Abstract
The aim of this study was to evaluate the relationship between coronary artery calcium score (CACS) assessed by multidetector computed tomography (MDCT) and plaque components assessed by virtual histology-intravascular ultrasound (VH-IVUS) in 172 coronary artery disease (CAD) patients with 250 coronary lesions. CACS was assessed according to Agatston scoring method by MDCT and patients were divided into four groups: Group I (CACS = 0 [n = 52]); Group II (CACS = 1-100 [n = 99]); Group III (CACS = 101-400 [n = 84]); and Group IV (CACS > 400 [n = 15]). Total atheroma volume was greatest in Group IV (152 ± 132 µL vs 171 ± 114 µL vs 195 ± 149 µL vs 321±182 µL, P < 0.001). The absolute dense calcium (DC) and necrotic core (NC) volumes were greatest, and relative DC volume was greatest in Group IV (5.5 ± 6.6 µL vs 11.0 ± 10.3 µL vs 15.6 ± 13.6 µL vs 36.6 ± 18.2 µL, P < 0.001, and 14.8 ± 18.2 µL vs 19.5 ± 18.9 µL vs 22.5 ± 19.1 µL vs 41.7 ± 27.9 µL, P < 0.001, and 6.4 ± 5.3% vs 11.0 ± 6.2% vs 14.0 ± 6.5% vs 20.0 ± 7.8%, P < 0.001, respectively). The absolute plaque and DC and NC volumes and the relative DC volume correlated positively with calcium score. CAD patients with high calcium score have more vulnerable plaque components (greater DC and NC-containing plaques) than those with low calcium score.
Coronary artery calcium is correlated closely with atherosclerotic plaque formation and has recently been developed as a marker of coronary atherosclerosis (1, 2). Also coronary calcium score can predict total mortality and degree of coronary artery disease risk according to Framingham criteria (3). Several studies have demonstrated a relation between the degree of coronary artery calcium and the severity of atherosclerosis and clinical events (4-8), and have shown that coronary artery calcium score (CACS) was associated with plaque burden and morphology (9-11). However, sparse data are available about the relation between CACS and plaque components.
Therefore, the aim of the present study was to evaluate the relation between CACS assessed by multidetector computed tomography (MDCT) and plaque components assessed by virtual histology-intravascular ultrasound (VH-IVUS) in patients with coronary artery disease (CAD).
This study was a retrospective, single-center study. From January 2007 to November 2009, a total of 172 CAD patients with 250 coronary lesions who underwent MDCT and VH-IVUS at Chonnam National University Hospital were enrolled in this study.
The blood samples were centrifuged, and serum was collected and stored at -70℃ until the assay was performed. Absolute creatine kinase-myocardial band levels were determined by radioimmunoassay (Dade Behring Inc., Miami, FL, USA). Cardiac-specific troponin I levels were measured by a paramagnetic particle, chemiluminescent immunoenzymatic assay (Beckman, Coulter Inc., Fullerton, CA, USA). The serum levels of total cholesterol, triglyceride, low-density lipoprotein cholesterol, and high-density lipoprotein cholesterol were measured by standard enzymatic methods. High-sensitivity C-reactive protein was analyzed turbidimetrically with sheep antibodies against human C-reactive protein; this has been validated against the Dade-Behring method (12).
Coronary angiogram was analyzed with validated QCA system (Phillips H5000 or Allura DCI program, Philips Medical Systems, Eindhoven, the Netherlands) (13). With the outer diameter of the contrast-filled catheter as the calibration standard, the minimal lumen diameter and reference diameter were measured in diastolic frames from orthogonal projections.
In the absence of contraindications (contraindication to intravenous contrast agents [contrast allergy] or elevated serum creatinine [> 1.3 mg/dL] or atrial fibrillation or frequent ventricular ectopy [> 10 extra systoles per minute], or a heart rate > 90 beats per minute), all patients with a resting heart rate of > 70 bpm received 50-100 mg of metoprolol orally 1-2 hr before scan. Blood pressure and pulse were rechecked immediately prior to performing the prodedure. CT examinations were performed with a two-phase, contrast-enhanced, electrocardiogram-gated, MDCT scanner (Sensation Cardiac 64, Siemens, Forcheim, Germany) set at a 0.75-mm section thickness with a gantry rotation time of 330 msec and a kernel value of B25f. The scan delay was determined using the bolus tracking technique: when a threshold of 120 Hounsfield Units (HU) was reached in the ascending aorta at the level of origin of the coronary arteries, a delay of 5 seconds was applied before the scan was initiated.
