Abstract
Work-related musculoskeletal disorders (WMSDs) can be compensated through the Industrial Accident Compensation Insurance Act. We looked at the characteristics of WMSDs in worker's compensation records and the epidemiological investigation reports from the Occupational Safety and Health Research Institute (OSHRI). Based on the records of compensation, the number of cases for WMSDs decreased from 4,532 in 2003 to 1,954 in 2007. However the proportion of WMSDs among the total approved occupational diseases increased from 49.6% in 2003 to 76.5% in 2007, and the total cost of WMSDs increased from 105.3 billion won in 2004 to 163.3 billion won in 2007. The approval rate of WMSDs by the OSHRI accounted for 65.6%. Ergonomic and clinical characteristics were associated with the approval rate; however, the degenerative changes had a minimal affect. This result was in discordance between OSHRI and the Korea Workers' Compensation & Welfare Service. We presumed that there were perceptional gaps in work-relatedness interpretation that resulted from the inequality of information in ergonomic analyses. We propose to introduce ergonomic analysis to unapproved WMSDs cases and discuss those results among experts that will be helpful to form a consensus among diverse groups.
Work-related musculoskeletal disorders (WMSDs) are a type of functional disorder caused by external factors such as occupational repetitive movements, overexertion, awkward postures, and vibration. The accumulation of minor injuries on tissues can lead to musculoskeletal disorders (MSDs). The body parts commonly affected are the waist, neck, shoulders, arms, and wrists.
There are three criteria for approving compensation claims for WMSDs under the Industry Accident Compensation Insurance Act (IACI Act). On a basic level, work based activities that repetitively places stress on the body that results in a MSD in a specific part of the body should be identified. Second, there is a case that work based activities may aggravate preexisting diseases. Last, there is evidence that a sudden and rapid external force can cause physical injury. For this case, it is compounded between accidental low back pain and other WMSDs. There are several conditions that may be considered; the injured area must be affected in daily tasks or be related to past work history. For example, if the office worker was stricken by low back pain when carrying a heavy object, the symptom can be classified as accidental low back pain. In contrast, the symptoms will be classified as non-accidental low back pain if a construction worker incurs a low back pain during a routine task that involves heavy weights. Accidental low back pain was classified as an occupational injury, but it was classified as an occupational disease in 2006.
The medical expert groups debated criteria 2-the aggravation of a preexisting disease. The challenge was to determine whether the aggravation was caused by work or whether it arose outside of work. Moreover, there is often a difference of opinion in determining whether different instances of aggravation are caused by natural aging or accumulated injury. Clinical radiological tools such as radiography, computed tomography, and magnetic resonance imaging are commonly used to judge the level of damage in the body but the degeneration phenomena observed by these tools are similar to the natural progress of aging. This situation requires the quantitative measurement of musculoskeletal stress on the worker by additional tools. Even after a decision of the quantitative measurement, there was a lack of sufficient epidemiological evidence for reference and a comparison for the quantity of musculoskeletal stress. In part, the agreement in opinion can be easily reached with the compensation approval of WMSDs for typical occupations that can be assessed with the aid of ergonomic tools. However, debate continues concerning not-typical occupations that are not line processes in manufacturing (that include complex tasks or affect body parts) that are quite difficult for ergonomic tools to examine such as the cervical vertebrae and lower limbs.
This study introduces the occurrence of WMSDs in Korea based on national statistical data from worker compensation records. We also reviewed epidemiological investigation cases from the Occupational Safety and Health Research Institute (OSHRI) regarding MSDs and their ergonomic analyses in order to examine how epidemiological evidence is applied to the OSHRI decision-making process.
This study displayed the status of WMSDs in Korea with data classified as MSDs among those approved as occupational diseases by the IACI Act. At present, statistics pertaining to occupational diseases are compiled in a periodic medical screening system for occupational diseases and in worker's compensation records; however, statistics for MSDs cannot be assembled from the periodic medical screening system for occupational disease as they are excluded from the test items. In the current IACI Act, MSDs are classified into 4 categories, musculoskeletal burdened work (including upper & lower limb disorders), non-accidental low back pain, accidental low back pain, and carpal tunnel syndrome. We obtained detailed information by acquiring the additional data of the names of the disorders and the circumstances of disorder occurrence through the OSHRI computer network and rearranged the data according to the anatomical parts affected by the disease occurrence.
For the criteria of work-relatedness, studies of MSDs among occupational disease epidemiologic investigations requested by the Korea Workers' Compensation & Welfare Service (COMWEL) and performed by the OSHRI (between 1992 and 2009) were analyzed. The characteristics of gender, age, the name of the disease, the anatomical part(s) associated with the disease occurrence, the cause of the disease occurrence, the duration of work, the industrial workplace classification, the job classification of the work activity, the size of the company, and other information were analyzed, according to the affected body parts (including the neck, upper limbs, lower back, and lower limbs). For common diseases among anatomical parts, the application method of the work-relatedness criteria and the quoted epidemiological grounds were also reviewed.
