Abstract
Skin disease is the most common occupational disease, but the reported number is small in Korea due to a difficulty of detection and diagnosis in time. We described various official statistics and data from occupational skin disease surveillance system, epidemiological surveys and cases published in scientific journals. Until 1981, 2,222 cases of occupational skin disease were reported by Korean employee's regular medical check-up, accounting for 4.9% of the total occupational diseases. There was no subsequent official statistics to figure out occupational skin diseases till 1998. From 1999, the Korea Occupational Safety and Health Agency (KOSHA) published the number of occupational skin diseases through the statistics of Cause Investigation for Industrial Accidents. A total of 301 cases were reported from 1999 to 2007. Recent one study showed the figures of compensated occupational skin diseases. Many of them belonged to daily-paid workers in the public service, especially forestry workers. Also, it described the interesting cases such as vitiligo and trichloroethylene-induced Stevens-Johnson Syndrome. Skin diseases are still important though the number of cases has decreased, and therefore it is recommended to grasp the status of occupational skin diseases through continuous surveillance system and to make policy protecting high-risk group.
Skin diseases account for the greatest part of occupational diseases, but few countries grasp the actual prevalence. In the USA, where Bureau of Labor Statistics (BLS) produces the annual number of incidence and incidence rate of occupational diseases through the Survey of Occupational Injuries and Illnesses (SOII), the rate of occupational skin disease per 10,000 workers was 16.2 in 1972. It reduced to 4.5 in 2006 (the total rate of occupational disease was 24.6, with proportion of skin disease being 18%), but still had the highest incidence rate among the diseases which were included in the classification to be grasped (1). In the UK, Health and Safety Commission (HSC) estimated that about 23,000 workers (78 per 100,000 workers) had skin diseases in 2006/2007 (2). Korea has no statistics on incidence rate of occupational skin disease, but the Ministry of Labor reported 19 cases of skin diseases through the Statistics on Industrial Accidents Analysis, among 2,098 cases of occupational disease in 2007 (3). An analysis of occupational diseases compensated with the Industrial Accident Compensation Insurance (IACI) in Korea revealed that skin diseases accounted for 17.2% of occupational diseases, being the fifth most common occupational disease following pneumoconiosis, hearing loss, infectious diseases, and poisoning (4).
Skin disease is a common occupational disease, but it is not acknowledged as much by occupational physicians or dermatologists because of its mildness and difficulty in diagnosing the patients in time. In Korea, occupational skin disease is difficult to find even with annual Special Health Examination for sorting out occupational diseases among workers exposed to hazards, because: 1) employees or employers, and agencies for Special Health Examination do not try hard for diagnosis or applying for compensation taking nuisance involved in reporting the patients, thinking occupational skin disease is not serious and life threatening, 2) physicians participating in Special Health Examination do not have sufficient knowledge on occupational skin diseases, and there is no simple testing methods which can identify the lesion in a number of workers in a short time, nor a system to bring cases to experts for identification, and 3) considering the usually transient characteristics of occupational skin diseases, health managers including occupational physicians should provide information to Special Health Examination agencies through regular observation, but the current Special Health Examination system is not suitable for it, and other type of system such as occupational skin diseases surveillance system is needed to be established (5).
In this study, various official statistics, data from occupational skin diseases surveillance system, data from epidemiological surveys, and cases reported in scientific publications were collected and reviewed to describe the kinds of occupational skin diseases and the characteristics of high-risk group in Korea.
In Korea, official counting of occupational skin diseases has not been attainable since 1982 when the case report form for special health examination was changed from disease-specific to agent-specific reporting, and therefore it is practically impossible to get or estimate the statistics, e.g., incidence rate, of occupational skin diseases.
Total number of workers with occupational skin diseases by Korean employee's regular medical check-up for 14 yr (1968-1981) was 2,222, accounting for 4.9% of total 45,071 cases of workers with occupational diseases and peaking in 1974 with 615 cases. Cellulitis and dermatitis reported in silk-reeling and textile manufacturing were most common (1,627 cases, 73.2%), followed by cellulitis and dermatitis in other types of industry excluding silk-reeling and textile manufacturing (438 cases, 19.7%). Eighty cases of corrosion, ulcer, and dermatitis by acid and alkali, and 67 cases of burn and frostbite were reported. As for primary epithelial cancer and anthrax from animal handling, only 6 and 4 cases were reported in 1972 and 1970, respectively (Table 1). As seen above, reported occupational skin diseases had mainly acute and injury nature which had apparently clear causal relationship.
