Abstract
The purpose of this study was to evaluate the associations between weight status and mental disorders, including depressive disorder, anxiety disorder and alcohol use disorder. A total of nationally representative 6,510 subjects aged 18-64 yr was interviewed in face-to-face household survey. Response rate was 81.7%. Mental disorders were diagnosed using the Korean version of the Composite International Diagnostic Interview (K-CIDI). The subjects reported their heights and weights. After adjusting for age and gender, the lifetime diagnosis of depressive disorder had a significant association with only the underweight group (odds ratio [OR], 1.68, 95% confidence interval [CI], 1.19-2.38). The association between underweight and depressive disorder was the strongest for subjects with a high education level (OR, 1.75, 95% CI, 1.2-2.56), subjects with a married/cohabiting status (OR, 1.94, 95% CI, 1.17-3.22) and smokers (OR, 2.58, 95% CI, 1.33-4.98). There was no significant association between obesity and depressive disorder in Korea. But there was a significant association between the underweight group and depressive disorder. The relationship between obesity and mental disorder in a Korean population was different from that in a Western population. These results suggest that the differences of traditional cultures and races might have an important effect on the associations between the weight status and mental disorders.
The prevalence of obesity among Koreans older than 20 yr of age was 26.3% (25.7% in male, 26.4% in female) in 1998 and rapidly increased to 31.8% (35.2% in male, 28.3% in female) in 2005. The increasing trend was prominent in male (1). The prevalence of obesity has rapidly increased globally and obesity is related with serious public health problems. However, the relationships between mental disorders and obesity remain controversial. Crisp et al. proposed a "jolly fat" theory in which depression and anxiety were decreased in obese middle-aged men (2, 3). However, a prospective study on middle-aged adults in the USA found that the risk of developing depression one-year later was two-times higher for the obese group than for the control group (4). Simon et al. (5) performed a cross-sectional study using NCS-R data to investigate the relationship between obesity and psychiatric disorders. They found a significant increase of the lifetime diagnoses of mood disorders and anxiety disorders in the obese group (body mass index [BMI] ≥ 30 kg/m2) but there was a significant decrease of the lifetime diagnosis of substance use disorder in the obese group. The association between obesity and mood disorder was strongest for non-Hispanic whites and college graduates. In one of the larger studies, the New Zealand Mental Health Survey (NZMHS), obesity was significantly associated with any mood disorder, major depressive disorder and any anxiety disorder, and obesity had the strongest association with post-traumatic stress disorder (PTSD) (6). Most of the data on obesity and its association with mental disorders has come from Western adult populations and only two Asian studies on China and Japan elderly population have been reported (7, 8). The data on Chinese elderly people supports the "jolly fat" hypothesis and it extends the hypothesis to both male and female elderly (7). Chinese traditional culture and the positive value of an obese body image may have affected the results of the above mentioned study. A cross-sectional study on Japanese elderly was done with examining the relationship between obesity and depression (8). No relationship between obesity and depression was shown for elderly men and healthy elderly women, but an inverse linear trend was observed for elderly women with chronic diseases. Thus, this "jolly fat" theory was supported for Japanese elderly women with chronic diseases. However, there has been no adult study on this for a general Asian population.
We hypothesize that the relationship between obesity and mental disorder in an Asian population may be different from that in a Western population due to the differences of traditional cultures, genetic and socioeconomic factors. In 2006 and 2007, the Korean Epidemiological Catchment Area (KECA) study, a nationwide cross-sectional survey in community sample of Korean adults aged 18-64 yr, was conducted to estimate the prevalence and clinical correlations of the psychiatric disorders and weight status (9). This study assessed the relationships between weight status and mental disorders, including depressive disorder, anxiety disorder and alcohol use disorder.
