Abstract
Occupational infection is a human disease caused by work-associated exposure to microbial agents through human and environmental contact. According to the literature, occupational infection was the third leading cause of occupational disease (861 cases, 8.0%), and health care, agricultural, forestry, and fishery workers were risk groups in Korea. In addition, most high-risk groups have not been protected by workers' compensation, which could lead to underestimation of the exact spectrum and magnitude of the problem, and may also result in a lack of development and implementation of occupational infection management. Through a review of national guidelines and documentations on prevention and control of occupational infection, a management strategy would promote adherence to worker safety regulations if it is explicit with regard to the agent and mode of infection in each of the high-risk groups.
Occupational infections are human diseases caused by work-associated exposure to microbial agents, including bacteria, viruses, fungi and parasites (helminthes, protozoa) (1). Although occupational infections can involve several organ systems (e.g., respiratory, enteric, and skin), unique characteristics differentiate them from other occupational disease with regard to the source of exposure, epidemiologic control, and prevention. Transmission involves a variety of routes in particular work environments (2).
Because of the characteristics of infections, prevention of occupational infection depends primarily on defining risky occupational practices or environments and developing a suitable practice policy fit for each causative agent. Among the general population, infectious disease risk should never be ignored, as it is a major public health issue. According to the national death registry in Korea (2008), infections, including tuberculosis, accounted for 11.3% (tuberculosis 4.3%) of total deaths (3). In 2005, the proportion of viral hepatitis B carriers was 3.7% of the total population, as reported by the Korea National Health and Nutrition Examination Survey (4). Since most people have been frequently exposed through person-to-person contact at workplaces, occupational infection risk could be a more serious issue than ordinary infections in public health, especially communicable diseases. However, the proportion of work-relatedness of infectious disease in the population has not yet been established in Korea.
The purpose of this literature review was to find out the epidemiology of occupational infections in Korea and assist medical practitioners and other stakeholders in establishing and promoting adherence to policies and management plans for not only general occupational infection, but also to focus on high-risk groups.
To understand characteristics of occupational infection in the workers' compensation database, annual reports published as 'The survey on the cause of occupational injuries and diseases' by the Occupational Safety & Health Research Institute (OSHRI) of the Korea Occupational Safety and Health Agency (KOSHA) were reviewed. The survey was approved based on the Statistics Act (approval no. 38001). Based on these data, 10,619 occupational disease and 44,501 work-related disorders in total during 9 yr between 1 January 1999 and 31 December 2007 were collected. Among them, 851 cases (8.0%), including 22 deaths (0.2%), were approved as occupational infections. The distribution of general and occupational characteristics of occupational infections, such as sex, age group, infectious agent or mode, working duration, industry and job type, were also determined.
After highly prevalent job types and industries were collected from the workers' compensation database, several review articles regarding cases from high-risk groups, such as health care, agricultural, forestry and fishery workers in Korea were also examined. A literature search was carried out using Medical Library Information System (MEDLIS), Korean Studies Information System (KISS), National Assembly library and web of science databases with the following key word combinations: "Occupational infectious disease", "Occupational infection", "Korea", "Communicable disease", "work-relatedness", "occupational exposure", "Blood-borne infection", "health care worker", "hemorrhagic fever", "viral hepatitis", "tuberculosis", "zoonosis". Snowball sampling was carried out with scanned articles. All of the articles were limited to Korea. Guidelines and documentation on the official websites of KOSHA, the Ministry of Employment and Labor of Korea (MOEL), the Ministry for Health, the Welfare and Family Affairs and the Rural Developmental Administration. Additionally, a review of guidelines for preventing and controlling occupational infection at work, not only in general workers but also in high-risk groups, and guidelines for specific infectious organisms and environments were carried out.
According to annual reports published from 1999 to 2007, 55,120 cases of work-related illness, including 10,619 cases of occupational disease and 44,501 cases of work-related disorders, were documented (5-12). Occupational infection (851 cases, including 22 deaths) comprised 8.0% of all occupational diseases and 1.5% of work-related illnesses in that time period. Occupational infection was found to be the 3rd most common occupational disease. In addition, the absolute number of compensated cases in 2007 (159) increased more than twofold from 1998 (66 cases).
The 851 cases (8.0%) of occupational infectious diseases, including 22 deaths (0.2%), approved as occupational disease were further analyzed. The number of annual compensated cases with occupational infection has been rising since 2000: 113 cases in 2006 and 159 cases in 2007.