CACS were determined on a workstation (CaScore, Siemens, Germany) with software for coronary artery calcification according to the Agatston method as previously described (14). We classified the CACS as follows: Group I (calcium score = 0), Group II (calcium score = 1-100), Group III (calcium score = 101-400), Group IV (calcium score > 400) (Fig. 1A).
All pre-intervention grey-scale and VH-IVUS examinations were performed after intracoronary administration of 300 µg nitroglycerin. A 20-MHz, 2.9F IVUS imaging catheter (Eagle Eye, Volcano Corp, Rancho Cordova, CA, USA) was advanced > 10 mm beyond the lesion; and automated pullback was performed to a point > 10 mm proximal to the lesion at a speed of 0.5 mm/sec.
Grey-scale IVUS and VH-IVUS data were analyzed by 2 independent observers. The levels of reproducibility for external elastic membrane, lumen, and plaque plus media cross-sectional areas using the Spearman rank-order correlation coefficients were 0.95, 0.97, and 0.97, respectively. Similarly, for plaque components by VH-IVUS, reproducibility for the fibrous, fibro-fatty, dense calcium, and necrotic core volume measurements using the Spearman rank-order correlation coefficients were 0.95, 0.92, 0.93, and 0.93, respectively.
Quantitative volumetric grey-scale and VH-IVUS analyses were performed across the entire lesion segment, and cross-sectional analysis was performed at the minimum lumen area sites and at the largest necrotic core sites. Conventional quantitative volumetric grey-scale IVUS analysis was performed according to the American College of Cardiology Clinical Expert Consensus Document on Standards for Acquisition, Measurement and Reporting of Intravascular Ultrasound Studies (15). Measurements were made by every 1-mm interval for the region of interest, which was defined as the segment between distal to proximal reference sites that were the most normal looking within 5 mm proximal and distal to the lesion. Volumetric data were generated by the software using Simpson's method. External elastic membrane and lumen cross-sectional areas were measured. Plaque plus media cross-sectional area was calculated as external elastic membrane minus lumen cross-sectional area; and plaque burden was calculated as plaque plus media divided by external elastic membrane cross-sectional area. Total atheroma volume was calculated by summation of atheroma area from each measured image as: TAV = Σ (external elastic membrane area-lumen area). The percent atheroma volume was determined using the formula: PAV = 100 × (Σ [external elastic membrane area-lumen area]/Σ [external elastic membrane area]). VH-IVUS analysis classified the color-coded tissue into four major components: green (fibrous), yellow-green (fibro-fatty), white (dense calcium), and red (necrotic core) (16). VH-IVUS analysis was reported in absolute amounts and as a percentage of plaque area or volume (Fig. 1B). Thin-cap fibroatheroma was defined as a necrotic core ≥ 10% of plaque area in at least 3 consecutive frames without overlying fibrous tissue in the presence of ≥ 40% least 3 plaque burden.
The statistical package for social sciences (SPSS) for Windows, version 15.0 (Chicago, IL, USA) was used for all analyses. Continuous variables were presented as the mean value ± SD; comparisons were conducted by ANOVA. Discrete variables were presented as percentages and frequencies; comparisons were conducted by chi-square test, where appropriate. Pearson's correlation was used to evaluate the correlation between VH-IVUS parameters and CACS. A P value < 0.05 was considered statistically significant.
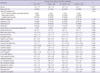
The baseline characteristics are summarized in Table 1. Group IV was oldest, and hypertension was observed most frequently in Group IV. The neutrophil count and hemoglobin level were lowest in Group IV. The high-density lipoprotein-cholesterol level was lowest in Group IV.
Coronary angiographic findings are summarized in Table 2. There were no significant differences in the target vessel, lesion location, and QCA data among four groups.
Grey-scale IVUS findings are summarized in Table 3. At the proximal reference, plaque burden was greatest in Group IV. At the distal reference, lumen cross-sectional area was smallest and plaque burden was greatest in Group IV. At the minimum lumen site, lumen cross-sectional area was smallest and plaque burden was tended to be greatest, and IVUS lesion was longest in Group IV. At the largest necrotic core site, plaque plus media cross-sectional area was greatest in Group IV. The calcium arc was greatest and calcium length was longest in Group IV and most of the calcium was observed at superficial location in Group IV. By volumetric analysis, external elastic membrane volume and total atheroma volume and percent atheroma volume were greatest in Group IV.