The KECA study was conducted in twelve different regions of Korea from July 2006 to April 2007 (9). The population sample was selected using a stratified, multi-stage cluster sampling method, which was based on the 2005 Population Census Data at the National Statistical Office of the Republic of Korea Government. One subject per selected household was chosen by identifying the individual with the earliest birthday without consideration of month or year. From an initially selected 7,968 persons, a total of 6,510 subjects, aged between 18 and 64 yr, were face-to-face interviewed; the response rate was 81.7%. Of 6,510 participants, 6,441 reported their weights and heights. The heights and weights were self-reported.
The psychiatric disorders were assessed using the K-CIDI version (10). The fully structured diagnostic interview was designed to make psychiatric diagnoses with using the criteria of the DSM-IV. The K-CIDI was validated by Cho et al. (10), according to the World Health Organization guidelines (11, 12), and previously used in a KECA study (13).
The K-CIDI and the included questionnaire assessed the following: demographics, depressive disorders (major depressive disorder, dysthymia), anxiety disorders (panic disorder, agoraphobia, specific phobia, PTSD, Obscessive-compulsive disorders [OCD]) and alcohol use disorder (alcohol abuse, alcohol dependence). Trained interviewers assessed the lifetime diagnoses of these disorders.
BMI was calculated from subject's self-reported weight and height. Each subject was classified into three groups; underweight (< 18.5 kg/m2), normal or overweight (18.5 kg/m2-24.9 kg/m2) and obese (≥ 25 kg/m2).
Statistical analysis was performed using SPSS, version 12.0. Statistical significance was determined at an alpha level < 0.05. Logistic regression models were used to calculate the odds ratios (ORs) and 95% confidence intervals of the relationship between weight status and the lifetime prevalence of depression disorder, anxiety disorder and alcohol disorder with adjusting for age, gender, the education level, the marital status and tobacco use. The subjects were classified into three BMI groups, with the normal or overweight group treated as the reference group. Between-group demographic characteristics were tested using the chi-square test.
All the analyses were based on weighted data for sex and age in order to approximate the national population in terms of sex and age as defined by the 2005 census of the Korean National Statistical Office. It was difficult to observe a tendency of continuous change in the three BMI group. Thus, BMIs was categorized into seven groups (BMI: 15-16.9, 17-18.49, 18.5-19.9, 20-24.9, 25-29.9, 30-34.9, 35-39.9 kg/m2) and the lifetime prevalence of mental disorders was shown in relation to the BMIs in a graph (Fig. 1).
Table 1 shows the demographic characteristics according to the BMI groups. Obesity prevalence was 27.5% among males and 14.7% among females. The proportion of people with an old age and a low education level was higher in the obese group than that in the underweight group. There were no severely obese subjects with a BMI ≥ 40 kg/m2.
Table 2 shows the lifetime prevalences of mental disorders among the three main BMI groups.
Obesity was significantly associated with panic or agoraphobia (OR, 2.58; 95% confidence interval [CI], 1.48-4.5) and alcohol use disorder (OR, 1.29; 95% CI, 1.1-1.5). Underweight was significantly associated with depressive disorder (OR, 2.07; 95% CI, 1.45-2.81), anxiety disorder (OR, 1.66; 95% CI, 1.18-2.35) and alcohol use disorder (OR, 0.60; 95% CI, 0.43-0.83). There was a strong relationship between being underweight and OCD (OR, 3.36; 95% CI, 1.44-7.86), but there was also a significant relationship between underweight and major depression (OR, 2.12; 95% CI, 1.51-2.98).
The prevalence of mental disorders in the seven BMI groups revealed a negative linear trend between BMI and depressive and anxiety disorders. However, there was a positive linear trend between BMI and alcohol use disorder (Fig. 1).
The lifetime prevalence of depressive disorder among the BMI groups was stratified by the sociodemographic groups (Table 3). The association between obesity and depressive disorder was significantly low for men (P < 0.05). Underweight was significantly associated with the 30-39 and 50-64 yr age groups, a high education level, people who were married or had a cohabiting status, and people with an unmarried status.