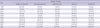
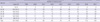
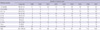
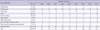
During the 9-yr time period, female workers accounted for 513 cases (60.3%) of compensated cases (Table 1). The most common age group was 20-29 yr old (294 cases, 34.5%) (Table 2). The most frequent disease was tuberculosis (283 cases, 35.8%), followed by scrub typhus (280 cases, 35.4%) and viral hepatitis (44 cases, 5.6%) (Table 3).
In the period, infection was the most frequent compensated occupational disease in workers employed less than 3 months (182 cases, 21.4%), followed by those employed between 6 months and 1 yr (105 cases, 12.3%) (Table 4). The most common type of industry was public administrative, health care, and education service sectors (520 cases, 61.1%), followed by agricultural, forestry, and fishery sectors (82 cases, 9.6%) (Table 5). The major type of occupation was professional (347 cases, 39.2%), followed by unskilled laborer (264 cases, 31.2%) (Table 6).
A focused review of occupational infection in health care workers from the workers' compensation database was performed (13). From January 1998 to December 2004, 307 cases of compensated occupational infection were collected. The most common cause of infection was tuberculosis (219 cases, 71.3%), followed by viral hepatitis (43 cases, 13.7%). The major type of occupation was nurse (223 cases, 72.7%), followed by doctor (37 cases, 12.1%). The most common working duration was 1.0-5.0 yr (164 cases, 53.4%) and the most common age group was 20-29 yr old (228 cases, 74.3%). The most common size of the enterprise was 500-900 workers (91 cases, 29.6%). The majority of working place of hospital were from inpatient wards (161 cases, 52.4%), followed by intensive care units (51 cases, 16.6%). The result showed that the highest risk group for occupational infection in the health care sector was female nurses of reproductive age. Therefore, the importance of prevention in high-risk groups for health care-related occupational infection should be stressed. Moreover, this article could elucidate the variety of occupational infection, not only the majority of health care-related infection, such as tuberculosis and viral hepatitis, but also infections through contact or airborne transmission (e.g., measles and meningitis).
In addition, a surveillance project for preventing needle stick injury (NSI) was initiated for health care workers since the 1990s. This project was funded by OSHRI and consisted of 10 university hospitals with web-based voluntary reporting systems for 3 months in 2009.
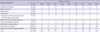
The incidence of NSI was 10.6 cases per 100 inpatients-bed per year and 4.1 cases per 100 workers per year in the surveillance system for NSI (Table 7) (14). Additionally, the experience rate of NSI in health care workers was 51.2-96.7% according to other studies in Korea (15, 16). The crude incidence rate for work-related blood-exposure was 2.6 cases per 100 workers in a study performed at a university hospital in Korea (17). Estimated incidence of NSI in 36 Korean hospitals was 6.1 cases per 100 beds and 3.0 cases per 100 workers in 1 yr (18). Even though the indices of incidence differed between the surveillance project for NSI and the other studies, risk factors for NSI were similar.
Health care workers have also experienced latent tuberculosis by exposure to the pathogen in hospitals. One study examined changes in the tuberculin skin test and the QuantiFERON-TB Gold assay before and after treatment for latent tuberculosis in health care workers at a local university hospital. Among 48 participants (14 doctors, 34 nurses), test-results were positive as markers of latent tuberculosis in 25-39.6% of study subjects respectively (19). A prevalence ratio for latent tuberculosis in health care workers compared with the general population was calculated. Tuberculosis occurred in 61 (0.72%) of 8,433 newly employed health care workers over a 6-yr period. The prevalence ratio was calculated by dividing the number of observed tuberculosis cases in health care workers by the number of tuberculosis cases in the general population in Korea. The prevalence ratio among all health care workers was 1.05 (95% CI 0.80-1.35) (20).
Studies by Ahn and Lim (21) analyzed occupational disease in farmers according to the workers' compensation database. In the 8 yr from January 1998 to December 2005, 10,734 cases of compensated occupational diseases in agricultural, forestry, and fishery workers were collected from 608,449 workers. There were 131 cases of occupational infection, including 24 cases in agricultural workers and 107 cases in fishery workers. The most common cause of infection (123 cases) was rickettsial disease known as scrub typhus (tsutsugamushi disease) (22). The majority of data was from workers below 6 months after employment and those over 50 yr old.