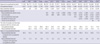
According to worker's compensation statistics in Korea, the occurrence of WMSDs increased from 124 cases in 1998 to 4,532 in 2003 and then gradually decreased from 4,112 cases in 2004 to 2,901 in 2005. In 2006, the figure increased again to 6,233 cases; however, this was largely due to the inclusion of accidental low back pain as a type of WMSDs. Before 2006, accidental low back pain was not included in the WMSDs statistics. The inclusion in 2006 had a great effect on the sudden increase of WMSDs cases in 2007. If those cases are removed from the total, the number drops from 2,621 cases in 2006 to 1,954 cases in 2007 and shows a decreasing trend since the peak in 2003. Accidental low back pain also decreased from 5,769 cases in 2007, 3,401 cases in 2008, to 2,472 cases in 2009 and confirmed an overall decreasing trend. Strenuous work causing a disorder in the upper limbs peaked in 2004 with 2,953 cases (though this number has since decreased) and occurred on a greater scale than the cases of low back pain; however, it has decreased sharply since 2008. Accidental low back pain decreased, whereas non-accidental low back pain increased (Table 1).
The ratio of MSD cases to work-related disorders cases was approximately 10% in the 1990s and showed a sharp increased since 2000. It currently is 60%-70%. Its percentage in the total approved occupational accident figures was 6%-8% over the last 3 yr (Table 1). The total amount of the industrial accident compensation insurance expenses was 105.3 billion won in 2004 and increased to 163.3 billion won in 2007. The proportion of compensated expenses reached 69.2% for occupational disease and 7.0% for the total compensation fund in 2008 (1).
In 2009, the distribution of 6,234 cases of WMSDs was as follows: 2,472 cases of accidental low back pain (39.7%), 2,407 cases of non-accidental low back pain (38.6%), and 1,355 cases of musculoskeletal burden work (21.7%). The general characteristics of WMSDs included 4,828 cases (77.5%) for males and 1,406 cases (22.5%) for females. In terms of age, we found 1,991 cases (31.9%) in their 30s, 1,867 cases (29.9%) in their 40s, 1,294 cases (20.8%) in their 50s, 643 cases (10.3%) under 20, and 439 cases (7%) over age 60. An analysis of MSD occurrence by workplace scale showed the greatest number of occurrences of 4,373 cases (80%) at workplaces with less than 50 employees, followed by 528 cases (9.7%) at workplaces with 100-499 employees, 415 cases (7.6%) at workplaces with 50-99 employees, 78 cases (1.4%) at workplaces with 500-999 employees, and 75 cases (1.4%) at workplaces with more than 1,000 employees. The occurrence number by location (provinces) was Gyeonggi, Gyeongsang, Seoul, Chungcheong, Jeolla, and Gangwon, respectively.
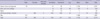
We extracted the disease name and outbreak situation information of 5,190 cases from 6,234 cases of WMSDs in 2009 and analyzed the anatomical sites of occurrence and the types of MSDs. An analysis of the outbreak area and the types of MSDs showed the following order: 2,281 cases (42.9%) of strain and tension in joints and ligaments, 1,981 cases (37.3%) of an intervertebral disk disorder; 788 cases (14.8%) of soft tissue (muscles and tendons) damage, 242 cases (4.6%) of other bone, joint, or cartilage disorder, and 22 cases (0.4%) of nerve disorder. Looking at each body part, musculoskeletal damage in the lumbar region was the highest at 4,152 cases (78.1%), neck and shoulder disorders numbered 510 cases (9.6%), hand and wrist disorders accounted for 317 cases (6.0%), arm and elbow disorders numbered 190 cases (3.6%), and lower limb disorders numbered 122 cases (2.3%). Looking at the proportion of regional MSDs for each disorder type, soft tissue damage was to most common in the shoulders followed by the arms and elbows, then the hands and wrists, and the strain and tension in joints and ligaments was most common for lumbar sprains, cervical sprains, and sprains of the hands and wrist. Other bone, joint and cartilage disorders were most common in the waist and knees. The most common disease among other bone, joint, and cartilage disorders of the waist was a compression fracture. Intervertebral damage of the lumbar vertebrae was found in 1,859 cases, showing an increase from the 967 cases in 2004 and significantly more than the 122 cases of the cervical vertebrae. Looking at each regional MSD, cervical intervertebral damage was the most frequent. In the shoulders, arms, and elbows, and hand and wrists, soft tissue damage (of muscles and tendons) accounted for the majority, and other bone, joint and cartilage damage accounted for the majority of leg (knee) MSDs. Of the 4,152 cases of MSDs in the lumbar region, intervertebral disk damage accounted for 1,859 cases; sprains, and tension in the joints and ligaments accounted for 2,184 cases; and other bone, joint, and cartilage disorders accounted for 107 cases (Table 2). Hence, lumbar sprains and lumbar compression fractures showed an increase after the inclusion of accidental low back pain in 2005.
The majority of WMSDs in Korea were intervertebral disk disorders in the cervical vertebrae and the lumbar vertebrae (such as intervertebral disk hernia) and the majority of sprains and tension in the joints and ligaments were lumbar sprains. Last of all, nervous and vascular disorders were minimal.
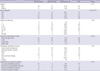
The OSHRI started to conduct research in 1992, with the total number of MSDs climbing to 170 cases as of 2009. We secured 127 cases as documents; the number of cases engaged in the manufacturing industry was 104 (82%) and males were 94 cases (74%) (Table 3).