The parallel subgroup analyses for anxiety disorders showed significant associations between obesity and the younger age group and an unmarried status (Table 4). Underweight was significantly associated with the older age group, the male gender and smokers.
The lifetime prevalence of alcohol use disorder among the BMI groups was stratified by the sociodemographic groups (Table 5). The association between alcohol use disorder and obesity was statistically significant for the people who were 18-29 yr of age. This association did not significantly differ according to gender. Underweight was negatively associated with the younger age group (18-29 yr) with statistical significance (OR, 0.55; 95% CI, 0.34-0.91). This positive linear trend for alcohol use disorder among the BMI groups is opposite the tendency for depressive disorder and anxiety disorder.
Several potential covariates might amplify or obscure the relationship between obesity and mental disorders. Those confounding factors (age, gender, martial status, education level and smoking status) were adjusted (Table 6). Before adjustment, underweight was positively associated with depressive disorder (OR, 2.07; 95% CI, 1.43-2.78) and anxiety disorder (OR, 1.66; 95% CI, 1.19-2.36) and it was negatively associated with alcohol use disorder (OR, 0.60; 95% CI, 0.42-0.82). Obesity was positively associated with alcohol disorder (OR, 1.29; 95% CI, 1.11-1.50).
Adjustment for age and gender did not significantly affect the association between underweight and depressive disorder (OR, 1.68; 95% CI, 1.19-2.38), but adjustment for age and gender rendered the association between the BMI groups and either anxiety or alcohol use disorder insignificant. Adjustment for the smoking status, marital status, the education level and comorbid psychiatric disorder had no significant effect on the observed associations.
We observed a significant association between underweight and depressive disorder. We also found a negative linear trend between BMI and depressive disorder. This trend was strong in men and it may support the "jolly fat" hypothesis. This result was consistent with the data on Chinese elderly people. Obese Chinese elderly people were less likely to suffer from depressive symptoms than the normal weight population (7). Another Asian study in Japanese elderly reported that an inverse trend between BMI and depressive disorder was observed only for women with chronic medical conditions (8).
The previous western studies have reported inconsistent results about the relationship between obesity and depression. Scott et al. (6) examined the association between mental disorders and obesity in New Zealand. In contrast to our study, the New Zealand study showed significantly positive association between obesity and major depressive disorder and anxiety disorder, with the strongest association shown for people with PTSD.
Simon et al. (5) used data from the national comorbidity survey replication (NCS-R) to evaluate the relationship between obesity and depression. Contrary to our study, obesity was significantly positively associated with mood disorder and anxiety disorder, but obesity was negatively associated with substance use disorder. The association between obesity and mood disorders was the strongest for young respondents, college graduates and non-Hispanic whites. However, our study found no relationship between obesity and depressive disorder and there was a lower prevalence of depression for obese men. No significant association was shown between obesity and anxiety disorder. These differences maybe originated from different traditional cultures, values and races. Subjects with severe obesity (BMI ≥ 40 kg/m2) are not common in the Asian population. Actually, our study has no severely obese subjects. In our study, only 2.1% of the male adults and 1.5% of the female adults had a BMI of 30 kg/m2 or over, but 2.1% of the male adults and 10.4% of the female adults had a BMI < 18.5 kg/m2. Thus, the association between mental disorder and the underweight group was prominent. Depression can also decrease appetite, resulting in weight loss. Asian populations have a lesser degree of obesity than do western populations, and there is less concern about weight gain and diet. In our study, Korean obese men showed a more stable marital status, a more smoking status and a lower prevalence of depressive disorder than did the normal weight men. Wealthy and successful Korean men tend to enjoy the workplace culture, and they go out to dine and drink alcohol with their companions. Being fat does not mean being unhappy in different countries (7). Crandall et al. (16) examined the attitudes toward obesity in six countries. The more negative attitudes toward obesity were shown in Australia, Poland and the USA, where individualism is prevalent as compared to India, Turkey and Venezuela, where collectivism dominates. The obese people experience a loss of self-esteem, social disadvantages and depression in individualistic countries. Collectivism dominates in Korean traditional culture, but individualism has recently spread rapidly among the young people. Many Korean young subjects have a western body weight norm and values and they feel pressure to diet. Our data found that younger obese women showed more of a depressive tendency than did the older obese men, although this was not significant. The "jolly fat" theory is not acceptable to young Korean women who are sensitive to social prejudice about body weight. Women repeatedly experience shame and helplessness whenever they gain weight after losing weight through a severe diet, and they "binge eat" to escape negative feelings and their diet (17). Mood disorder has been reported in 60% of bulimic patients (18).