Trends in transmission and epidemics of infection are a mirror of the times (23). Moreover, the socio-economic status of the general population is a factor for occupational infection.
Korean military personnel have been a suggested at-risk group for endemic infectious disease. From 1995 to 1997, a case report was written for vaccinations and chemoprophylaxis against malaria given to UN peacekeeping forces operating in Angola, Western Sahara, Georgia, India, and Pakistan (24). Vaccinations included those for yellow fever, hepatitis, tetanus, diphtheria, typhoid fever, polio, meningococcal meningitis, influenza, measles and immunoglobulin. In contrast, malaria chemoprophylaxis was administered 6 weeks after returning to Korea (25).
From 1977 to 1981, cases of medical injury and illness were 1,049 in total from all travelers returning from Middle-East, as reported by the medical clinic in International Airport in Korea (26). Cases of injury and illness in business travelers increased from 102 in 1997 to 303 cases in 1981 (27). A questionnaire-type survey was conducted on 357 business travelers working for 5 construction companies in the Middle East, including Jordan, Egypt and Sudan, in 1984. Among infectious diseases classified as 'tropical disease', the most common were malaria (112 cases, 52.8%) and leishmaniasis (19 cases, 9%) (28). A more updated report based on the national reporting system in Korea found 73 cases of occupational infection in business travelers in 2002 and 110 cases in 2004 (29).
Recently, the main issue has been the socio-economic status of those in the service sector, and it is also a concern in occupational medicine. Workers' compensation cases in the service sector rose from 29% of the total number of compensation cases in 2002 to 37% in 2008. In previous reviews of workers' compensation annual reports, the service industry accounted for the majority of cases (684, 80.3%), including the subcategories 'public health & education', 'recreational, cultural and sporting activity' and 'real estate & leasing business'. Several case-series reports from service sectors providers have been published and included in this review. Service sector workers, such as veterinarians, researchers, and animal trainers or keepers, are known to be vulnerable to zoonoses. A case of hemorrhagic fever with renal syndrome occurred in a researcher, with the suspected cause being laboratory-acquired Hantavirus infection. Among 218 laboratory workers tested, 7 were serologically positive for Hantavirus. In the same study, the association between exposure to animals in the workplace and a serologic-positive result was significantly strong (OR 19.68, 95% CI 1.11-350.40) (30).
The index case for zoonosis from a fungal infection with Microsporum canis was a person employed to dance with tigers. Among 16 cases in total, 14 had direct contact with a tiger while 2 were indirectly infected by co-workers (31). In addition, a fungal infection with Microsporum canis in a horse keeper was reported (32). Bovine-associated brucellosis was first reported in 1955, and has risen to 25,454 cases in 2006 (33). A prevalence rate of 2.18 per cattle marks it as the most emerging risk of occupational infection.
In 1993, the Occupational Safety and Health (OSH) Act had legislated to maintain and protect the health of workers and prevent potential workplace health hazards in Korea. Regular checkups for occupational disease, known as Special Health Examination, and Work Environment Monitoring would benefit workers. Unfortunately, biological risk factors at work have been excluded from the application of the examination and the monitoring (34).
Even though few regulations and work standards for specific pathogens or industries group exist, a few guidelines for occupational infection have been recently developed by government agencies. The first set of guidelines, named as the KOSHA-code, dealt with prevention and protection against NSI, the most vulnerable mode of exposure to occupational infectious agents. The KOSHA-code, 'Guideline for preventing of injury for needle stick and sharp vehicles in health care workers' was established for employers and employes by KOSHA, the administrative and supportive organization under MOEL, and it was the first set of guidelines for health care workers in Korea (35). Preventive measures, accident management plans, and worker education strategies were detailed. The record format for verification of needle stick injury, flow chart for injury and accident, and check-up list for handling sharp instrument around injection were provided.
Guidelines for prevention of pandemic flu (H1N1 influenza) were recently established due to societal pressure. These guidelines focused on plans for business continuity during pandemics and established by cooperation between the Ministry of Employment and Labor, responsible for worker's health, and the Ministry for Health, Welfare and Family Affairs, responsible for public health care and infection control (36). In summary, these guidelines consisted of infection control for pandemic flu and a business continuity plan (BCP) in the workplace. The guidelines' greatest strength is the wide spectrum of their applicability. For example, the reporting format for those who have contracted pandemic flu in the health care workplace and a checklist for management and promotion of infection control in the workplace according to each national alert level for pandemic flu were provided in this set of guidelines.