Statistics on Industrial Accidents Analysis by Ministry of Labor presented occupational skin diseases from 2006. Twenty-nine cases (8) and 19 cases (3) of skin disease were approved for medical care benefit in 2006 and 2007, respectively.
Since 1999 KOSHA has published 'Statistics on Cause Investigation for Industrial Accidents', which describes the characteristics of workers with recognized industrial accident and their workplaces. These statistics are the only statistics in occupational health field approved by the Government (Approval no. 38001) and highly reliable. However, these statistics give very limited information.
Three hundred and one cases of skin disease were recognized as work-related for 9 yr (1999-2007), accounting for 0.6% of total 55,120 cases of work-related disease and 2.8% of total 10,619 cases of occupational disease during the period. By year, 26 cases (9.7%) in 1999, 40 cases (15.0%) in 2000, 51 cases (19.1%) in 2001, 34 cases (12.7%) in 2002, 39 cases (14.6%) in 2003, 51 cases (19.1%) in 2004, and 20 cases (7.5%) each in 2005-2007 were reported, respectively, peaking in 2001 and with a mean of 33 cases. Among the 301 cases, 267 cases (except 34 cases recognized in 2002) were analyzed.
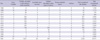
By sex, occupational skin diseases were reported more in male, with 198 cases (74.2%) in male and 69 cases (25.9%) in female workers. By age, 50-59 yr old group accounted for the greatest part (82 cases, 30.7%), followed by 40-49 yr old group (75 cases, 28.1%), 30-39 yr old group (52 cases, 19.5%) and 60 yr or older group (26 cases, 9.7%). By duration of performing the job which caused the skin disease, less than 3 months was most common (119 cases, 44.6%), followed by 1-5 yr (55 cases, 20.6%) and 3 months-1 yr (44 cases, 16.5%), indicating that less than 1 yr accounted for 61.1%. By industry classification, public administration, welfare, educational service accounted for the greatest part (83 cases, 31.1%), followed by manufacturing (80 cases, 30.0%) and recreational, sports & personal service activities (25 cases, 9.4%). By job classification, elementary occupations were most common (104 cases, 39.0%), followed by plant, machine operators & assemblers (52 cases, 19.5%), craft and related trades workers (48 cases, 17.9%), and service and sales workers (25 cases, 9.4%). By causative agent, biological agents were most common (164 cases, 61.4%), with 3 cases (1.1%) due to physical agents, 96 cases (36.0%) due to chemical agents, and 4 cases due to unknown agents (Table 2).
'Statistics on Cause Investigation for Industrial Accidents' gives only very limited information on workers with skin diseases compensated as occupational disease, and is insufficient for understanding the kinds of skin diseases and causative agents. Therefore, Ahn et al. (9) analyzed in detail the characteristics of skin diseases which were recognized as work-related during 1999-2003.
Two hundred and sixteen cases of skin disease were recognized as work-related diseases for 5 yr (1999-2003). The majority of disease were contact dermatitis (116 cases, 53.70%), cellulitis (36 cases, 16.7%), vitiligo (11cases, 5.7%) and scabies (7 cases, 3.2%). By causative agent for 121 cases of dermatitis and eczema, 76 cases of allergic contact dermatitis were due to plants (53 cases), chemicals (9 cases), metals (4 cases), drugs (4 cases), dyes (2 cases), cosmetics (1 case), and other agents (3 cases). 9 cases of allergic urticaria were caused by plants (8 cases) and dye (1 case). The major types of industry were public administration and defense (91 cases, 42.1%), manufacturing (57 cases, 27.1%), other community, repair and personal service activities (13 cases, 6.0%), construction (12 cases, 5.6%) and business activities (11 cases, 5.1%). Many cases occurred among day laborers for public service, especially forestry care workers.
Since 1999 occupational disease surveillance systems by disease or region have been operated, and the operating researchers reported (10-14) the results through which we could understand the kinds and characteristics of occupational skin disease partly, although they were not official statistics. These data were not nationwide but limited to some regions only (Daejeon, Gumi, and Busan · Ulsan · Gyeongnam area); the cases were not invariably confirmed as occupational diseases; and they provided no concrete description for characteristics of the skin diseases or workers. In summary, these data are insufficient for occupational physicians or clinicians to accurately understand the kinds of skin diseases and to utilize in managing the patients who are suspected to be occupational and preventing occupational skin diseases.