On the other hand, our study showed a higher lifetime prevalence of panic disorder or agoraphobia in the obese group before adjusting for age and gender. Because of the low prevalence of panic disorder or agoraphobia (1.6%), it is not useful to compare our data to the previously reported data from other countries. Anxiety disorder is a heterogenous disease so that it shows a complex relationship with BMI.
Scott et al. (6) reported a high one-year prevalence of depressive disorder, anxiety disorder and especially PTSD in the obese group. The national epidemiologic survey on alcohol and related conditions (NESARC) in the USA found a significantly high prevalence of panic disorder in overweight men and a high prevalence of specific phobias in overweight and obese women (19). Some patients with anxiety disorder experienced obesity due to emotional eating which was related with binge eating. When the binge eating was not followed by compensatory behaviors, it was significantly related with obesity (20). Anxiety is a negative feeling that increases food intake in obese individuals as compared to that of the normal weight group (21). Anxiety disorder is not accompanied by a decreased appetite, which is seen in depression. Anxiety disorder is also reported in patients with eating disorder in many cases (6, 22). Panic disorder and being overweight share some symptoms; obesity is highly related with cardiovascular disease and diabetes mellitus type 2. Cardiovascular disease and diabetes mellitus type 2 may induces panic like symptoms. Panic disorder was diagnosed more in adult males, suggesting the possibility of panic disorder coexisting with undiagnosed cardiovascular disease or diabetes mellitus type 2 (19).
In contrast to the previously reported western data, a positive linear trend was observed between BMI and alcohol use disorder. Several community surveys in the United States and Germany have reported significantly low levels of a lifetime diagnosis of substance use disorder in the obese group (5, 23). However, a prospective study in Britain with 5 yr of follow-up found that heavy alcohol intake contributes to obesity (24).
Alcohol and food consumption may be similar behaviors for dealing with stress and for temporarily relieving anxiety (23). Alcohol drinking may lead to weight gain due to the high calorie intake. Acetate is a metabolite of ethanol, and acetate inhibits lipolysis in peripheral tissues and it suppresses whole-body lipid oxidation (24). However, alcohol drinking also may induce weight loss because of anorexia and gastrointestinal disorder.
Korean obese men showed a more stable marital status, a higher education level and a higher prevalence of alcohol use disorder than did the normal weight men. In our study, the lifetime prevalence of alcohol use disorder was 20% in the obese group and 16.3% in the normal BMI group. Our data showed a prominently higher prevalence of alcohol use disorder in Korea than that in the Western countries (25). The lifetime prevalence of alcohol use disorder decreased from 22.0% in 1984 to 17.2% in 2001 in South Korea (13); which, it is still the highest among the Asian and Western countries (26).
In Korean traditional culture, it is permissive to drink alcohol in social settings. Workers frequently attend workplace outings, and especially when there is pressure from management to attend. For our subjects, 26.3% of the males and 6.9% of the females showed alcohol use disorder. Working men have many more opportunities to social alcohol drink than do homemakers. The wealthier and more sociable peoples often enjoy alcohol drinking and this is not recognized as problem drinking. The diagnostic interview criteria of the CIDI for an alcohol problem are strict for traditional Korean culture.