Through this review, occupational infection was revealed to be the 3rd most common compensated occupational disease (851 cases, 8.0%) in Korea in the most recent years (1999-2007). The number of annual compensated cases of occupational infection has risen since 2000. In that 9-yr period, compensated occupational infections were most frequent in workers employed for less than 3 months (182 cases, 21.4%).
Cases diagnosed as occupational infection and covered under workers' compensation were classified as 'the disorder caused by biological agent' in international statistics on occupational injury and illness. Because of differences in classification, a global consensus on the magnitude and spectrum of infectious diseases in occupational disease has failed to materialize. In 2008, occupational disorders caused by biological agents in Japan accounted for 2.9% (257 cases) of the total number of occupational injury and illness (8,684 cases) (37). The Ministry for Health, and Welfare in Korea noted a similar trend in occupational infection. Among all occupational illnesses (2,432 cases) in 2008, excluding industrial accident-related illnesses (6,252 cases), cases of occupational infection accounted for 10.6% of the total in Japan. According to the Finnish Register of Occupational Diseases, 134 cases (2.0%) of occupational infection out of 6,715 recognized and suspected cases of occupational disease occurred in 2006 (38). In 2009, work-related infection accounted for approximately 3% of work-related health problems in 28 EU countries, according to Euro-stat (39). In the USA, occupational infections were not classified as infectious disease, but instead as non-fatal occupational injury and illness. However, problems arise when making direct comparisons of occupational health statistics between countries because of differences in reporting procedures and how work-related injury and illness are compensated.
Despite the limitations of workers' compensation statistics, the increasing trend of compensated occupational infection has been evident since 2000. With regard to infection source (Table 3), the rising trend of scrub typhus may reflect the overall increase in total occupational infection. Along with this result, there is a rising trend of cases in the agriculture and forestry sectors. We collectively estimated exposure-scenarios of farmer and forestry workers exposed to mites and reported work-related scrub typhus.
Cases of occupational infection in 2007 (159 cases) were more frequently reported than in 2006 (113 cases). Intestinal tract infection (17 cases) and dermal fungal infection (17 cases), which had hardly been reported in the past, had surged in 2007 (Table 3). Moreover, incidence according to industry type (clerk, 21 cases) and time-duration after employed (0.5-1 yr) peaked in 2007. An overview of all available statistics for 2007 suggested an increase in occupational infection, such as food-borne illness. In the 9-yr period covered by this review, compensated occupational infection was most frequent in workers employed less than 3 months, with the exception being 2007. Regardless of working characteristics, all newly employed workers should be educated in maintaining safety and health in the workplace. Even if case numbers are collated in annual reports without an actual analysis of the data, the number of compensated cases showed a trend, and the epidemiology of occupational infection should be an essential consideration for control and management of occupational disease.
This review had several limitations. First, even though categorization according to the cause of industrial accidents was validated, the spectrum of categories was too broad to verify the actual pathogen according to occupational subgroup. Secondly, statistics from the workers' compensation database showed only a part of the actual burden of occupational infection. Much of the information on groups at high-risk of occupational infectious disease was controlled by MOEL. The distribution of workers' compensation coverage was heterogeneous according to the spectrum of regulation, even among the same functional groups in Korea. Since high-risk groups have been legally unprotected, the validity and effectiveness of statistics-based on workers' compensation is tenuous. Underestimation for policy-making and interventions to decrease risk of exposure could be raised. Therefore, a broad approach should be considered encompassing social- and academic-based issues for high-risk groups, as well as provision of training and equipment.
Fortunately, a national surveillance system for health care workers, especially for NSI, has been initiated with public funds. A national surveillance of agricultural workers was also implemented in terms of prevention of injury or intoxication. However, occupation-related epidemics from each surveillance system cannot displace official workers' compensation statistics. A national surveillance system with a broader spectrum, including agricultural, fishery, and forestry workers, is needed.