The disease counts were 163 cases (Table 4). The occurrence site by anatomical classification was in the order of neck and upper limbs (99 cases), trunk (46 cases), lower limbs (18 cases), and whole body (1 case). The occurrence site according to a histological classification was in the order of discogenic disorders (59 cases), soft tissue (muscles and tendons) disorders (48 cases), bone, joint and cartilage disorders (24 cases), sprains of joints and ligaments (18 cases), nerve disorders (12 cases), and other (3 cases).
After examining the epidemiological studies, we identified 84 cases as highly work-related and 43 cases as having a low relationship to work. Some of the cases were partly approved in 6 individuals of the highly work-related ones. When we calculated the number of diseases, we confirmed that 107 cases (65.6%) were approved and 56 cases (34.4%) were not approved. We then determined that the approval of workers' compensation requests was affected by certain factors, including gender, age, the duration of exposure, and anatomical and pathological factors.
The approval rate 75.6% in women was higher than 61.9% in men, but the gender difference was not significant (P=0.14). The approval rate by age showed a decrease of 66.7% when the claimant was in their 20's, then reached a peak of 72.5% in the 30's and finally decreased. Aging was of borderline statistical significance according to a chi-square test for trend (P=0.21). The exposure period did not show a certain trend but showed a high rate of approval from over 1 yr to under 5 yr and from over 10 yr to under 20 yr (P=0.64, chi-square test for trend).
An analysis of the anatomical classification showed the following order: neck & upper arm (77.6%), trunk (56.5%), and lower limbs (27.8%). Analysis of the histological classification showed the following order: sprain in joints and ligaments (83.3%), soft tissue (muscles and tendons and membranes) disorders (74.5%), nervous disorders (66.7%), discogenic disorders (62.7%), and bone, joint, and cartilage disorders (41.7%) (P=0.03, chi-square test).
The OSHRI checks for five causal requirements in the determination of work-relatedness evaluations of MSDs. A clear diagnosis in which a concordance between work-related musculoskeletal risk factors and body parts of disorders exists, whether the job can be estimated as a high musculoskeletal burden job considering ergonomic factors such as the work intensity and work time, the period of exposure time, and if the condition exists due to factors other than work-related causes.
We could not check any abnormalities of clear diagnoses and the concordance between a disease and the site of anatomical burden (except herniated disk disorders). For example, if a patient with back pain declares that the cause of a herniated disk is an industrial accident and seeks approval for compensation, the investigator checks if a nervous disorder of the projected nerve roots exists or not by pressing it. The OSHRI determines the acceptance of the diagnostic name of the herniation of an intervertebral disk depending on the symptoms of the patient and a medical check by a doctor, an electromyogram, and nerve conduction tests.
According to some reports of radiologic findings, natural aging and external factors can differ in character; however, this cannot be used in all cases. The OSHRI recognizes that it is very difficult to state the absolute differences between natural aging and degeneration by extrinsic factors; in most cases, they appear together. Thus, they can reach a conclusion without concern of age or degeneration level themselves (other than some cases that they can differentiate absolutely).
Of the 127 cases, there were 94 cases (74.8%) in which age and degeneration were not mentioned as a cause in the final paragraph of the study. Among the 32 cases that mentioned age, there were 9 cases where they could not be differentiated by a degeneration level adjustment for age, instead in estimating it was more probable that the work factors effected early degenerative changes in lesions and approved the work-relatedness designation. There were also another 9 cases regarded as degeneration by natural aging, where they did not approve the work-relatedness designation. Six cases were regarded as definitely early degenerative changes comparative to the age of the claimant; however, one of them was not approved. Though an individual had a disease at its most common age, the approval rate was not affected. The approved cases numbered 3 and the unapproved cases numbered 3. These findings show that the OSHRI applies age and degeneration levels as a second priority in its decision criteria.
The variable that greatly affected work-related evaluations was the ergonomic analysis result. Most epidemiologic investigations held that ergonomic results were the major factor behind a decision. In fact, there was a strong association between the ergonomic analysis results and work-relatedness evaluations (P<0.01, chi-square test). The OSHRI approved 71 of 79 cases as musculoskeletal burden work. The unapproved cases were 5 of 32 cases and showed a considerable difference (Table 4).
The OSHRI used a variety of ergonomic tools and one or more ergonomic tools were used in 81 cases out of the 127 epidemiological investigations. The Rapid Upper Limb Assessment Tool (RULA) was most frequently used in neck disorders. Of 29 cases where RULA was used and in 17 cases it was used to assess neck disorders. When RULA was applied to neck disorders, a method of evaluating part of the neck separately (according to the angle of flexion and the extension of the neck scale) and a method of evaluating the total action level were used. A score of 5 or higher was given for neck flexion and an extension of 20° degrees or higher; this was used as the criteria of ergonomic stress.
On RULA, technical differences can exist (even between ergonomic factors) for the angle of the neck movement. A special standard to measure the angle of the neck movement (ISO11226) was used by the OSHRI after 2008; consequently, there were some differences between the neck angle measurements among different professionals. In addition, it should be noted that RULA did not suggest any quantitative criteria. Accordingly, when assessing atypical work, the portion of high-risk work should be taken into account after a proper work analysis. For upper limb disorders including the shoulder joint, RULA was used in 11 cases. RULA is considered as useful in evaluating inappropriate work postures considering the overhead position of the hands.