VH-IVUS findings are summarized in Table 4. At the proximal reference, absolute dense calcium and necrotic core areas were greatest in Group IV. At the distal reference, absolute dense calcium and necrotic core areas were greater in Group III and IV than Group I and II. At the minimum lumen area site, absolute dense calcium area was greatest in Group IV (Fig. 2A). At the largest necrotic core site, absolute dense calcium and necrotic core areas were greatest in Group IV. At the proximal reference, relative dense calcium and necrotic core areas were greatest in Group IV. At the minimum lumen area site, relative dense calcium area was greatest, and in contrast relative fibrous area was smallest in Group IV (Fig. 2B). At the largest necrotic core site, relative dense calcium area was greatest, and in contrast relative fibrous area was smallest in Group IV. By volumetric analysis, absolute fibrous and fibro-fatty and dense calcium and necrotic core volumes were greatest in Group IV (Fig. 3A). Relative dense calcium and necrotic core volumes were greatest, and in contrast relative fibrous volume was smallest in Group IV (Fig. 3B). Also thin-cap fibroatheromas were observed more frequently in Group IV (10% vs 12% vs 8% vs 33%, P = 0.046, respectively).
The absolute plaque and dense calcium and necrotic core volumes and the relative dense calcium volume correlated positively with CACS (r = 0.470, P < 0.001, r = 0.318, P < 0.001, r = 0.313, P < 0.001, respectively), in contrast the relative fibrous volume correlated negatively with CACS (r = -0.328, P < 0.001).
The present study demonstrated that 1) CAD patients with high CACS was oldest, and hypertension was observed most frequently, and had the lowest high-density lipoprotein-cholesterol level; 2) the absolute and relative dense calcium area were greatest, and in contrast relative fibrous area was smallest at the minimum lumen area site in patients with highest CACS; 3) the absolute fibrous and fibro-fatty and dense calcium and necrotic core volumes were greatest, and relative dense calcium and necrotic core volumes were greatest, and in contrast relative fibrous volume was smallest in patients with highest CACS; 4) the absolute plaque and dense calcium and necrotic core volumes and the relative dense calcium volume positively correlated with calcium scores, in contrast the relative fibrous volume negatively correlated with CACS.
CACS can be quantified using MDCT and calcification scores can be related to the extent and severity of atherosclerotic disease and can improve the prediction of CAD risk. Several studies demonstrated relations between the coronary calcification and the severity of coronary artery disease and clinical events. Ho et al. (17) reported that as CACS increased, there was a corresponding increase in frequency of MDCT obstructive disease and a CACS > 400 was associated with increased risk of significantly obstructive stenosis. Also this study has shown that increasing age, male gender, and the presence of hypertension and hyperlipidemia are significantly associated with higher CACS. Church et al. (18) reported that CACS can identify individuals at increased risk for coronary heart disease events who otherwise would be considered low-risk based on clinical assessment and CACS of zero is associated with very low risk for coronary heart disease in the short to intermediate term regardless of the number of risk factors present.
Previous IVUS studies have shown that CACS was associated with plaque burden and morphology. Nicholls et al. (19) reported that high calcium index patients had a greater atheroma volume. In the present study, total atheroma volume and percent atheroma volume were greatest in CAD patients with highest CACS. Okabe et al. (20) reported that mean plaque burden, calcified length, and arc of calcium increased significantly, while minimum lumen area decreased with increasing CACS. Also multivariate analysis showed a calcified length and an arc of calcium were significant predictors for CACS. In the present study, calcium-arc was greatest and calcium length was longest in CAD patients with highest CACS.