In cases of data from the Korean surveillance system for NSI, the incidence was 10.56 cases per 100 inpatients-bed per year and 4.07 cases per 100 workers per year. These were significantly lower values than from statistics in the US such as the National Surveillance System for Healthcare Workers (NaSH) (30 cases per 100 beds) (40) and Exposure Prevention Information Network (EPINet) (28.8-40.0 cases per 100 beds) (41). The prime issue when studying occupational infection in health care workers was representativeness. Further analysis was needed in not only compensated data coverage from IACI, but also other types of compensated data coverage from private educational pensions, which was covered by 10 university hospitals in Korea. The addition of more hospitals to its reporting network would further strengthen the NSI surveillance system. Along with these results, health care workers have experienced latent tuberculosis due to exposure in hospitals. An analysis of the workers' compensation database for occupational infection in health care workers was performed. During 7 yr, 307 cases of compensated occupational infection were collected. The most common cause of infection was tuberculosis (219 cases, 71.3%). In addition, latent tuberculosis was evaluated. The prevalence ratio among all health care workers was 1.05 (95% CI 0.80-1.35) in a university hospital. Further studies of tuberculosis should be conducted because the burden of tuberculosis is high in the general population in Korea. After identifying epidemics in health care workers, focused prevention and management should be performed in high-risk groups.
Through analysis the workers' compensation database, 131 cases in total including 24 cases of agricultural workers and 107 cases of fishery workers was analyzed. The most common cause of infection is rickettsial disease known as scrub typhus, which accounted for 123 cases. It was revealed that most of the actual cases of scrub typhus in agricultural workers could be underreported in statistics of compensated occupational disease. Because most agricultural workers have been engaged in self employed-business or unskilled laborers in Korea, they were almost beyond the criterion for coverage from workers' compensation. In addition, these analyses were preliminary and have not been adjusted for potential confounders.
From a management standpoint, social concern for disease is important, as well as the frequency and severity of disease. Especially in the case of infection, trends in transmission and epidemics of infection may reflect trends in the socio-economic status of the general population.
In the past, Korean military personnel have been suggested as being at risk of exposure to endemic infectious disease. However, recent trend of globalization has led to an increase in business travelers instead of expeditionary forces. According to the national reporting system, infection while abroad increased approximately 2-fold in 2004 over a 2-yr period. The alleviation of risk of infection and demand for infection control could be shared by both occupational medicine and public health.
Workers in service sectors, such as veterinarians, researchers, and animal trainers or keepers are vulnerable to biological hazards, termed 'zoonosis'. Sentinel cases for zoonosis, such as hemorrhagic fever with renal syndrome in animal research and fungal infection in animal caregivers, showed us how the actual risk of zoonosis could be concealed in practice. Another potential sentinel case could be brucellosis due to the exponential increase of bovine brucellosis in Korea. Finally, sewage or waste handlers should be considered as a high-risk group for exposure to biological hazards. Since most waste handlers are self-governed with respect to workers' compensation, most cases of infection have been concealed. There are several 'blind spots' for official statistics on occupational infection. Workers in the funeral industry should be considered as one emerging risk group for occupational infection from corpses. Even though funeral service providers share risk of transmission with health care workers, national statistics for conditions of funeral service providers have not been recognized yet. A thesis on the risk of exposure in funeral service providers was reported, with special focus on the embalming of corpses was reported once in Korea, but it was not for public health but for economic perspective (42).
Through the review of current guidelines, the main considerations found were standard precautions, attitude/behavior against contact with pathogen, vaccination, and PEP. Promoting blocking of transmission against pathogens, vehicles, and carriers should be the main focus for prevention of infection at work (43).
Therefore, the application of primary prevention should be recommended and verified for specific characteristics of exposure for each agent and mode of infection. International trends have emerged regarding specialized agents or hosts at risk. For instance, US NIOSH has provided a national protection plan and agenda for two independent agents categorized as 'blood-borne infection' and 'infectious aerosol' (44). The focus of future plans for prevention and control of occupational infection should be verified and applied in each high-risk group for occupational infection with a global perspective.
Recently, the main challenges for government have been being focusing on each high-risk group. However, most high-risk groups for occupational risk of infectious disease are beyond the scope of MOEL in Korea. Health care, agricultural, fishery and forestry workers, and waste handlers are considered 'blind spots' when dealing with workers' compensation. The combination of under-reporting of occupational disease in national statistics and lack of concern from the organizational system for occupational disease can result in the responsibility for prevention and control of infection being a personal burden. This could lead to the weakening demand for policy-making and reduction of obligation for risk control interventions. Therefore, a broader approach should be considered that encompasses social- and academic-based issues for high-risk groups, including the practicalities of training and equipment availability.