The Rapid Entire Body Assessment Tool (REBA) is an ergonomic tool that is used most frequently next to RULA. REBA, a work posture evaluation tool, was developed to complement RULA, which is limited to its coverage of the posture of the upper limbs. Lee et al. (2) reported that REBA was the most appropriate tool for evaluating systemic postures. The subjects showed an irregular work posture in all of the 17 cases that used REBA. All subjects worked in the manufacturing industry except for 1 subject working in a restaurant business and 1 subject working in the area of VDT. Interestingly, 14 cases of 17 were requested after 2007. This was thought to be the result of the COMWEL commencement of requests at the OSHRI that recognized the necessity of separate evaluations for work-relatedness for atypical work starting in 2007.
The Strain Index (SI) is a quantitative assessment technique for upper limb disorders originally developed at the University of Wisconsin (3). It calculates the SI as a product of the pinch/grip power, duration, frequency, posture, work speed, and working hours. Of 8 cases, it was used in 5 cases of the hand and wrist, 1 case of myofacial pain syndrome of the wrist muscles, 1 case of ganglion at the wrist, and 3 cases of carpal tunnel syndrome. In all of these cases, SI was used as a crucial basis of judgment for an ergonomic assessment related to the hand and wrist. One case involving the use of a Push/Pull gauge to measure shoulder joint stress was found that occurred in 2007. Judgment of excess stress on the joint may be important in some cases of disorders of the rotator cuff that include supraspinatus tendon rupture, abduction of the shoulder joint, the overhead position of the hand, and cases of repetitive movement. The Push/Pull gauge provided quantitative results for these excess forces.
For vibration measurements, there was 1 case involving a local vibration measurement and 5 cases involving systemic vibration measurements. The National Institute for Occupational Safety and Health (NIOSH) reported in 1997 that vibration was very closely related to hand-arm vibration syndrome and lumbar pain epidemiologically; however, it reported an insufficient epidemiologic basis for cervical pain. Of epidemiologic investigation cases, there were 2 vibration measurement cases of a ruptured cervical disk (1 case approved and 1 case unapproved), 1 case of lumbar disc herniation (approved), and 2 cases of combined ruptured cervical disk and lumbar disc herniation (1 case approved and 1 case unapproved). The jobs of the corresponding workers were taxi drivers, bus driver, forklift driver, crane operator, and rock drill operator. For local vibration, the formula provided by ISO 5349-1:2001(E) was used for the vibration exposure-effect assessment that evaluated whether the possibility of the occurrence of hand-arm vibration syndrome within the corresponding period exceeded the 50th percentile with mean vibration acceleration and exposure duration. For systemic vibration, the vector sum method and the Health Guidance Caution Zone from ISO 2631/1(1997) were used for the vibration exposure-effect measurement and evaluation. While the epidemiologic relationship between the vibration and the ruptured cervical disk was insufficient (for 1 approved case of a ruptured cervical disk) it appeared that the experience of a traffic accident (taxi) and the work posture were taken into account.
In addition to these tools, the OSHRI used for Ovako Working Posture Assessment System (OWAS), NIOSH Lifting Equation (NLE), American National Standards Institute (ANSI) Z-365, biomechanical loading analysis, surface EMG, and other similar tools that consider various work conditions and work environment conditions.
Work-relatedness evaluations of MSDs involve the consideration of various factors for each disease with different criteria for each case. It becomes necessary to consider many different factors and epidemiological evidence. The OSHRI approached these cases separately, according to each body part and disease. We examined the disease occurrence status in the report by the OSHRI (according to the neck, upper limbs, waist, and lower limbs) and searched for how to evaluate the work-relatedness aspects of each disease along with the applied epidemiological evidence.
There were 99 cases of neck and upper limb disorders out of the 163 cases. Investigated in more detail, the neck (40 cases), shoulder and shoulder joint (27 cases), and simultaneous involvement of the neck, shoulder, and upper arm (4 cases); while the wrist (11 cases), elbow (9 cases), upper arm (4 cases), hand (2 cases), and forearm (2 cases) were also noted. Of the neck disorders, the most common and second most common diseases were a cervical herniated disc (26 cases) and a cervical sprain (8 cases). The diseases that simultaneously affected the neck, shoulder, and upper arm were occupational cervicobrachial disorders, myofacial pain syndrome, and fibromyalgia. Shoulder disorders included 15 cases of rotator-cuff-related disorders and 4 cases of myofacial pain syndrome. Wrist disorders were composed 7 cases of carpal tunnel syndrome, 1 case of Kienböck disease, and 1 case of Preiser's disease. Among diseases of the elbow joint, lateral epicondylitis was the highest with 5 cases. Other diseases included benign focal amyotrophy, thoracic outlet syndrome, and Hand-Arm Vibration Syndrome.
A degenerative change of the disc by natural aging and degenerative changes precipitated by mechanical factors cannot be differentiated. Specifically, work-relatedness cannot singularly be determined by a diagnosis of disease, but by the level of the effect of which risk factors in the workplace can be attributed to harming the disc. Occasionally in the event of the findings of early degenerative changes that occur sooner than normal at the same age we can estimate such a clinical finding as work-related. It is reported that soft disc herniation may occur generally in the 30s-40s and that hard disc herniation may occur mainly in those over 50s. This herniation can be accepted as a work-related factor for this disease if some people suffer from one of these diseases before the age at which it occurs most commonly; however, degenerative changes of the cervical disc can be found asymptomatically in those in their 20s. It is also commonly found in those over age 50 and indicates that (apart from cases of prominent disc degeneration occurring before age 20) it may be that actual cases for which this logic can be applied to actual work-relatedness evaluations are rare.
