health and Welfare; †Data from Statistics Korea (Sources: reference 2-15).
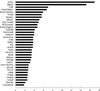
Fig. 4
The infant mortality rates of OECD nations in 2008. The mean infant mortality rate of Korea is 3.4 in comparison with 4.7 of OECD nations (Source: reference 18). *The USA in 2006; †Canada and Ireland in 2007.
ACKNOWLEDGMENTS
The authors would like to thank Young Ja Han, Ph.D. for her works on the Korean infant mortality survey of 1993, 1996, 1999, 2002, 2003, 2005, 2006 under the Korea Institute for Health and Social Affairs and for allowing us to incorporate the statistical results.
AUTHOR SUMMARY
Decreasing Trends of Neonatal and Infant Mortality Rates in Korea: Compared with Japan, USA, and OECD Nations
Ji-Young Chang, Kyung Suk Lee, Won-Ho Hahn, Sung-Hoon Chung, Yong-Sung Choi, Kye Shik Shim and Chong-Woo Bae
In this review, we investigated changes in neonatal and infant mortality rate (NMR, IMR) in Korea and compared the results with those of Japan, USA, and OECD nations. During the past 20 yr, NMR and IMR have lowered remarkably; the values in 2009 were lower than the average of OECD nations and USA, although higher than Japanese IMR. Several suggestions in perinatal, neonatal and infantile health care were elucidated to achieve further improvement on NMR and IMR in Korea.
References
1. Park CB, Park BT. Infant mortality rate: survey of recent fertility in Korea. 1981. Seoul: Korea Institute for Health and Social Affairs;11–25.
2. Han YJ, Doh SR, Seo K, Park JH, Lee SU. Infant mortality level and characteristics in 1996. 1998. Seoul: Korea Institute for Health and Social Affairs, Korea Ministry of Health and Welfare;62–64.
3. Korea Ministry of Health and Welfare. Infant mortality survey report in 1996. 1999. Seoul: Korea Ministry of Health and Welfare;31–33.
4. Han SH, Kim IS. Recent trends of infant death rates and its determinants in Korea. Korean J Epidemiol. 1990. 12:57–89.
5. UN, UN data, Infant mortality rate. accessed on 15 July 2011. Available at http://data.un.org/Data.aspx?q=infant+mortality&d=PopDiv&f=variableID%3a77.
6. Han YJ, Doh SR, Lee SU, Lee HB, Lee MI. Infant mortality survey report in 1993. 1997. Seoul: Korea Ministry of Health and Welfare, Korea Institute for Health and Social Affairs;59–60.
7. Han YJ, Doh SR, Lee SU, Lee HB, Lee MI. Infant mortality level and characteristics. 1996. Seoul: Korea Institute for Health and Social Affairs;70–74.
8. Han YJ, Lee SU, Chang YS, Kim DJ, Lee SU. Infant mortality level and characteristics of perinatal death in 1999. 2002. Seoul: Korea Institute for Health and Social Affairs;39–43.
9. Han YJ, Seo K, Lee SU, Lee SU, Shin CW. Infant and maternal death survey report in 2002-2003. 2005. Seoul: Korea Institute for Health and Social Affairs, Korea Ministry of Health and Welfare;67–70.
10. Han YJ, Choi JS, Seo K, Lee SU, Oh HC, Kim NO, Hong JS, Shin SM, Lee NH. Infant and maternal death survey report in 2005-2006. 2008. Seoul: Korea Institute for Health and Social Affairs, Korean Medical Record Association, Korea Ministry of Health and Welfare;77–92.
11. Korea Ministry of Health and Welfare. Infant mortality survey report in 1996. 1999. Seoul: Korea Ministry of Health and Welfare;33–37.
12. Korea Ministry of Health and Welfare. Infant mortality survey report in 1999. Korea Ministry of Health and Welfare 1999 (Infant mortality level and characteristics of perinatal death in 1999). 2002. Seoul: Korea Ministry of Health and Welfare;39–43.
13. Choi JS, Seo K, Lee NH, Lee SU, Shin CW, Bu YK. Infant and maternal death survey report in 2007-2008. 2010. Seoul: Korea Institute for Health and Social Affairs, Korean Medical Record Association, Korea Ministry of Health and Welfare;89–90.
14. Korea Ministry of Health and Welfare. Yearbook of heath, welfare and family statistics in 2007. 2007. Seoul: Korea Ministry of Health and Welfare;56.
15. Korea Ministry of Health and Welfare. Yearbook of heath, welfare and family statistics. 2009. Seoul: Korea Ministry of Health and Welfare in 2009;20.
16. Statistical report of causes of death in Korea in 2009. Statistics Korea. accessed on 15 July 2011. Available at http://kostat.go.kr/wnsearch/search.jsp.
17. Korea Ministry of Health and Welfare. OECD statistics in 2009. 2009. Seoul: Korea Ministry of Health and Welfare;96.
18. OECD Health Data 2010, Infant mortality. OECD. accessed on 15 July 2011. Available at http://www.oecd.org/document/0,3746,en_2649_201185_46462759_1_1_1_1,00.html and http://www.oecd.org/dataoecd/4/36/46796773.pdf.
19. Health statistics and health information systems, infant mortality. WHO. accessed on 15 July 2011. Available at http://www.who.int/healthinfo/morttables/en/index.html.
20. WHO mortality database, infant death. WHO. accessed on 15 July 2011. Available at http://apps.who.int/whosis/database/mort/table2.cfm.
