Abstract
Suitability rate of endovascular aneurysm repair (EVAR) and the anatomic features causing unsuitability have not been well determined in Asian patients who have abdominal aortic aneurysm (AAA). In a single Korean center, a total of 191 patients with abdominal aortic aneurysm (maximal diameter ≥ 4 cm) were identified. Aortoiliac morphologic characteristics in contrast-enhanced computed tomography images were retrospectively reviewed to determine suitability for EVAR with four FDA-approved stent-grafts. AAA was considered ideally suitable for EVAR in 46.6% of patients. The most frequent causes for unsuitability were common iliac artery (CIA) aneurysm (61.8%) and excessive neck angulation (52.9%). Problems such as small and/or short neck and small access were found in minor incidences. If CIA aneurysm is dealt by overstenting with sacrifice of internal iliac artery, suitability rate can increase to 65%. Larger aneurysms were more frequently unsuitable for EVAR and had more chance of having multiple unfavorable features. In conclusion, the overall feasibility rate for EVAR in Korean patients was not different from that in Western patients. However, considering the difference in the major causes of unsuitability, more attention has to be paid to neck angulation and CIA aneurysm to provide EVAR for more Korean patients especially who have large aneurysm.
Although endovascular aneurysm repair (EVAR) has been established as a standard intervention for abdominal aortic aneurysm (AAA) (1, 2), it is not ideal or feasible for the patients who have challenging anatomic features that cannot be overcome by the design of currently available devices (3-6). The estimated proportion of AAA patients suitable for EVAR varies and has been reported as high as 80% (7-11). However, most of the reports came from Western countries and there have been only a few data from Asian population who have smaller body size and subsequently may have different anatomic features (12, 13).
With rapid aging of the population and economical development in East Asia, the incidence of newly diagnosed AAA is rapidly increasing (14, 15). So, it would be pertinent to answer the following questions; 1) how large proportion of patients with AAA can be effectively treated with EVAR in the region, 2) are the suitability rate and anatomic features different from those of Western patients, 3) is there need for modification of device design specific to Asian patients? This study aimed to answer those questions by retrospective analysis of the aortoiliac morphology in a single-center Korean patient cohort.
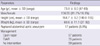
From the database linked to the electronic medical records of the hospital, the patients who had AAA as one of their diagnoses were sought. Among them, only the patients who underwent contrast-enhanced spiral computed tomography (CT) and whose maximal aneurysm diameter was 40 mm or larger were included for this study. In a 7-yr period from July 2003 through August 2010, a total of 191 patients were identified (Table 1). For these patients, suitability of the aneurysm morphology for EVAR was retrospectively investigated by review of their CT images.
CT angiography was performed using a slice thickness of 2.5 to 4 mm. Morphologic characteristics of the aneurysm such as the diameters and the lengths of the proximal aortic neck and both common iliac arteries were measured with digital calipers on a PACS workstation. All the diameters were measured in the perpendicular plane to the vessels' long axes on the sagittal or coronal images. The lengths were measured in three-dimensionally rendered images. Infrarenal neck angulation (in degrees) was determined with the digital goniometer. For the common iliac artery, the maximal diameter was recorded. To assess the suitability for access of device, the narrowest diameter was determined along the external iliac and common femoral arteries at both sides. All the measurements were performed by a single reviewer.
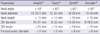
Suitability of EVAR was determined according to the criteria recommended by the manufacturers (Table 2) of the four FDA-approved devices which are available in Korea; AneuRx® (Medtronic Cardiovascular, Santa Rosa, CA, USA), Talent® (Medtronic CardioVascular), Zenith® (Cook Medical., Bloomington, IN, USA), and Excluder® (W. L. Gore & Associates, Flagstaff, AZ, USA). The aneurysm was considered suitable for EVAR when the morphologic characteristics met the manufacturer's recommendation of any of the four devices. In determining the suitability, only the above-mentioned characteristics that were measurable in numerical values were considered. Factors prone to subjective variation such as wall calcification, luminal thrombus or atheroma, shape of the neck (straight vs conical), and iliac artery tortuosity were not taken into consideration.