Occupational skin disease surveillance system in Korea comprised the model project by KOSHA from May to November 1998 and one-year operation in 2000, falling short of the established meaning of surveillance system defined with continuous reporting and feedback.
Occupational skin disease surveillance system by KOSHA (10) was composed of doctors and nurses in 150 enterprises with dispensary or attached hospital, physicians in 92 Special Health Examination agencies and 150 dermatologists. KOSHA collected and analyzed the suspected cases of occupational skin disease reported by surveillance system using pre-distributed report form from 1 May to 30 November 1998. Cases from 1,077 workers were reported by 66 among 150 enterprises and 47 among 92 Special Health Examination agencies. Among those cases, 490 cases from 431 workers were judged work-related skin diseases by established criteria. The analysis of data from surveillance system revealed that contact dermatitis (363 workers, 74.1%) was most common among occupational skin diseases, followed by pigment disorders (36 workers, 7.3%), nail disorders (33 workers, 6.7%), and burns (21 workers, 4.3%). By industry where the workers with contact dermatitis were engaged and by agents used in workplaces, automobile and trailer manufacturing (105 workers, 29.6%) and organic solvents (183 cases, 46.7%) accounted for the greatest part. By characteristics of contact dermatitis, 64.5% (165 workers) were chronic cases with repeated healing and relapse. In addition, 245 workers (72.5%) answered that colleagues had similar skin diseases, which indicated clustered incidence. In the aspect of controlling, 133 workers (64.9%) answered that personal protective equipment (PPE) was not effective, accounting for the larger number compared with workers who answered that PPE was effective. In addition, as many as 73 workers (25.4%) did not take treatment for the disease. Twenty-seven workers (8.7%) answered that they had taken early leave or been absent from workplaces.
The surveillance system showed that workers were collectively and chronically afflicted with work-related skin diseases, seldom wore PPE, and were not properly treated at onset of disease, thus early leave and absence were not unusual. Establishing the practical control measures for occupational skin diseases and consistent grasping of the problems through the surveillance system are needed.
From 1995 to 2008, 52 cases of skin disease were investigated to OSHRI for estimating the work-relatedness, among which 28 cases were judged as highly work-related. Several notable cases are presented below.
Stevens-Johnson syndrome associated with occupational exposure has gained the attention since the mass outbreak in a Korean electronic company in the Philippines. Erythema multiforme or Stevens-Johnson syndrome were developed in some workers who were exposed to TCE used as cleaning agent for electronic parts, and 2 workers died (15). In addition, 7 cases have been reported in Korea, including 3 cases published in scientific journals (16-18) and 4 cases for which epidemiological surveys were conducted by OSHRI (19, 20). A mass outbreak of Stevens-Johnson syndrome was also reported among Filipino workers in an electronic product manufacturing company in Taiwan, but through case-control study (21) it was concluded to be caused by anthelmintics (mebendazole, metronidazole) use. The 7 cases in Korean company in the Philippines and 5 cases in Korea have no relations with anthelmintics use, and were all developed in workers who were exposed to TCE as cleaning agent, with toxic hepatitis and within 1 month of TCE exposure. Therefore, studies to clarify the cause, such as case-control study in patients with Stevens-Johnson syndrome or erythema multiforme who visit a dermatologist, are needed. In addition, although the causality has not been scientifically established yet, as an advance preventive measure health examination within 1 month after placement is recommended for workers exposed to TCE to recognize the development of Stevens-Johnson syndrome and to take appropriate measures.
Vitiligo does not present serious symptoms, but the patients may suffer from mental anguish due to aesthetic reason and have difficulty in social activity. However, even when recognized as occupational disease, compensation benefit for vitiligo is very little because compensation is based on disabilities. Vitiligo due to occupational exposure to chemicals is known to be caused by materials containing hydroquinone or materials containing alkylphenol or catechol derivatives. Those materials are contained usually in agents for preventing emulsification of oil, deodorizing agents, copying papers, formaldehyde resins, phenolic disinfectants, pesticides, rubber glue, automotive fuel additives, plasticizers for cellulose acetate, printing ink, lacquer, paint, and resin. Therefore, vitiligo may be developed in workers who are engaged in processes manufacturing of handling these materials. Eleven cases of vitiligo were estimated by OSHRI as highly related with work, among which 5 cases were observed in painters exposed to epoxy paint and alkyd paint, and others were caused by vitiligo-causing agents contained in cleaning agent, cutting oil, and asphalt (10).