From the 26 cases of a herniated cervical disc actually investigated by the OSHRI, the reasons for the investigation requests from COMWEL were analyzed. We found that out of 18 cases which were considered as grounds for an investigation request from COMWEL, requests of approval for 11 cases were rejected by the COMWEL committee on the grounds of degeneration by the natural aging of the disc and adjacent parts. For one of the cases, COMWEL presumed the worker to be exposed to an acceptable musculoskeletal burden; however, this case was also rejected due to the presumption of degeneration by natural aging. Instead of regarding the existence of a musculoskeletal risk factor for a worker (positive proof that such a progress could exist was a first-order priority) they gave greater priority to the MRI finding (negative proof that there can be no such progress). It remained the degeneration differentiation was an unsolved uncertain problem. We assumed it as a type of decision-making process problem. In 11 cases involving degeneration findings, the COMWEL committee mentioned a central protrusion of a disc, disc bulges, nucleus pulposus degeneration, degenerative spondylosis, and ossification of the posterior longitudinal ligament as degenerative changes caused by natural aging. They also considered 1 case of hard disc herniation by degenerative spondylosis occurring from natural aging. We found that the OSHRI had an agreement with the decisions of the COMWEL committee regarding degeneration by natural aging, but the actual decision-making process of the OSHRI was different from that of COMWEL. The OSHRI tended to choose degeneration by natural aging as the second valuable clue for decision in cases of without serious musculoskeletal burdens. However, in some cases of hard disc herniation and spinal stenosis when the subject turned over 60s, the OSHRI has also engaged in careful consideration of the aging effect on degenerative change.
Applying epidemiologic evidences of work-related factors associated with cervical disc herniation, the OSHRI has referred to literature from the NIOSH (1997) and has commonly applied findings related to repetitive movements and awkward positions of the neck (4). The report by Mayer et al. (5) has often been cited as the epidemiologic evidence used to show an increasing risk of cervical disc herniation due to neck extension. This report found that neck extension and overhead viewing while lifting the upper limbs increase the pressure on the C5-6 disc, ligaments, and adjacent structures. Cadaveric experimental studies of the effects on cervical discs with neck extension, studies of repetitive flexions, and extensions of animal necks have been cited as well (6, 7). As additional evidence, many investigators cited the results of a biomechanical study that found the disc pressure loading is (for instance) at the 4th and 5th cervical disc, 500-700 N while flexing and twisting and 1100 N while extending (8).
Abduction of the shoulder joint is mostly performed by the deltoid and supraspinatus. This is the basis for suspecting a high possibility of rotator cuff tendinitis or supraspinatus tendinitis and rupture when work involves abduction movement of the shoulder joint. In epidemiologic investigations, workers engaged in sewing work and similar workers who worked while repeatedly bending their back forward with overhead viewing action, were reported to have a high possibility of the occurrence of myofacial pain syndrome and rotator cuff tendinitis (9).
Degenerative changes of the subacromial mucous cyst and acromioclavicular joint are an essential prerequisite for the rupturing of the supraspinatus tendon, usually occurring at the ages between 45 and 65. Sher et al. (10) reported that MRI investigations in 96 subjects without shoulder joint symptoms showed rotator cuff damage in 34% of the subjects and the prevalence increased with age. Degeneration with natural aging may also precede work-relatedness evaluations of rotator cuff disorders and makes judgment difficult for work-relatedness evaluations of aged workers. There are two hypotheses regarding the mechanism of the rupture of the supraspinatus tendon: extrinsic factors and intrinsic factors. The extrinsic mechanism theory suggests that the wearing of the supraspinatus tendon progresses by repeated movement of the shoulder joint with the congenital morphology of the acromion or acquired morphologic changes such as degenerative osteophyte at the lower part of the acromion preceding. Bigliani classified subacromial morphology into 3 types and focused on the hook type as the main cause of a complete rupture. The intrinsic factor theory suggests that local ischemic lesions arise with a decreased blood supply at the direct surface onto which the supraspinatus tendon is inserted into the greater tubercle of the humerus. The decreased blood flow in this region causes degenerative changes of the supraspinatus tendon, calcification, and even rupturing (11, 12). Both mechanisms can be understood as musculoskeletal burden work that may promote the progression of a disorder.
The determination if a worker's job is a musculoskeletal burden that may cause shoulder joint degeneration is important for work-relatedness evaluations. Of the 15 cases of rotator cuff disorders by the OSHRI, work-related loading was seen as promoting shoulder joint degeneration in 10 of 11 approved cases. In another case, work-relatedness was even approved in an aged worker who was assumed to have considerably progressed degeneration, considering that their fragile supraspinatus muscle was exposed to intensive shoulder stress during a short time.
The number of lumbar disorders was 44 cases out of 163 diseases. Herniated lumbar disc was noted in 29 cases and lumbar sprain was noted in 8 cases (with spondylolisthesis comprising 3 cases).