Vulnerable plaque in coronary artery can progress to plaque rupture and thrombosis, and have a strong potential to induce acute coronary syndrome. Also inflammation and necrotic core size play a greater role in the progression of atherosclerosis in diabetic subjects in sudden coronary death (21). In the present study, dense calcium and necrotic core components were greatest in lesions with highest calcium score compared to those with lower calcium score. Some investigators believe that calcium stabilizes the plaque, while others believe that it increases the shear stress and hence the risk of rupture. Almost all patients with recent acute coronary syndromes have measurable coronary calcium because of pre-existing moderate-to-advanced coronary artery disease. In these same individuals, flow-obstructing coronary lesions are not necessarily linked to calcium (22). However, several studies indicate that extensive coronary calcium by CT is related to increased incidences of myocardial infarction, obstructive coronary disease and death (23-25). Also our observations indicate that with increasing CACS the likelihood of thin-cap fibroatheroma also increases.
Few data are available about the relation between coronary calcium score and plaque components. Fujii et al. (26) reported that ruptured plaques are associated with a larger number of calcium deposits within an arc of < 90°, and Ehara et al. (27) reported that IVUS allows the identification of vulnerable plaques in coronary arteries, not only by identifying a fibro-fatty plaque and positive remodeling, but also by identifying a spotty pattern of calcification. Also this study has shown that the length of calcium deposits detected by IVUS within the culprit lesion segment was found to be positively correlated with the largest arc. Harada et al. (28) reported that MDCT is a promising approach for noninvasive detection of different types of coronary plaque and may therefore contribute to coronary risk stratification. However, the ability of MDCT to determine the volume of individual plaque components is limited. Moreover the edge of a calcified plaque appears to have a lower density than the internal region on MDCT. As a result of these effects, MDCT is prone to overestimate the volume of both low attenuated and calcified plaque. On the other hand, Carrascosa et al. (29) reported that MDCT can provide important information concerning the composition of atherosclerotic plaques in addition to detecting luminal obstruction. Galonska et al. (30) reported that coronary atherosclerotic plaques can be reliably identified and classified as either calcified or non-calcified by 16-slice MDCT in postmortem studies and might not be too far from being able to detect vulnerable plaques with CT technology. The result of the present study shows the association between CACS and vulnerable plaque components in patients with CAD. Therefore, cardiac MDCT can be used as a useful tool to detect not only significant atherosclerosis but also vulnerable plaque components non-invasively in patients with CAD.
There are several limitations to be mentioned. First, the present study was a retrospective single center study, so was subjected to limitations inherent in this type of clinical investigation. Second, IVUS and VH-IVUS imaging were performed at the discretion of the individual operators leading to potential selection bias. Third, there was a limitation using 20 MHz IVUS because this low frequency IVUS has a limitation to detect the plaque in detail, especially in the near field. Fourth, heavily calcified plaques may have induced an artifact regarding the codification of plaques by VH-IVUS resulting in an increase in necrotic core content.
In conclusion, it is suggested that CAD patients with high calcium score have more vulnerable plaque components (greater dense calcium and necrotic core-containing plaques) than those with low calcium score.
Figures and Tables
Fig. 1
The examples of coronary artery calcium detected by cardiac multidetector computed tomography (MDCT) (A) and plaque components assessed by virtual histology-intravascular ultrasound (VH-IVUS) (B).

Fig. 2
Absolute (A) and relative (B) plaque components at the minimum lumen area sites. Absolute dense calcium and relative dense calcium (%) areas were greatest in Group IV; in contrast, relative fibrous (%) area was smallest in Group IV.

Fig. 3
Absolute (A) and relative (B) plaque components by volumetric analysis. Absolute and relative dense calcium (%) and necrotic core (%) volumes were greatest in Group IV; in contrast, relative fibrous (%) volume was smallest in Group IV.

AUTHOR SUMMARY
Relationship between Coronary Artery Calcium Score by Multidetector Computed Tomography and Plaque Components by Virtual Histology Intravascular Ultrasound
Yun Ha Choi, Young Joon Hong, In Hyae Park, Myung Ho Jeong, Khurshid Ahmed, Seung Hwan Hwang, Min Goo Lee, Keun-Ho Park, Doo Sun Sim, Ju Han Kim, Youngkeun Ahn, Jeong Gwan Cho, Jong Chun Park and Jung Chaee Kang
The aim of this study was to evaluate the relationship between coronary artery calcium score (CACS) assessed by multidetector computed tomography (MDCT) and plaque components assessed by virtual histology-intravascular ultrasound in 172 coronary artery disease (CAD) patients with 250 coronary lesions. CACS was assessed according to Agatston scoring method by MDCT and patients were divided into four groups. Total atheroma volume was greatest in the group with highest calcium score. The absolute dense calcium (DC) and necrotic core (NC) volumes were greatest, and relative DC volume was greatest in the group with highest calcium score. In conclusion, CAD patients with high calcium score have more vulnerable plaque components than those with low calcium score.