Among studies on occupational skin diseases published in scientific journals in Korea until recently, less than 30 studies conformed to the epidemiological study in one or more workplaces, except case reports. Earlier data reporting the prevalence of occupational skin diseases in Korea were shown in a study on workers' non-occupational and occupational diseases performed by Industrial Health Research Institute of Catholic University together with the Korean National Tuberculosis Association, in 148,358 workers at 1,773 workplaces with more than 30 employees nationwide, from April to November 1963: the prevalence of occupational skin diseases was 3.2%, accounting for about 25% of total prevalence of occupational diseases (22). After the late 1980s, occupational diseases became social issues, occupational skin diseases have gained increasing attention, and several epidemiological studies were published. Special Health Examination for workers at 5 car repair shops in Gyeonggi-Incheon area, performed by Ministry of Labor in November 1990, revealed that 83.1% of the workers had one or more kinds of occupational skin diseases (22).
In the 1990s, some epidemiological studies were conducted for workers of manufacturing factories such as tannery, automobile, shipyard, metal, etc. It showed that a great number of workers were afflicted with skin diseases (22-24).
In the 2000s, epidemiologic studies were conducted on workers not only manufacturing factories but also service industries such as beauty shops and healthcare workers. A study in beauty shops showed that 45.8% among 96 workers complained of contact dermatitis (25). A study in health care workers in a hospital showed that 40.9% of the workers complained of skin diseases (26) (Table 3).
Jobs for which occupational skin diseases were reported in scientific journals from 1972 to 2007 much varied, including cotton mill worker, silk-reeling worker, farmer, glass pane manufacturer, copper smelter, deer farmer, molding worker (automobile company), stainless steel products manufacturing worker, worker dealing with radiation, chemical company worker, tanner, worker dealing with epoxy resin, metal manufacturing worker, mechanics, sewage treatment plant worker, office worker (VDT), textile mill worker, worker dealing with vibration tool, frozen food handlers, plastic case products manufacturing worker, waterproofing worker, cellular phone case manufacturing worker, and metal cleaning worker. The kinds of occupational skin diseases included foot mycosis, toxic epidermal necrosis, contact dermatitis (allergic and irritant), contact urticaria, toxic erythema, exfoliative dermatitis, radiation dermatitis, facial eczema by VDT, erythema multiforme, Raynaud syndrome, chilblain, vitiligo, photoxic dermatitis, oil acne, folliculitis, argyria, Stevens-Johnson syndrome by TCE, and exfoliative dermatitis, etc. (16-18, 22, 27, 28) (Table 4).
Estimating prevalence rate of work-related skin diseases is very difficult to calculate representative numerator and denominator. In Korea, there has been "Survey on Workers' Health" every 5 yr since 1999. Among items of this survey conducted in 2004, there was one asking about occurring of work-related skin diseases, workers suffered from skin problems caused or made worse by work, to workers. This survey relies on self diagnosis and responses given therefore depend on lay workers' perceptions of medical matters and work-relatedness. In 2004, 12,989 workers were systematically subject from Korean workers employed in companies with more than 5 workers. Of them, 76 workers responded to work-related skin diseases (29). The prevalence rate of work-related skin diseases was 585 per 100,000 workers. The prevalence rate was higher in women (589) and manufacturing industries (627) than those of men (564) and non-manufacturing industries (503). This was 7.5 times higher than that of Great Britain (78/100,000 employees) estimated in 2004/2005 as the similar self-reported measure (30).
The number of patients with occupational skin diseases in Korea before 1982 was understood from the statistics for patients in the result of Korean employee's regular medical check-up. The number of patients with occupational skin diseases was 2,222 and this accounted for as high as 4.9% of total patients with occupational diseases. Patients with skin diseases after 1982 could not be identified since occupational skin diseases were not separately reported in the statistics of Korean employee's regular medical check-up after 1982. Statistics for work-related diseases using data from 'Cause Investigation for Industrial Accidents' had shortcomings as they show only the outlines including the number of cases of skin diseases, sex, age, working duration, large-class industry job classification while the detailed analyses for the types of skin diseases, hazards and high-risk group were not performed.