Our study had several limitations. First, the body weights and heights were self-reported by the interviewees so that the calculated BMIs may have been more inaccurate than objective measurement. However, previous research suggests that self-reported height and weight are highly correlated with objective measurements, but some obese persons tend to underreport weight and overreport height (27). Many papers about relationships between obesity and psychiatric disorders used self-statements of body weight and height (5, 6, 23). Second, this cross-sectional design was effective in determining the coexistence of obesity and mental disorder, but the causal relationship for whether obesity affects the development of mental disorder could not be inferred. Third, we did not evaluate the effects of medications, although the relationship between psychotropic drugs and obesity is well pronounced. Fourth, we classified obesity as BMI ≥ 25 kg/m2 by the recommendation of the Steering Committee of the Western Pacific Region of WHO (28). If we accept the Western criteria of BMI ≥ 30 kg/m2, the prevalence of obesity is less than 5% in Japan and Korea, in contrast to the 20-30% in United States and United Kingdom (29). In our study, the percentage of population with BMI ≥ 30 kg/m2 is only 2.1% of male and 1.5% of female adults, so we needed the adjustment of the Western criteria. In Japanese-American's study, BMI ≥ 25 kg/m2 is practical criteria for identifying diabetes risk (30). In the groups of BMI ≥ 30 kg/m2, the lifetime prevalence of panic or agoraphobia and alcohol use disorder was significantly increased than normal weight population. However, those associations were not observed after adjustment for age, gender and smoking.
Our study had a lot of strong points. First, it was large-scale nationally representative face-to-face household survey and the sample was selected to accurately represent the general population of the twelve different regions of Korea. Second, we assessed psychiatric disorders using the K-CIDI and a fully structured diagnostic interview, which have high validity and reliability. The CIDI has frequently been used in previous Western studies, so our data is useful to compare with Western data.
In conclusion, no significant association between obesity and depressive disorder was observed in the Korean adult population. Yet there was a significant association between the underweight group and depressive disorder. These results suggest that differences of traditional cultures and races might have an important effect on the associations between the body weight and mental disorders.
Figures and Tables
Fig. 1
Prevalence of lifetime mental disorders (depressive disorder, anxiety disorder, alcohol use disorder) in the multiple BMI groups.

Table 1
Demographic characteristics of the study sample and by the BMI* groups (the weighted proportions)

Table 3
Lifetime prevalence of depressive disorder by the BMI and as stratified by age, gender, the education level and the marital status

Table 4
Lifetime prevalence of anxiety disorder by BMI and as stratified by age, gender, years of education and the marital status

Table 5
Lifetime prevalence of alcohol use disorder by BMI and as stratified by age, gender, the years of education years and the marital status

Table 6
Adjusted ORs (with 95% CIs) of mental disorders‡ among those subjects with a BMI ≥ 25 and < 18.5 (relative to those with a BMI 18.5-24.9)
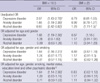
*P < 0.001; †P < 0.05; ‡Lifetime prevalence of depressive disorder, anxiety disorder and alcohol use disorder; §The OR for depressive disorders was adjusted for anxiety and alcohol use disorders. The OR for anxiety disorders was adjusted for depressive and alcohol use disorders, and the OR for alcohol use disorders was adjusted for depressive and anxiety disorders. BMI, body mss index.
ACKNOWLEDGMENT
The authors are grateful to all the interviewers and the Korean Ministry of Health and Welfare for their cooperation and assistance. The Korean Ministry of Health and Welfare had no additional role in study design, in the collection and analysis of data and in the writing of the paper.