All values are given as mean ± standard deviation. Comparison between groups were performed for statistical significance with Student t-test, one-way ANOVA, Pearson's correlation, or Fisher's exact tests according to the type of the variables. Those tests were performed using SPSS version 15.0 (SPSS Inc, Chicago, IL, USA).
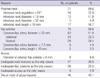
Endovascular repair of the abdominal aortic aneurysm would have been feasible in 89 patients (46.6%) if the manufacturer's guidelines had been strictly followed without compromise of the criteria. The most frequent causes for unsuitability were aneurysmal dilatation of the common iliac artery and excessive angulation of the aneurysm neck (Table 3). Especially, common iliac artery dilatation was the most frequently found problem (63/191, 33.0%) and bilateral dilatation was present in almost the same number of patients as unilateral dilatation. The problem of short proximal landing zone was found in a relatively minor proportion of the patients (17/191, 8.9%). Other factors that may be expected to be present in Asian population whose body size is small were present also in relatively small numbers; small neck diameter in 12 patients (6.3%), small common iliac artery in 5 patients (2.6%), and small external iliac/femoral arteries in 9 patients (4.7%).
The problems making EVAR unsuitable were present in the neck and the common iliac arteries with almost equal incidences. In addition, both the neck and common iliac arteries had morphological characteristics unsuitable for EVAR in 46 patients (24% of entire patients and 45.1% of unsuitable patients, Table 3). When the characteristics of the aortoiliac morphology in this series were compared with previous reports from other countries (12, 13, 16, 17), there was no difference in the diameter and length of the proximal neck and the lengths of the common iliac arteries. The only remarkable difference was the larger average diameter of the common iliac arteries in our patients (Table 4).
Between the patients who had aneurysm suitable for EVAR and those who did not, there was no significant difference in the age (72.2 ± 8.3 vs 73.6 ± 7.6 yr), height (165.5 ± 7.4 vs 163.9 ± 8.8 cm), or body weight (62.2 ± 10.0 vs 59.2 ± 10.8 kg). There was also no significant difference in EVAR suitability between genders (47.4% in male vs 42.9% in female). While female patients had more chance of small access (external iliac and common femoral artery diameter < 8 mm) than male patients (8.6% vs 3.8%), the difference was not statistically significant. Although the height (160.6 ± 8.1 cm vs 164.9 ± 8.2 cm) and body weight (54.5 ± 13.4 kg vs 60.9 ± 13.4 kg) were smaller in the patients who had small access problem, the difference was not statistically significant, either.
Meanwhile, suitability of EVAR was significantly correlated with the maximal diameter of aneurysm sac. More than 60% of aneurysms with the maximal diameter 6 cm or less were suitable for EVAR without compromise of the manufacturer's guidelines. On the contrary, the suitability decreased markedly as the aneurysm sac size increased larger than 6 cm (P < 0.05, Fig. 1). In addition, the larger the aneurysm became, the more was the chance of having problems in both of the proximal and the distal landing zones. Almost 60% of the aneurysms with the maximal diameter 8 cm or larger had unfavorable morphology in the neck and common iliac arteries at the same time.
Considering the aging of the large population along with economic growth and advance of health care system in Asia, there will be a rapid increase in the incidence of aortic aneurysm in the region. The question of whether the suitability for EVAR is the same between different races would be pertinent to modifying the stent-graft design targeting the large potential market. However, we could find only two articles addressing this issue in previous literature (12, 13). While the former two studies investigated the anatomical features only in the patients who underwent endovascular repair, our study included all the patients who had abdominal aortic aneurysm with the maximal diameter 4 cm or larger. As a result, many patients who declined any intervention or underwent conventional surgery were subject to analysis (Table 1). Many of our surgical patients could have been treated with endovascular procedure if the FDA-approved commercial devices had been available (they became available in Korea since 2007). This fact makes our study helpful for giving insight into the suitability rate for EVAR among the entire AAA population and reasons for unsuitability.