One study in workers recognized as having work-related diseases indicated that high-risk group for occupational skin diseases was the group of public workers engaged in forestry care, the most frequently recognized skin disease was allergic contact dermatitis rather than irritant contact dermatitis. Thus it is estimated that preventive measures, including instruction prior to work, for preventing occupational skin diseases, especially allergic contact dermatitis, are needed for daily-paid laborers engaged in public service. In addition, preventive measures, including active program for case finding, for diseases such as skin cancer, vitiligo, and Stevens-Johnson syndrome (exfoliative dermatitis) caused by TCE are needed since the cases of these diseases are expected to increase in the future considering the number of exposed workers though only a few cases have been recognized up to the present.
Statistics for work-related diseases displayed merely dozens of cases of skin diseases per year, but data from surveillance system showed that the incidence of occupational skin diseases was still not low. Analyses revealed that workers were collectively and chronically afflicted with work-related skin diseases, seldom wore PPEs, and were not properly treated at onset of disease, thus early leave and absence were not unusual. Establishing the practical control measures for occupational skin diseases and consistent grasping of the problems through the surveillance system are needed.
The prevalence rate of work-related skin diseases was 585 per 100,000 workers, which was estimated based on self-reported National Survey on Workers' Health in 2004. It was 7.5 times higher than that of Great Britain (78/100,000 employees) estimated in 2004/2005 as the similar self-reported measure.
This study revealed the outline of occupational skin diseases in Korea. Occupational skin diseases are still important occupational diseases though the number of cases has decreased, and therefore it is recommended to grasp the status of occupational skin diseases through continuous surveillance system and to set up a system for managing high-risk group.
Figures and Tables
Table 2
Characteristics of workers with occupational skin diseases, based on Cause investigation for industrial accident

References
1. US Department of Labor, Bureau of Labor Statistics. Occupational injuries and illness. 2008. Washington, DC: US Government Printing Office.
2. Health and Safety Commission (HSC). Health and Safety Statistics Highlights 2006/2007. 2008. HSE Books.
3. Ministry of Labor. 2007 Statistics of Industrial Accidents Analysis. 2009. Seoul: Ministry of Labor;207–208.
4. Ahn YS, Kang SK, Kim KJ. Analysis of occupational diseases compensated with the Industrial Accident Compensation Insurance from 2001 to 2003. Korean J Occup Environ Med. 2004. 16:139–154.
5. Eun HC. Yum YT, editor. Occupational skin disease. Training materials for occupational and environmental medicine. 1996. Seoul: The Rainbow Press;517–527.
6. Korea Industrial Health Association (KIHA). A book in celebration of 30th anniversary of Korea Industrial Health Association. 1993. Seoul: KIHA.
7. Korea Occupational Safety and Health Agency (KOSHA). 1999-2007 Cause investigation for industrial accidents. 2009. Incheon: KOSHA.
8. Ministry of Labor. 2006 Statistics of Industrial Accidents Analysis. 2008. Seoul: Ministry of Labor.
9. Ahn YS, Kim DH, Lee JY, Kim HO. Characteristics of occupational skin diseases compensated with the Industrial Accident Compensation Insurance from 1999 to 2003. Korean J Dermatol. 2005. 43:331–341.
10. Ahn YS, Kim HO, Lee JY, Jung HK. Characteristics of occupational skin disease reported by surveillance system. Korean J Prev Med. 1999. 32:130–140.
11. Chang SS, Kim S. Contact dermatitis surveillance system in Taejon City: Prevalence of contact dermatitis among the workers exposed to solvents and nonmetallic chemicals through an immediate health examination system in Taejon City. Korean J Occup Environ Med. 2000. 12:227–234.
12. Kang SK, Jee YK, Ahn YS, Kim HO, Ha MN, Kwon HJ, Paik NJ, Kim SA, Hong YC, Kim JY, Kang DH, Jung HS, Ha EH. The present status and perspective. Korean J Occup Environ Med. 2001. 13:116–126.