AUTHOR SUMMARY
Relationships of Mental Disorders and Weight Status in the Korean Adult Population
Young-Kyung Sunwoo, Jae Nam Bae, Bong-Jin Hahm, Dong-Woo Lee, Jong-Ik Park, Seong-Jin Cho, Jun-Young Lee, Jin-Yeong Kim, Sung Man Chang, Hong Jin Jeon, and Maeng Je Cho
The purpose of this study was to evaluate the associations between weight status and mental disorders, including depressive disorder, anxiety disorder and alcohol use disorder. A total of nationally representative 6,510 subjects aged 18-64 yr was interviewed in face-to-face household survey. Response rate was 81.7%. Mental disorders were diagnosed using the Korean version of the Composite International Diagnostic Interview (K-CIDI). The subjects reported their heights and weights. The lifetime diagnosis of depressive disorder had a significant association with only the underweight group (odds ratio [OR], 1.68, 95% CI, 1.19-2.38). The association between underweight and depressive disorder was the strongest for subjects with a high education level (OR, 1.75, 95% CI, 1.2-2.56), subjects with a married/cohabiting status (OR, 1.94, 95% CI, 1.17-3.22) and smokers (OR, 2.58, 95% CI, 1.33-4.98). The relationship between obesity and mental disorder in a Korean population was different from that in a Western population. These results suggest that the differences of traditional cultures and races might have an important effect on the associations between the weight status and mental disorders.
References
1. Korean Ministry of Health and Welfare. Korean health and nutrition examination survey. 2005. Seoul: 38–39.
2. Crisp AH, McGuiness B. Jolly fat: relation between obesity and psychoneurosis in general population. Br Med J. 1976. 1:7–9.
3. Palinkas LA, Wingard DL, Barrett-Connor E. Depressive symptoms in overweight and obese older adults: a test of the "jolly fat" hypothesis. J Psychosom Res. 1996. 40:59–66.
4. Roberts RE, Kaplan GA, Shema SJ, Strawbridge WJ. Are the obese at greater risk for depression? Am J Epidemiol. 2000. 152:163–170.
5. Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, Kessler RC. Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry. 2006. 63:824–830.
6. Scott KM, McGee MA, Wells JE, Oakley Browne MA. Obesity and mental disorders in the adult general population. J Psychosom Res. 2008. 64:97–105.
7. Li ZB, Ho SY, Chan WM, Ho KS, Li MP, Leung GM, Lam TH. Obesity and depressive symptoms in Chinese elderly. Int J Geriatr Psychiatry. 2004. 19:68–74.
8. Kuriyama S, Koizumi Y, Matsuda-Ohmori K, Seki T, Shimazu T, Hozawa A, Awata S, Tsuji I. Obesity and depressive symptoms in elderly Japanese: the Tsurugaya project. J Psychosom Res. 2006. 60:229–235.
9. Korean Ministry of Health and Welfare. The Epidemiological survey of psychiatric illnesses in Korea. 2006. Seoul: 27–31.
10. Cho MJ, Hahm BJ, Suh DW, Hong JP, Bae JN, Kim JK, Lee DW, Cho SJ. Development of a Korean version of the Composite International Diagnostic Interview (K-CIDI). J Korean Neuropsychiatr Assoc. 2002. 41:123–137.
11. World Health Organization. CIDI, Core version 2.1 Trainer's manual. 1997. Geneva: World Health Organization;1–244.
12. World Health Organization. The world health report 2002: reducing risks, promoting healthy life. 2002. Geneva: World Health Organization;59.
13. Cho MJ, Kim JK, Jeon HJ, Suh T, Chung IW, Hong JP, Bae JN, Lee DW, Park JI, Cho SJ, Lee CK, Hahm BJ. Lifetime and 12-month prevalence of DSM-IV psychiatric disorders among Korean adults. J Nerv Ment Dis. 2007. 195:203–210.
14. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004. 363:157–163.
15. Korean society for the study of obesity. Clinical obesity. 2008. Seoul: Korean medical book publisher;179–180.
16. Crandall CS, D'Anello S, Sakalli N, Lazarus E, Wieczorkowska G, Feather NT. An attribution-value model prejudice: anti-fat attitudes in six nations. Pers Soc Psychol Bull. 2001. 27:30–37.