21. Statistics, infant mortality rate. Japan Ministry of Health, Labour and Welfare. accessed on 15 July 2011. Available at http://www.mhlw.go.jp/english/database/db-hw/report/3.html.
22. United States infant mortality rate. Index Mundi. Index Mundi. accessed on 15 July 2011. Available at http://www.indexmundi.com/united_states/infant_mortality_rate.html.
23. Ministry of Health and Welfare. Health care and service for newborn, infant and mother: 2011. 2011. Seoul: Ministry of Health and Welfare;3–9.
24. Change of statistical method for infant and mother's death survey in Korea. Statistics Korea. accessed on 15 July 2011. Available at http://kostat.go.kr/wnsearch/search.jsp.
25. Hahn WH, Chang JY, Chang YS, Shim KS, Bae CW. Recent trends in neonatal mortality in very low birth weight Korean infants: in comparison with Japan and the USA. J Korean Med Sci. 2011. 26:467–473.
26. Hwang NM. Health care and service system for newborn and infant in other nations. Proceeding of the 57th annual spring meeting of the Korean pediatric Society. 2007. 19: 27.
27. Neonatal Research Network, Japan. accessed on 15 July 2011. Available at http://nrn.shiga-med.ac.jp/.
28. Perinatal Care Center Network, Japan. accessed on 15 July 2011. Available at http://plaza.umin.ac.jp/nrndata/syukei.htm.
29. Kusuda S, Fujimura M, Sakuma I, Aotani H, Kabe K, Itani Y, Ichiba H, Matsunami K, Nishida H. Morbidity and mortality of infants with very low birth weight in Japan: center variation. Pediatrics. 2006. 118:e1130–e1138.
30. Itabashi K, Horiuchi T, Kusuda S, Kabe K, Itani Y, Nakamura T, Fujimura M, Matsuo M. Mortality rates for extremely low birth weight infants born in Japan in 2005. Pediatrics. 2009. 123:445–450.
31. Bae CW. Bench-marking of Japanese perinatal center system for improving maternal and neonatal outcome in Korea. Korean J Perinatol. 2010. 21:129–139.
32. National Institute of Child Health and Human Development (NICHD) Neonatal Research Network. accessed on June 2011. Available at https://neonatal.rti.org/.
33. Vermont Oxford Network. accessed on June 2011. Available at http://www.vtoxford.org/.
34. Payne NR, Finkelstein MJ, Liu M, Kaempf JW, Sharek PJ, Olsen S. NICU practices and outcomes associated with 9 years of quality improvement collaboratives. Pediatrics. 2010. 125:437–446.
35. Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR, Bauer CR, Donovan EF, Korones SB, Laptook AR, Lemons JA, Oh W, Papile LA, Shankaran S, Stevenson DK, Tyson JE. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol. 2007. 196:147.
36. Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, Hale EC, Newman NS, Schibler K, Carlo WA, Kennedy KA, Poindexter BB, Finer NN, Ehrenkranz RA, Duara S, Sánchez PJ, O'Shea TM, Goldberg RN, Van Meurs KP, Faix RG, Phelps DL, Frantz ID 3rd, Watterberg KL, Saha S, Das A, Higgins RD. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010. 126:443–456.
37. Mathews TJ, Miniño AM, Osterman MJ, Strobino DM, Guyer B. Annual summary of vital statistics: 2008. Pediatrics. 2011. 127:146–157.
38. MacDorman MF, Mathews TJ. Recent trends in infant mortality in the United States. NCHS Data Brief. 2008. (9):1–8.
39. Mathews TJ, MacDorman MF. Division of Vital Statistics. Infant mortality statistics from the 2007 period linked birth/infant death data set. Natl Vital Stat Rep. 2011. 59:1–47.
40. Anderson GF, Squires DA. Measuring the U.S. health care system: a crossnational comparison. Issue Brief (Commonw Fund). 2010. 90:1–10.
41. Cohen RA, Martinez ME. Health insurance coverage: early release of estimates from the National Health Interview Survey. National Center for Health Statistics. accessed on 15 July 2011. Available at http://www.cdc.gov/nchs/nhis.htm.
42. The Children's Health Insurance Program (CHIP). Children's Health Insurance Program Reauthorization Act of 2009 (CHIPRA or Public Law 111-3). accessed on 15 July 2011. Available at https://www.cms.gov/chipra/.
43. Birth statistics in Korea in 2010. Statistics Korea. accessed on 15 July 2011. Available at http://kostat.go.kr/wnsearch/search.jsp.
44. Moon JY, Hahn WH, Shim KS, Chang JY, Bae CW. Changes of maternal age distribution in live births and incidence of low birth weight infants in advanced maternal age group in Korea. Korean J Perinatol. 2011. 22:30–36.
45. Choi SH, Park YS, Shim KS, Choi YS, Chang JY, Hahn WH, Bae CW. Recent trends in the incidence of multiple births and its consequences on perinatal problems in Korea. J Korean Med Sci. 2010. 25:1191–1196.
46. Park YS, Choi SH, Shim KS, Chang JY, Hahn WH, Choi YS, Bae CW. Multiple births conceived by assisted reproductive technology in Korea. Korean J Pediatr. 2010. 53:880–885.
47. Kim HY, Sun BY, Kim EY, Jung JH. Unwed mother's life world and policy agenda. 2009. Korean Women's Development Institute;39–40.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download