13. Kim SA, Kim JS, Jeon HR, Jung SJ, Kim SW, Lee CY, Ham JO, Yoo JY, Choi TS, Goo HB, Cho MH, Woo KH. Surveillance of work-related diseases in Kumi. Korean J Occup Environ Med. 2003. 15:95–110.
14. Kim JI, Kim BG, Kim JW, Chae CH, Yi CH, Kang D, Kim JH, Kim JH, Kim YW, Lee YH, Lee JH, Choi Y, Kim JH, Yun HR, Yoo CI, Jeong BG, Jang TW, Kim YG, Yun DY, Kang JU, Kim JE, Ahn JH, Lee DJ, Jang JH, Lee KY, Song HR, Lee YH, Cho BM, Choi HR, Koh SB, Kim E, Lee YJ, Hong YS, Jung KY, Kim JM, Kim JY. Occupational disease surveillance system in Busan, Ulsan, Kyung-Nam area. Korean J Occup Environ Med. 2004. 16:1–12.
15. Occupational Safety and Health Research Institute (OSHRI). Health Sector Research Article 99-79-261: Epidemiologic survey report on the KP-company in Philippines. 1999. OSHRI;5–6.
16. Hong DP, Kim JS, Kim SH, Kim JM, Lee ES. A case of toxic erythema, toxic hepatitis and dermatitis due to tetrachloroethylene. Korean J Dermatol. 1985. 23:785–789.
17. Chae HB, Kim JA, Lee KS, Park SM, Yoon TY, Yoon SJ. A case of hepatitis after occupational exposure of tetrachloroethylene. Korean J Hepatol. 1999. 5:59–64.
18. Chae HJ, Lee SK, Lee KJ, Kim JY, Lee SC, Shin DH, Moon JD. Exfoliative dermatitis and toxic hepatitis associated with occupational exposure to tetrachloroethylene. Korean J Occup Environ Med. 2003. 15:111–117.
19. Occupational Safety & Health Research Institute (OSHRI). Epidemiologic investigation report on work-related diseases. 1995. OSHRI.
20. Occupational Safety & Health Research Institute (OSHRI). Epidemiologic investigation report on work-related diseases. 2002. OSHRI.
21. Chen KT, Twu SJ, Chang HJ, Lin RS. Outbreak of Stevens-Johnson Syndrome/toxic epidermal necrolysis with mebendazole and metronidazole use among Filipino laborers in Taiwan. Am J Public Health. 2003. 93:489–492.
22. Lim HS, Cheong HK, Choi BS, Kim JY, Sung YO, Kim YH. A study on the establishment of management methods about occupational dermatoses. Korean J Prev Med. 1996. 29:617–638.
23. Park JB, Lee KJ, Jang JY, Chung HK. Skin diseases of male workers in painting workplace. Korean J Prev Med. 1997. 30:830–839.
24. Park JI, Kim HO, Park SR, Oh CH, Kim SD, Yum YT. Occupational dermatoses in metalworking fluid exposed workers. (II) Allergic contact dermatitis. Korean J Dermatol. 1998. 36:246–251.
25. Park JH, Ro YS. Occupational skin disease in hairdressers: results of patch test. Korean J Dermatol. 2006. 44:669–674.
26. Cho YK, Park HJ, Lee JY, Cho BK. Occupational dermatoses of health care workers in Korea. Korean J Dermatol. 2005. 43:887–890.
27. Shin JY, Hong YC, Leem JH, Park SG, Lee JN, Kim HC. Occupational allergic contact dermatitis like erythema multiforme induced by bolivian rosewood. Korean J Occup Environ Med. 2004. 16:220–226.
28. Kim M, Kim D, Hwang S, Park J, Seo C, Shin S, Ahn J, Lee J. A case of allergic contact dermatitis caused by epichlorohydrin and tris-DMP in an epoxy resin worker. Korean J Occup Environ Med. 2009. 21:276–282.
29. Occupational Safety and Health Research Institute (OSHRI). Health Sector Research Article 2004-24-861: Survey for Workers' Health 2004. 2004. OSHRI.
30. Dermatitis and other skin disorders, Table SWIT3W12-2004/2005. Health and Safety Executive (HSE). 2005. accessed May 10 2010. HSE;Available at http://www.hse.gov.uk/statistics/lfs/0405/swit3w12.htm.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download