Because most infectious diseases are preventable through behavioral changes, prevention of exposure to infectious sources should be encouraged through education and practice in each specific organizational climate. Therefore, the focus of future studies should include the establishment of effective management plans, as long as they consider the risk factors of occupational infection, actual exposure levels of infectious agents, and effectiveness of infection control interventions in each group, with careful regard for risk level in Korea workplaces.
Figures and Tables
References
1. Cohen R, Estacio PL. Ladou J, editor. Occupational Infections. Current Occupational & Environmental Medicine. 2004. 3rd ed. California: Mcgraw-Hill;268–286.
2. Panilio AL, Gerberding JL. Rosenstock L, Cullen MR, Brodkin CA, Redlich CA, editors. Occupational Infectious Diseases. Textbook of Clinical Occupational and Environmental Medicine. 2004. 2nd ed. Philadephia: Elsevier Saunders;469–451.
3. Results of Korean National Death Registry. Korean Statistical Office. accessed on 9 Sep 2010. Available at http://www.kosis.kr.
4. Results of Korean National Health & Nutrition Examination Survey III. Ministry for Health Welfare and Family Affairs. accessed on 9 Sep 2010. Available at http://knhanes.cdc.go.kr/.
5. Occupational Safety & Health Research Institute. The survey on of the cause of occupational injuries and diseases 1999. 2000. Incheon: Korea Occupational Safety and Health Agency.
6. Occupational Safety & Health Research Institute. The survey on of the cause of occupational injuries and diseases 2000. 2001. Incheon: Korea Occupational Safety and Health Agency.
7. Occupational Safety & Health Research Institute. The survey on of the cause of occupational injuries and diseases 2001. 2002. Incheon: Korea Occupational Safety and Health Agency.
8. Occupational Safety & Health Research Institute. The survey on of the cause of occupational injuries and diseases 2002. 2003. Incheon: Korea Occupational Safety and Health Agency.
9. Occupational Safety & Health Research Institute. The survey on of the cause of occupational injuries and diseasest 2003-4. 2005. Incheon: Korea Occupational Safety and Health Agency.
10. Occupational Safety & Health Research Institute. The survey on of the cause of occupational injuries and diseases 2005. 2006. Incheon: Korea Occupational Safety and Health Agency.
11. Occupational Safety & Health Research Institute. The survey on of the cause of occupational injuries and diseases 2006. 2007. Incheon: Korea Occupational Safety and Health Agency.
12. Occupational Safety & Health Research Institute. The survey on of the cause of occupational injuries and diseases 2007. 2008. Incheon: Korea Occupational Safety and Health Agency.
13. Ahn YS, Lim HS. Occupational infectious diseases among Korean health care workers compensated with industrial accident compensation insurance from 1998 to 2004. Ind Health. 2008. 46:448–454.
14. Occupational Safety & Health Research Institute. The Korean surveillance project for preventing percutaneous injury. 2009. Incheon: Korea Occupational Safety and Health Agency.
15. Kim YB. A study on needle stick injuries in health professionals. J Nurs Acad Soc. 1996. 26:605–622.
16. Han JS, Kang KS, Kim HS. A study to identify an occupational hazards for hospital working health care providers from needle stick injury as an occupational hazards of health care providers in hospital and prevention. Korean Nurse. 1995. 34:45–57.
17. Oh HS, Choi KW. Descriptive study of reported blood-borne exposures in health care workers in a university hospital. Korean J Nosocomial Infect Control. 2002. 7:51–64.
18. Korean Association of Infection Control Nurses. Incidence and epidemiologic characteristics of reported sharps injuries in Korean hospitals: multi-center survey result. 2007. Seoul: Becton Dickinson Korea.
19. Lee SJ, Kim HS, Ma JE, Lee SM, Ham HS, Cho YJ, Jeong YY, Kim HC, Lee JD, Kim SJ, Hwang YS. Tuberculin skin test and QuantiFERON-TB Gold assay before and after treatment for latent tuberculosis infection among health care workers in local tertiary hospital. Tuberc Respir Dis. 2007. 62:270–275.
20. Lee K, Han MK, Choi HR, Choi CM, Oh YM, Lee SD, Kim WS, Kim DS, Woo JH, Shim TS. Annual incidence of latent tuberculosis infection among newly employed nurses at a tertiary care university hospital. Infect Control Hosp Epidemiol. 2009. 30:1218–1222.