Herniated lumbar disc also occurs by natural degeneration and occupational degeneration that cannot be differentiated by clinical radiological tools. Boden et al. (13) reported 67 subjects without symptoms who had an MRI taken. A total of 54% of those under age 60 and 79% of those over age 60 had at least more than one level of a bulging disc. A total of 34% of the group in their 20s to 30s, 59% in their 40s to 50s, and 93% in their 60s to 80s had more than one degenerative disc. A total of 21% in their 20s to 30s, 22% in their 40s to 50s and 36% in their 60s to 80s had more than one herniated disc. Spinal stenosis was noted in 21% of those in their 60s to 80s.
The evaluation basis for a herniated lumbar disc stemming from work-related stress was similar to that of a cervical herniated intervertebral disc. The OSHRI regards it important to make a clear diagnosis and if the work is a waist burden work. Even if there is suspicion of a bulging disc, if the symptoms for lumbar neuropathy match those stipulated by NCV/EMG, the diagnosis of a herniated lumbar disc could be acknowledged and a work-related evaluation should be done. Occupational factors that cause stress on the waist as mentioned in NIOSH (1997) are heavy physical work, lifting and forceful movements, bending, twisting, awkward postures, whole-body vibration, and static work postures.
Lower limb disorders numbered 18 of 164 diseases; knee joint disorders (6 cases), hip joint disorders (6 cases), feet disorders (4 cases), and calf disorders (2 cases). Of diseases that are related to the knee joints, 6 involved a meniscus tear. There were 6 hip joint disorders involving avascular necrosis of the femoral head. For foot disorders1 case of hallux valgus and 1 case of tendinitis of the foot. One was injury to the soft tissues and one was plantar fasciitis. Calf disorders included 1 varicose vein case and 1 case of cellulitis.
Meniscus cartilage is biomechanically known to absorb shock. It is related to movement delivery, lubrication, and protects the knee joint. It serves an important function as it lessens the weight going to the tibia and decreases the stress rate. It also protects the joint cartilage and stops degenerative arthritis (14).
Regarding work-relatedness evaluations of meniscus injury, the criteria are different depending on if the affliction occurred due to a rapid accident or it was a chronic symptom simply realized by chance. If it started at an early age in an acute manner, a meniscus injury usually has appears as a longitudinal tear or an oblique tear. On the other hand, horizontal tears happens regularly in middle-aged adults and (unlike different types of tears) there is no special injury on the outside or only a slight injury, usually accompanied with degenerative changes of the tissues around it. Because the injury on the outside is unidentifiable and because the degenerative changes are commonly found during the diagnostic test, it is reported that the meniscus tears have more to do with degenerative arthritis of the knee joint. Research in 1998 shows that 61.7% of the people were blue-collar workers, 14.7% office workers, and 14.7% housewives (15). According to Smillie (16), an individual might not notice a slight tear in the cartilage that will eventually grow larger because of constant irritation. This tear will eventually lead to degenerative changes and seeing the level of rupture reach that of a functional disorder (16). A complex tear and a horizontal tear (compared to other types of tears) involve a change in the degeneration of the cartilage. These can lead to serious problems (17).
In the epidemiologic research conducted by the OSHRI, 4 cases were approved and 2 were rejected among 6. All 6 of the cases involved damage inside the knee joints. A total of 2 out of the 4 unapproved cases were declared to have occurred after the tear of the knee joint, because a horizontal tear does not normally occur (except for instances of rapid trauma) and because the job did not affect the knee joints very much. The other case was a male who declared the disease after working for 3 yr. This case involved a vertical tear that could not have happened in three years and implied that the tear was a pre-existing work condition. Therefore, the case was not approved as it was deemed not work-related. The last case was a person who had worked for 25 yr, but because the work of the claimant did not place stress on the knee, it was deemed not work-related. The 2 cases that were approved were a 55 yr old man who was a welder (employed for 22 yr) and a 48 yr old painter. They each had a vertical tear coming from the accumulation of small tears. This case was approved because they worked stressing the knees while squatting and kneeling. There was no absolute evidence that the squatting and kneeling position had a direct correlation with the knee joint tears; however, reports of knee pain coming from kneeling (18) and squatting are more common in people working in the ship building industry (19, 20). Many of these individuals show degenerative arthritis and knee joint cartilages tear relationships, with a squatting and kneeling position causing injury to the meniscus (21-23). However, this type of assumption can easily be turned around and implies that more evidence must be collected.
Looking at the reports of the OSHRI, we found that some consistent principles were applied. In the case of gender, though it was not statistically significant (P=0.14), women have more benefit than men. It appeared that females can be considered as a group vulnerable to musculoskeletal risk factors. The criteria that regarded the interpretation of ergonomic assessment tools were stricter for women than men owing to the discrepancy in physical ability between males and females. In the work-relatedness decision process, special regard might be made in consideration of physical ability.
According to age, it is possible that humans may be vulnerable to musculoskeletal risk factors owing to weakness of the physical function and degeneration caused by natural aging. In Korea, there is some debate whether the acceptable musculoskeletal burden for young workers in 20s and 30s is regarded as a considerable causal factors for workers 40 or older with consideration of the vulnerability due to simply an existing weak physical status caused by natural degeneration. The result of the OSHRI data shows that those in their 30's have some advantages in the evaluations of work-relatedness; however, the approval rate gradually decreases after age 40. This showed that younger groups are in a more advantageous position regarding the evaluations of WMSDs compared to older groups.