According to our results, morphological characteristics 'ideal' for stent-graft implantation were found in about a half of Korean AAA patients. If the criterion of common iliac artery diameter is compromised by placement of the iliac limb of stent-graft in the external iliac artery and sacrificing one or both internal iliac arteries, the proportion of 'feasible' patients can increase to 65%. However, the actual proportion of 'ideal' or 'feasible' patients would have been less if we had taken into consideration other factors prone to subjective variation such as wall calcification, luminal thrombus or atheroma, shape of the neck, and iliac artery tortuosity. Considering the all of above factors, we think that the overall 'feasibility' rate for EVAR may be almost the same or a little lower in Korean patients compared with Western population. Although the estimates regarding the rate of suitability or feasibility for EVAR vary between different reports, recent Western studies reported 48%-66% rate with current commercial devices (7, 8).
While the overall feasibility rate is not thought much different, we could find differences between our data and previous reports regarding the anatomical features making EVAR unsuitable. In a report from the Netherlands (7), unsuitability was more frequently caused by inadequate proximal neck, especially inadequate length of the neck, than by inadequate iliac anatomy. On the contrary, in our series, neck features and iliac anatomy were the reasons for unsuitability in almost the same frequency and excessive angulation was the most frequent features making the neck unstable for EVAR. Our data also shows some difference from others reports that investigated Asian population. Cheng et al. reported that both the neck and common iliac arteries of Chinese patients were larger and shorter compared with Caucasians (12). However, the only difference between our patients and previous Western series (and the only common finding between ours and the Chinese report) was that the common iliac artery was significantly larger in Asian patients. Another difference from Cheng's report was that our patients had significantly higher incidence of severe neck angulation. It could be explained by the difference of the study material because Cheng's report included only the patients who underwent EVAR while our study examined all the patients with AAA. We have to admit that our measurement of the neck length may be inaccurate in some patients, because it was made in sagittal or coronal view (instead of center-line program) and sometimes with 4-mm-thick slices that is too large for a short neck. However, considering that the difference of average neck lengths was just 5 mm between ours and the Chinese series that included only the EVAR cases, we do not think the possible measurement error had a significant impact in interpretation of our data.
In a study of Hawaiian patients, Masuda et al. (13) reported that the external iliac artery diameter was significantly smaller in Asians than in other races (8.2 vs 9.5 mm) and this factor was related with higher incidences of access-related and device-related complications after aortoiliac endografting. However, the mean external iliac artery diameter of our patients was well above 9 mm and small access problem was found in only 9 patients (4.7%). The difference may be related to the fact that the patients in Hawaiian study were significantly older than ours. Although their older patients might have smaller body size and subsequently smaller iliofemoral arteries than ours, their data did not mention about the body size of the patients.
As both of Chinese series and ours show that the common iliac arteries are larger in AAA patients, common iliac artery aneurysm may be the most frequent problem that makes EVAR more complicated in Asian patients. Among Western literature, we could find only one report addressing the issue of common iliac artery aneurysm in AAA patients. Armon et al. (18) reported that the mean common iliac artery diameter was significantly larger in AAA patients compared with general population. They suggested that common iliac artery aneurysm in AAA patients should be defined as those greater than 2.4 cm in diameter. With their definition, the incidences of unilateral and bilateral common iliac artery aneurysm were 16% and 12%, respectively. Our series shows the similar incidences (14.1% and 15.2%) and internal iliac artery coverage would have been necessary in 34% of our patients if EVAR had been performed. Cheng et al. (12) reported that internal iliac artery coverage was necessary in 51% of Chinese patients undergoing EVAR.