17. Foster GD, Wadden TA. Blackburn GL, Kander BS, editors. The psychology of obesity, weight loss, and weight regain: research and clinical findings. Obesity: psychophysiology, psychology, and treatment. 1994. New York: Chapman & Hall;140–166.
18. Mussell MP, Mitchell JE, Weller CL, Raymond NC, Crow SJ, Crosby RD. Onset of binge eating, dieting, obesity, and mood disorder among subjects seeking treatment for binge eating disorder. Int J Eat Disord. 1995. 17:395–401.
19. Pickering RP, Grant BF, Chou SP, Compton WM. Are overweight, obesity, and extreme obesity associated with psychopathology? Results form the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2007. 68:998–1009.
20. Yanovski SZ. Binge eating disorder and obesity in 2003: could treating an eating disorder have a positive effect on the obesity epidemic? Int J Eat Disord. 2003. 34:Suppl. S117–S120.
21. Ganley RM. Emotion and eating in obesity: a review of the literature. Int J Eat Disord. 1989. 8:343–361.
22. Godart NT, Flament MF, Perdereau F, Jeammet P. Comorbidity between eating disorders and anxiety disorders: a review. Int J Eat Disord. 2002. 32:253–270.
23. John U, Meyer C, Rumpf HJ, Hapke U. Relationships of psychiatric disorders with overweight and obesity in an adult general population. Obes Res. 2005. 13:101–109.
24. Wannamethee SG, Shaper AG. Alcohol, body weight, and weight gain in middle-aged men. Am J Clin Nutr. 2003. 77:1312–1317.
25. Helzer JE, Canino GJ, Yeh EK, Bland RC, Lee CK, Hwu HG. Alcoholism--North America and Asia. A comparison of population surveys with the Diagnostic Interview Schedule. Arch Gen Psychiatry. 1990. 47:313–319.
26. Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, Angermeyer MC, Bernert S, de Girolamo G, Morosini P, Polidori G, Kikkawa T, Kawakami N, Ono Y, Takeshima T, Uda H, Karam EG, Fayyad JA, Karam AN, Mneimneh ZN, Medina-Mora ME, Borges G, Lara C, de Graaf R, Ormel J, Gureje O, Shen Y, Huang Y, Zhang M, Alonso J, Haro JM, Vilagut G, Bromet EJ, Gluzman S, Webb C, Kessler RC, Merikangas KR, Anthony JC, Von Korff MR, Wang PS, Brugha TS, Aguilar-Gaxiola S, Lee S, Heeringa S, Pennell BE, Zaslavsky AM, Ustun TB, Chatterji S. WHO World Mental Health Survey Consortium. Prevalence, severity and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004. 291:2581–2590.
27. Kuczmarski MF, Kuczmarski RJ, Najjar M. Effect of age on validity of self-reported height, weight, and body mass index: findings from the Third National Health and Nutrition Examination Survey. 1988-1994. J Am Diet Assoc. 2001. 101:28–34.
28. Steering Committee of the Western Pacific Region of the World Health Organization. The International Association for the Study of Obesity, and the International Obesity Task Force. The Asia-Pacific perspective: redefining obesity and its treatment. 2000. Melbourne, Australia: Health Communications Australia Pty Ltd;18.
29. Kanazawa M, Yoshiike N, Osaka T, Numba Y, Zimmet P, Inoue S. Criteria and classification of obesity in Japan and Asia-Oceania. Asia Pac J Clin Nutr. 2002. 11:Suppl 8. S732–S737.
30. McNeely MJ, Boyko EJ, Shofer JB, Newell-Morris L, Leonetti DL, Fujimoto WY. Standard definition of overweight and central adiposity for determining diabetes risk in Japanese Americans. Am J Clin Nutr. 2001. 74:101–107.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download