References
1. Javadrashid R, Salehi A, Tarzamni MK, Aslanabadi N, Pak N. Diagnostic efficacy of coronary calcium score in the assessment of significant coronary artery stenosis. Kardiol Pol. 2010. 68:285–291.
2. Kitamura A, Kobayashi T, Ueda K, Okada T, Awata N, Sato S, Shimamoto T. Evaluation of coronary artery calcification by multi-detector row computed tomography for the detection of coronary artery stenosis in Japanese patients. J Epidemiol. 2005. 15:187–193.
3. Shaw LJ, Raggi P, Schisterman E, Berman DS, Callister TQ. Prognostic value of cardiac risk factors and coronary artery calcium screening for all-cause mortality. Radiology. 2003. 228:826–833.
4. Thompson GR, Partridge J. Coronary calcification score: the coronary-risk impact factor. Lancet. 2004. 363:557–559.
5. Mitsutake R, Niimura H, Miura S, Zhang B, Iwata A, Nishikawa H, Kawamura A, Kumagai K, Shirai K, Matsunaga A, Saku K. Clinical significance of the coronary calcification score by multidetector row computed tomography for the evaluation of coronary stenosis in Japanese patients. Circ J. 2006. 70:1122–1127.
6. LaMonte MJ, FitzGerald SJ, Church TS, Barlow CE, Radford NB, Levine BD, Pippin JJ, Gibbons LW, Blair SN, Nichamar MZ. Coronary artery calcium score and coronary heart disease events in an large cohort of asymptomatic men and women. Am J Epidemiol. 2005. 162:421–429.
7. Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, Liu K, Shea S, Szklo M, Bluemke DA, O'Leary DH, Tracy R, Watson K, Wong ND, Kronmal RA. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008. 358:1336–1345.
8. Wong ND, Hsu JC, Detrano RC, Diamond G, Eisenberg H, Gardin JM. Coronary artery calcium evaluation by electron beam computed tomography and its relation to new cardiovascular events. Am J Cardiol. 2000. 86:495–498.
9. Baumgart D, Schmermund A, Goerge G, Haude M, Ge J, Adamzik M, Sehnert C, Altmaier K, Groenemeyer D, Seibel R, Erbel R. Comparison of electron beam computed tomography with intracoronary ultrasound and coronary angiography for detection of coronary atherosclerosis. J Am Coll Cardiol. 1997. 30:57–64.
10. Funabashi N, Misumi K, Ohnishi H, Asano M, Komuro I. Characterization and morphology of atherosclerotic plaque of coronary arteries: utility of electron-beam tomography to detect non-calcified plaque: a comparison with conventional coronary angiography and intravascular ultrasound. Int J Cardiol. 2007. 115:108–113.
11. Henneman MM, Schuijf JD, Pundziute G, van Werkhoven JM, van der Wall EE, Jukema JW, Bax JJ. Non-invasive evaluation with multislice computed tomography in suspected acute coronary syndrome: plaque morphology on multislice computed tomography versus coronary calcium score. J Am Coll Cardiol. 2008. 52:216–222.
12. Roberts WL, Moulton L, Law TC, Farrow G, Cooper-Anderson M, Savory J, Rifai N. Evaluation of nine automated high-sensitivity C-reactive protein methods: implications for clinical and epidemiological applications. Part 2. Clin Chem. 2001. 47:418–425.
13. Reiber JH, van der Zwet PM, Koning G, von Land CD, van Meurs B, Gerbrands JJ, Buis B, van Voorthuisen AE. Accuracy and precision of quantitative digital coronary arteriography: observer-, short-, and medium-term variabilities. Cathet Cardiovasc Diagn. 1993. 28:187–198.
14. Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990. 15:827–832.
15. Mintz GS, Nissen SE, Anderson WD, Bailey SR, Erbel R, Fitzgerald PJ, Pinto FJ, Rosenfield K, Siegel RJ, Tuzcu EM, Yock PG. American College of Cardiology Clinical Expert Consensus Document on Standards for Acquisition, Measurement and Reporting of Intravascular Ultrasound Studies (IVUS). A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2001. 37:1478–1492.