We presume that there is another in regards to the difficulty of differentiation between degeneration by aging and musculoskeletal burdens. Individuals can assume that the longer a worker is exposed to mechanical factors, then the higher approval rate. The result of the exposure time analysis showed the approval of MSDs is somewhat appropriate in regards to the concepts of age and duration of exposure. If the duration of exposure is less than one year, this has a negative effect on the diseases occuring that require a longer time for cumulative exposure. Adversely, an effect of an excessively long time of exposure overlaps with the effects of aging. The OSHRI seemed to create a solution of this problem from the ergonomic analysis. The result of ergonomic analysis was almost crucial to determine the work-relatedness. A total of 71 of 79 approved cases were confirmed to be exposed to considerate musculoskeletal burden by ergonomic analysis. Considering the difficulty of the differentiation between natural aging and degenerative changes precipitated by mechanical factors, this may be the best way to handle the situation. Someday, we will also ask for measuring and comparing an aging effect with musculoskeletal burden quantitatively in order to evaluate work-relatedness through further studies.
According to the anatomical classification, neck and upper limb disorders showed the highest approvement percentage. On the other hand, low approval rates of lower limb disorders were observed. This result was assumed to be largely affected by four cases of avascular necrosis of the femur head, which were claimed to have a trauma-induced origin. It is not common for trauma only, not resulted in a fracture, to be approved. In another hypothesis, we can assume that there is not enough epidemiological evidence of lower limb disorders as well, and we can also presume the difficulty of ergonomic analyses in the lower limbs.
WMSDs in Korea based on worker's compensation statistics reached the peak in 2003 or in 2006 when accidental low back pain was included as a type of WMSDs, and we found it to indicate the trend of a gradual decrease. However, cautious judgment must be made regarding whether any other external factor contributed, as this data only represents the total number of the approved worker's compensation cases. In the case of Europe, WMSDs has occupied 49% of the causes of absenteeism, and 100 million workers suffered WMSDs. Especially, in Sweden, WMSDs took up more than 57% of occupational diseases. In America, the proportion of WMSDs by repetitive movements was 33.6% in 1992. It peaked at 34.7% in 2000. In 2007, it decreased to 28.9% by various measures. In the case of Korea, the proportion of WMSDs in total occupational diseases continuously increased. Especially, the rapid increase mainly occurred in workplaces with over 1,000 employees and the social issue of labor-management disputes was on the rise. In addition, the expense of the compensation insurance was 5.9 billion won in 2000 that became 105.3 billion in 2004 and 163.3 billion won in 2007. This data shows the considerable social expenses of WMSDs.
Another issue of WMSDs is the approval rate. Some expert groups insisted that the continual decrease of the approval rate for WMSDs has been observed from 2006 to 2009. There is no official report of COMWEL about the approval rate of WMSDs; however, we found a report of total accepted cases of worker's compensation insurance for MSDs. It reported that the accepted cases increased with 4,298 cases in 2006, 3,485 cases in 2007, 3,885 cases in 2008 and 5,853 cases in 2009. However, the unapproved cases increased with 1,416 cases (32.9%) in 2006, 1,557 cases (44.7%) in 2007, 1,650 cases (42.5%) in 2008, and 2,710 cases (46.3%) in 2009 (24).
Most cases of epidemiological investigation by the OSHRI were consulted by the request of claimant due to the decision to deny in the first or second deliberation by COMWEL. Thus, the data of the OSHRI includes the probability of a selection bias and it is difficult to consider that this data can satisfy the statistical representativeness. The OSHRI data showed a 65.6% approval rate and a previously mentioned report of worker's compensation records showed a similar level of the approval rate that ranged from 54% to 67% from 2006-2009. However, the OSHRI data were intentionally selected among unapproved cases and all of the unapproved cases were not referred to the OSHRI; therefore the cases of the OSHRI occupied only small proportion of the total cases of WMSDs.
Assuming the high difficulty of their population referred to the OSHRI, it could show different outcome if every accepted cases were referred to an OSHRI epidemiological investigation. The OSHRI decision of approval means the first determination will be reversed, a 65.6% approval rate has over 50% of discrepancy by the expert's interpretation of work-relatedness by COMWEL and the OSHRI. When applying the compensation approval criteria for WMSDs, there have been perceptional gaps between the expert groups in Korea that influenced the work-relatedness evaluation. If this is so, where does these perceptional gaps stem from? At present, the work-relatedness evaluation of MSDs by COMWEL was conducted on many cases in a relatively short-time by a committee and therefore it could be easy that simple contextual information and the radiologic findings were used only limitedly (25). Unfortunately, a degenerative change by natural aging and by mechanical factors cannot be differentiated only by radiologic imaging. If there was not enough data for ergonomic analysis, the committee had to judge with incomplete information about a case that could result in the under or overestimation of work-relatedness.
On the other group of this interpretation, in the qualitative review of the reports by the OSHRI, we suspected that the OSHRI has a hierarchical relationship which was a priority for the results of ergonomic analysis more than age. In addition, we also found the trend of a dependency on the result of ergonomic analysis even though there was obscure judgment of a hierarchical relationship between age and ergonomic analysis. However, COMWEL shows a significant difference of the interpretation of priority. This difference may be interpreted as whether or not additive information of the work environment exists or we can presume a deficiency in the mutual exchange on the information of the interpretation of work-relatedness.