21. Ahn YS, Lim HS. Occupational disease among agricultural, forestry and fishery workers approved by Korea Labor Welfare Corporation. Korean J Occup Environ Med. 2007. 19:1–16.
22. Korea Center for Disease Control and Prevention. The characteristics of recent trends in Scrub-typhus. Commun Dis Mon Rep. 2004. 15:246–252.
23. Lim HS. Changing patterns of communicable diseases in Korea. J Prev Med Public Health. 2005. 38:117–124.
24. Chung MH. Adult immunization. Korean J Med. 2008. 74:344–347.
25. Lee MS. Vaccination experience to expeditionary forces of Korea for participation of peace keeping operation in the forces of the organization of UN. Keimyung Med J. 1998. 17:289–296.
26. Kang JK. Disease of Korean patients evacuated from middle east Asia and Africa. Yonsei Rep Trop Med. 1984. 15:89–90.
27. Kim HC. Recent status on Korean overseas workers. Yonsei Rep Trop Med. 1984. 15:99–102.
28. Soh CT, Kim J, Min D. Korean workers in tropical countries (middle east) with special reference to their understandings of tropical diseases. Yonsei Rep Trop Med. 1985. 16:45–58.
29. Kim HY. The policy of communicable disease from abroad. J Korean Med Assoc. 2004. 47:895–900.
30. Cho SH, Ju YS, Kang D, Kim S, Kim IS, Hong ST. Laboratory-acquired infections with Hantavirus at a research unit of medical school in Seoul, 1996. Korean J Prev Med. 1999. 32:269–275.
31. Pal M, Lee CW. Microsporum canis infection in a horse and its transmission to man. Korean J Vet Clin Med. 1998. 15:196–198.
32. Lee JH, Song MH, Park JW, Bu TS, Whang KU. Microsporum canis infections transmitted from a tiger in a group. Korean J Dermatol. 2000. 38:553–556.
33. Jung S, Her M, Kim J, Kim J, Hwang I, Ku BK, Park YH, Yoo HS. Bovine brucellosis in Korea. J Zoonoses. 2010. 1:1–15.
34. Labor laws of Korea 2010. Ministy of Employment and Labor. accessed on 9 Sep 2010. Available at http://www.moel.go.kr/english/ibook-laws2/laws/book.html.
35. Korea Occupational Safety and Health Agency. KOSHA-CODE H-46-2008. Guideline for preventing of injury for needle stick and sharp vehicles in health care workers. 2008. Incheon: Korea Occupational Safety and Health Agency.
36. Ministry of Employment and Labor. Korean Center for Disease Control. Ministry for Health, Welfare, and Family Affairs. 2009 Guideline of business continuity plan for pandemic swine flu H1N1. 2009. Seoul: Ministry of Employment and Labor.
37. Survey on Industrial Accidents. Statistics and Information Department, Ministry of Health, Labour and Welfare Japan. 2009. accessed on 9 Sep 2010. Available at http://www.mhlw.go.jp/.
38. Finnish Institute of Occupational Health. Ammattitaudit ja ammattitautiepailyt 2006. 2007. Helsinki: Finnish Institute of Occupational Health.
39. The result of survey for occupational injury and illness. European Commission. Eurostat. accessed on 9 Sep 2010. Available at http://epp.eurostat.ec.europa.eu/portal/page/portal/eurostat/home/.
40. The national surveillance system for hospital health care workers: summary report for data collected from June 1995 through July 1999. Centers for Disease Control and Prevention. 2003. accessed on 9 Sep 2010. Centers for Disease Control and Prevention;Available at http://www.cdc.gov/ncidod/hip/NASH/report99.pdf.
41. Uniform needlestick and sharp object injury report 21 hospitals, 1999. International Health Care Worker Safety Center. EPINet. accessed on 9 Sep 2010. Available at http://www.med.virginia.edu/medcntr/centers/EPINet/soi99.html.
42. Jeong J. A study on the embalming regulation. 2008. Graduate School for Social Education, Myongji University.
43. Takahasi K. Ladou J, editor. Occupational Infection. Current Occupational and Environmental Medicine. 2008. Fourth ed. California: Mcgraw-Hill;262–265.
44. Bloodborne infection control. National Institute of Occupational Safety and Health. accessed on 9 Sep 2010. Available at http://www.cdc.gov/niosh/topics/.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download