Correlation between EVAR feasibility with gender, age, and maximal aneurysm diameter has been controversial in the previous studies (7, 8, 19, 20). In our series, feasibility for EVAR was not different according to the patient's age or gender. However, there was a strong correlation between the size of the aneurysm and EVAR suitability. As the maximal aneurysm diameter increases larger than 6 cm, the suitability decreased significantly. In addition, it is worth mentioning that unsuitability was caused by multiple anatomic features rather than a single factor as the aneurysm size increases. Our result is concordant with the previous studies which showed that larger aneurysms were less suitable for EVAR and had higher incidence of complications or unsatisfactory outcome after EVAR (20-22).
In conclusion, the overall 'feasibility' rate for endovascular repair of abdominal aortic aneurysm in Korean patients is not thought to be much different compared with Western patients. However, considering that the most frequent causes for unsuitability were different from those in Western patients, future modification of stent-graft design should address excessive neck angulation and more attention has to be paid to common iliac artery aneurysm to provide endovascular treatment for more of Korean patients especially those who have large aneurysm.
Figures and Tables
Fig. 1
Maximal diameter of abdominal aortic aneurysm versus EVAR suitability. EVAR, endovascular aneurysm repair; AAA, abdominal aortic aneurysm.

AUTHOR SUMMARY
Suitability of Endovascular Repair with Current Stent Grafts for Abdominal Aortic Aneurysm in Korean Patients
Kay-Hyun Park, Cheong Lim, Jae Hang Lee and Jae Suk Yoo
In 191 patients with abdominal aortic aneurysm (AAA), aortoiliac morphologic characteristics in CT images were reviewed to determine suitability for EVAR. EVAR was ideally suitable in 46.6% of AAA patients. The frequent causes for unsuitability were common iliac artery (CIA) aneurysm (61.8%) and excessive neck angulation (52.9%). Unsuitable neck or small access was found in minor incidences. Larger aneurysms were more frequently unsuitable for EVAR and had more chance of having multiple features making EVAR unsuitable. In conclusion, the overall feasibility rate for EVAR was not different between Korean and Western patients. However, the difference in the major causes of unsuitability requires further consideration in designing stent-graft for EVAR.
References
1. EVAR trial participants. Endovascular aneurysm repair versus open repair in patients with abdominal aortic aneurysm (EVAR trial 1): randomized controlled trial. Lancet. 2005. 365:2179–2186.
2. Prinssen M, Verhoeven EL, Buth J, Cuypers PW, van Sambeek MR, Balm R, Buskens E, Grobbee DE, Blankensteijn JD. Dutch Randomized Endovascular Aneurysm Management (DREAM) Trial Group. A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. N Engl J Med. 2004. 351:1607–1618.
3. Torella F. Effect of improved endograft design on outcome of endovascular aneurysm repair. J Vasc Surg. 2004. 40:216–221.
4. Greenberg RK, Clair D, Srivastava S, Bhandari G, Turc A, Hampton J, Popa M, Green R, Ouriel K. Should patients with challenging anatomy be offered endovascular aneurysm repair? J Vasc Surg. 2003. 38:990–996.
5. Chisci E, Kristmundsson T, de Donato G, Resch T, Setacci F, Sonesson B, Setacci C, Malina M. The AAA with a challenging neck: outcome of open versus endovascular repair with standard and fenestrated stent-grafts. J Endovasc Ther. 2009. 16:137–146.
6. Sternbergh WC 3rd, Carter G, York JW, Yoselevitz M, Money SR. Aortic neck angulation predicts adverse outcome with endovascular abdominal aortic aneurysm repair. J Vasc Surg. 2002. 35:482–486.
7. Simons P, van Overhagen H, Nawijn A, Bruijninckx B, Knippenberg B. Endovascular aneurysm repair with a bifurcated endovascular graft at a primary referral center: influence of experience, age, gender, and aneurysm size on suitability. J Vasc Surg. 2003. 38:758–761.