16. Nair A, Kuban BD, Tuzcu EM, Schoenhagen P, Nissen SE, Vince DG. Coronary plaque classification with intravascular ultrasound radiofrequency data analysis. Circulation. 2002. 106:2200–2206.
17. Ho JS, Fitzgerald SJ, Stolfus LL, Wade WA, Reinhardt DB, Barlow CE, Cannaday JJ. Relation of a coronary artery calcium score higher than 400 to coronary stenoses detected using multidetector computed tomography and to traditional cardiovascular risk factors. Am J Cardiol. 2008. 101:1444–1447.
18. Church TS, Levine BD, McGuire DK, Lamonte MJ, Fitzgerald SJ, Cheng YJ, Kimball TE, Blair SN, Gibbons LW, Nichaman MZ. Coronary artery calcium score, risk factors, and incident coronary heart disease events. Atherosclerosis. 2007. 190:224–231.
19. Nicholls SJ, Tuzcu EM, Wolski K, Sipahi I, Schoenhagen P, Crowe T, Kapadia SR, Hazen SL, Nissen SE. Coronary artery calcification and changes in atheroma burden in response to established medical therapies. J Am Coll Cardiol. 2007. 49:263–270.
20. Okabe T, Mintz GS, Weigold WG, Roswell R, Joshi S, Lee SY, Lee B, Steinberg DH, Roy P, Slottow TL, Kaneshige K, Torguson R, Xue Z, Satler LF, Kent KM, Pichard AD, Weissman NJ, Lindsay J, Waksman R. The predictive value of computed tomography calcium scores: a comparison with quantitative volumetric intravascular ultrasound. Cardiovasc Revasc Med. 2009. 10:30–35.
21. Burke AP, Kolodgie FD, Zieske A, Fowler DR, Weber DK, Varghese PJ, Farb A, Virmani R. Morphologic findings of coronary atherosclerotic plaques in diabetics: a postmortem study. Arterioscler Thromb Vasc Biol. 2004. 24:1266–1271.
22. Schmermund A, Erbel R. Unstable coronary plaque and its relation to coronary calcium. Circulation. 2001. 104:1682–1687.
23. Pitt B, Rubenfire M. Risk stratification for the detection of preclinical coronary artery disease. Circulation. 1999. 99:2610–2612.
24. Raggi P, Callister TQ, Cooil B, He ZX, Lippolis NJ, Russo DJ, Zelinger A, Mahmarian JJ. Identification of patients at increased risk of first unheralded acute myocardial infarction by electron-beam computed tomography. Circulation. 2000. 101:850–855.
25. Arad Y, Spadaro LA, Goodman K, Newstein D, Guerci AD. Prediction of coronary events with electron beam computed tomography. J Am Coll Cardiol. 2000. 36:1253–1260.
26. Fujii K, Carlier SG, Mintz GS, Takebayashi H, Yasuda T, Costa RA, Moussa I, Dangas G, Mehran R, Lansky AJ, Kreps EM, Collins M, Stone GW, Moses JW, Leon MB. Intravascular ultrasound study of patterns of calcium in ruptured coronary plaques. Am J Cardiol. 2005. 96:352–357.
27. Ehara S, Kobayashi Y, Kataoka T, Yoshiyama M, Ueda M, Yoshikawa J. Quantification of coronary calcification by intravascular ultrasound. Circ J. 2007. 71:530–535.
28. Harada K, Amano T, Uetani T, Funahashi H, Arai K, Okada K, Hirashiki A, Hayashi M, Oshima S, Ishii H, Izawa H, Matsubara T, Murohara T. Accuracy of 64-slice multidetector computed tomography for classification and quantitation of coronary plaque: comparison with integrated backscatter intravascular ultrasound. Int J Cardiol. 2011. 149:95–101.
29. Carrascosa PM, Capuñay CM, Garcia-Merletti P, Carrascosa J, Garcia MF. Characterization of coronary atherosclerotic plaques by multidetector computed tomography. Am J Cardiol. 2006. 97:598–602.
30. Galonska M, Ducke F, Kertesz-Zborilova T, Meyer R, Guski H, Knollmann FD. Characterization of atherosclerotic plaques in human coronary arteries with 16-slice multidetector row computed tomography by analysis of attenuation profiles. Acad Radiol. 2008. 15:222–230.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download