The equality of opportunity is universally important and we think that the present worker's compensation system has a significant defect in the ability to classify work-relatedness issues. For solving this problem, we try to guarantee the epidemiological investigation that includes ergonomic analysis in all unapproved cases and we try to form a consensus among experts about this subject. For that goal, we must start to introduce a training system that can evaluate work-relatedness issues. Simultaneously, we need to evolve the quantitative explanations for the attributions of musculoskeletal burdens.
Figures and Tables
References
1. Kim DS, Park JK, Kim KS. A study for the efficient implementation management through the evaluating effectiveness of a WMSDs prevention program. 2009. Occupational Safety and Health Research Institute.
2. Lee IS, Chung MK, Choi KI. Comparison of observational posture evaluation methods based on perceived discomfort. J Ergon Soc Korea. 2003. 22:43–56.
3. Moore JS, Garg A. The Strain Index: a proposed method to analyze jobs for risk of distal upper extremity disorders. Am Ind Hyg Assoc J. 1995. 56:443–458.
4. Putz-Anderson V, Bernard B, Burt S, Cole L, Fairfield Estill C, Grant K, Gjessing C, Jenkins L, Hurrell J, Nelson N, Tanakan S. Musculoskeletal disorders (MSDs) and workplace factors: a critical review of epidemiologic evidence for work-related musculoskeletal disorders of the neck, upper extremity, and low back (2nd printing). 1997. Cincinnati, OH: U.S. Department of Health and Human Services (DHHS);Available at http://www.cdc.gov/niosh/docs/97-141/pdfs/97-141.pdf.
5. Mayer TG, Gatchel RJ, Polatin PB. Occupational Musculoskeletal Disorders: Function, Outcomes, and Evidence. 2000. Philadelphia: Lippincott Williams & Wilkins.
6. Farmer JC, Wisneski RJ. Cervical spine nerve root compression. An analysis of neuroforaminal pressures with varying head and arm positions. Spine. 1994. 19:1850–1855.
7. Callaghan JP, McGill SM. Intervertebral disc herniation: studies on a porcine model exposed to highly repetitive flexion/extension motion with compressive force. Clin Biomech (Bristol, Avon). 2001. 16:28–37.
8. Moroney SP, Schultz AB, Miller JA. Analysis and measurement of neck loads. J Orthop Res. 1988. 6:713–720.
9. Kaergaard A, Andersen JH. Musculoskeletal disorders of the neck and shoulders in female sewing machine operators: prevalence, incidence, and prognosis. Occup Environ Med. 2000. 57:528–534.
10. Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995. 77:10–15.
11. Hagberg M. Arbetsmiljöns betydelse för besvär i skuldra och halsrygg. 1990. Uppsala: Ord & Form.
12. Riand N, Levigne C, Renaud E, Walch G. Results of derotational humeral osteotomy in posterosuperior glenoid impingement. Am J Sports Med. 1998. 26:453–459.
13. Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990. 72:403–408.
14. Stone RG, Frewin PR, Gonzales S. Long-term assessment of arthroscopic meniscus repair: a two- to six- year follow-up study. Arthroscopy. 1990. 6:73–78.
15. Cho SD, Shin DB, Cho YS, Park TW, Kim YK. Horizontal tear of the meniscus. J Korean Orthop Assoc. 1998. 33:1737–1742.
16. Smillie IS. Injuries of the knee joint. 1978. 5th Ed. New York: Churchill Livingstone.
17. Christoforakis J, Pradhan R, Sanchez-Ballester J, Hunt N, Strachan RK. Is there an association between articular cartilage changes and degenerative meniscus tears? Arthroscopy. 2005. 21:1366–1369.
18. Cozzensa da Silva M, Fassa AG, Rodrigues Domingues M, Kriebel D. Knee pain and associated occupational factors: a systematic review. Cad Saude Publica. 2007. 23:1763–1775.
19. Park BC, Cheong HK, Kim SK. Risk factors related to musculoskeletal symptoms in shipyard workers. Korean J Occup Environ Med. 2003. 15:373–387.
20. Kim I, Koh SB, Kim JS, Kang DM, Son M, Kim Y, Song J. The relationship between musculoskeletal symptoms and job stress & intensity of labor among shipbuilding workers. Korean J Occup Environ Med. 2004. 16:401–412.
21. Jensen LK, Mikkelsen S, Loft IP, Eenberg W, Bergmann I, Løgager V. Radiographic knee osteoarthritis in floorlayers and carpenters. Scand J Work Environ Health. 2000. 26:257–262.
22. Cooper C, McAlindon T, Coggon D, Egger P, Dieppe P. Occupational activity and osteoarthritis of the knee. Ann Rheum Dis. 1994. 53:90–93.
23. Coggon D, Croft P, Kellingray S, Barrett D, McLaren M, Cooper C. Occupational physical activities and osteoarthritis of the knee. Arthritis Rheum. 2000. 43:1443–1449.
24. IM SH. The changes of the approved rate before and after introducing occupational disease award commission to industrial accident compensation insurance system. OSH Res Brief. 2010. (10):8–11.
25. Lee CY. An occupational medicine specialist's point of view, who has participated in occupational disease award commission in Korea worker's compensation and welfare service. OSH Res Brief. 2010. (10):12–17.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download