8. Carpenter JP, Baum RA, Barker CF, Golden MA, Mitchell ME, Velazquez OC, Fairman RM. Impact of exclusion criteria on patient selection for endovascular abdominal aortic aneurysm repair. J Vasc Surg. 2001. 34:1050–1054.
9. Wolf YG, Fogarty TJ, Olcott C IV, Hill BB, Harris EJ, Mitchell RS, Miller DC, Dalman RL, Zarins CK. Endovascular repair of abdominal aortic aneurysms: eligibility rate and impact on the rate of open repair. J Vasc Surg. 2000. 32:519–523.
10. Zarins CK, Wolf YG, Lee WA, Hill BB, Olcott C IV, Harris EJ, Dalman RL, Fogarty TJ. Will endovascular repair replace open surgery for abdominal aortic aneurysm repair? Ann Surg. 2000. 232:501–507.
11. Armon MP, Yusuf SW, Latief K, Whitaker SC, Gregson RH, Wenham PW, Hopkinson BR. Anatomical suitability of abdominal aortic aneurysms for endovascular repair. Br J Surg. 1997. 84:178–180.
12. Cheng SW, Ting AC, Ho P, Poon JT. Aortic aneurysm morphology in Asians: features affecting stent-graft application and design. J Endovasc Ther. 2004. 11:605–612.
13. Masuda EM, Caps MT, Singh N, Yorita K, Schneider PA, Sato DT, Eklof B, Nelken NA, Kistner RL. Effect of ethnicity on access and device complications during endovascular aneurysm repair. J Vasc Surg. 2004. 40:24–29.
14. Ishikawa S, Takahashi T, Sato Y, Suzuki M, Ohki S, Oshima K, Mohara J, Nameki T, Otani Y, Morishita Y. Screening cost for abdominal aortic aneurysms: Japan-based estimates. Surg Today. 2004. 34:828–831.
15. Cheng SW, Ting AC, Tsang SH. Epidemiology and outcome of aortic aneurysm in Hong Kong. World J Surg. 2003. 27:241–245.
16. EUROSTAR Data Registry Centre. EUROSTAR participants progress report 8. 2003.
17. Matsumura JS, Brewster DC, Makaroun MS, Naftel DC. A multicenter controlled clinical trial of open versus endovascular treatment of abdominal aortic aneurysm. J Vasc Surg. 2003. 37:262–271.
18. Armon MP, Wenham PW, Whitaker SC, Gregson RH, Hopkinson BR. Common iliac artery aneurysms in patients with abdominal aortic aneurysms. Eur J Vasc Endovasc Surg. 1998. 15:255–257.
19. Velazquez OC, Larson RA, Baum RA, Carpenter JP, Golden MA, Mitchell ME, Pyeron A, Barker CF, Fairman RM. Gender-related differences in infrarenal aortic aneurysm morphologic features: issues relevant to Ancure and Talent endografts. J Vasc Surg. 2001. 33:2 Suppl. S77–S84.
20. Welborn MB 3rd, Yau FS, Modrall JG, Lopez JA, Floyd S, Valentine RJ, Clagett GP. Endovascular repair of small abdominal aortic aneurysms: a paradigm shift? Vasc Endovascular Surg. 2005. 39:381–391.
21. Ouriel K, Srivastava SD, Sarac TP, O'hara PJ, Lyden SP, Greenberg RK, Clair DG, Sampram E, Butler B. Disparate outcome after endovascular treatment of small versus large abdominal aortic aneurysm. J Vasc Surg. 2003. 37:1206–1212.
22. Peppelenbosch N, Buth J, Harris PL, van Marrewijk C, Fransen G. Diameter of abdominal aortic aneurysm and outcome of endovascular aneurysm repair: does size matter? A report from EUROSTAR. J Vasc Surg. 2004. 39:288–297.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download