Abstract
Occupational hepatic disorders are classified into toxic hepatitis, viral hepatitis, and chemical-induced malignancy in Korea. Toxic hepatitis cases were reported in workers who were exposed to dimethylformamide, dimethylacetamide, or trichloroethylene. Pre-placement medical examination and regular follow-up are necessary to prevent the development of toxic hepatitis. Viral hepatitis was chiefly reported among health care workers such as doctors, nurses and clinical pathology technicians who could easily be exposed to blood. Preventive measures for these groups therefore include vaccination and serum monitoring programs. Hepatic angiosarcoma caused by vinyl chloride monomer (VCM) exposure is a very well known occupational disease and it has not been officially reported in Korea yet. Some cases of hepatocellular carcinoma were legally approved for compensation as an occupational disease largely by overwork and stress, but not supported by enough scientific evidence. Effort to find the evidence of its causal relationship is needed.
Hepatic disorders are very common in Korea. The Korea National Health and Nutrition Examination Survey (KNHANES) in 2005 showed that 3.7% of the total population were hepatitis B virus carriers (1); and the health examination for workers in 2007 reported that hepatic disorders ranked the second highest after hypertension, at 139.3 per 10,000 workers (2).
The reason hepatic disorders are very important in occupational medicine is that most chemicals are metabolized in the liver and toxic metabolites generated through the metabolism are the main cause of liver damage. However, many hepatic diseases are difficult to diagnose due to nonspecific clinical manifestations. Moreover, as hepatic diseases like alcoholic or viral hepatitis are common in Korea, it is difficult to confirm occupational hepatic disorders. Simultaneous conditions, such as viral hepatitis and alcohol or drug abuse, may confound the liver disorders caused by specific occupational hepatotoxic agents. Toxic hepatic disorders can be divided into three categories according to their etiology: viral hepatitis (inflammatory liver disorders), chemical-induced injuries, and physical agent-induced lesions (radiation) (3). Hepatic toxic disorders are generally viewed as occupational disorders, and the aggravation of hepatic disorders due to overwork has been also reported as an occupational disease in Korea.
This article will review the scale of occupational hepatic disorders in Korea, cases of toxic hepatitis, cases of occupational viral hepatitis and occupational hepatocellular carcinoma due to overwork and stress.
Health examination is carried out every two years for clerical workers and every year for non-clerical workers in Korea. The examination includes liver function tests. In 2007, 70,345 of 5,049,400 workers who underwent these health examinations were diagnosed with abnormal findings in liver. This marked the second highest prevalence rate, following hypertension (Fig. 1). In the National Health and Nutrition Examination Survey, performed every three years in Korea, the proportion of hepatitis B virus carriers in 2005 was 3.7% of the total population, which was lower than that in 1998 and 2001 surveys, but still high (Fig. 2).
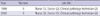
In 1999, the Korea Workers' Compensation and Welfare Service (COMWEL) reported 2 cases of toxic hepatitis caused by dimethylformamide (DMF), 3 cases of hepatocellular carcinoma due to overwork and 7 cases of liver cirrhosis (Table 1) (4). Between 2001 and 2003, 14 occupational viral hepatitis cases were reported (1 case of hepatitis A, 10 cases of hepatitis B, and 3 cases of hepatitis C). Six cases of toxic hepatitis caused by DMF, 4 cases of toxic hepatitis due to waste materials, and 1 case of hepatocellular carcinoma due to overwork were reported during the same period (5). While the number of reported occupational hepatic disorders was very small, it is likely that there may be a much higher number of unreported cases given the high prevalence of hepatic disease in the general population.
Hepatotoxic substances have been classified as either intrinsic or idiosyncratic based on their presumptive mechanism of action. Most hepatotoxins are intrinsic toxins; i.e., their hepatotoxicity is a predictable property of the substance itself, and most individuals will be affected if the dose is high. Most intrinsic toxins, called direct toxins, are defined as substances or their metabolites that directly injure the liver rather than indirectly interfering with metabolic pathways. Acute and subacute injury by such agents produces varying degrees of hepatocellular injury with necrosis and steatosis. A few hepatotoxins are idiosyncratic, in that they cause liver injury that is sporadic and generally not dose-related, possibly due to hypersensitivity or immunologic-type reaction (3). In Korea, DMF, dimethylacetamide (DMAc) and trichloroethylene (TCE) have been known as idiosyncratic agents which induce toxic hepatitis. Also, a case of toxic hepatitis of a worker who used methylene chloride as a degreasing agent was reported in the year of the report (2004) (6).
Generally, three conditions must be satisfied for diagnosis of occupational toxic hepatitis. First, the liver damage must occur after a worker commences employment at the workplace in question. Second, liver enzyme levels must increase to at least double the upper limit of normal levels, while pre-exposure serum aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels must be in the normal range. Third, other possible causes of liver disease should be excluded (7-9).
The best-known major hepatotoxic chemicals are halogenated compounds such as carbon tetrachloride (CCl4) and chloroform. Use of these materials has been strictly restricted in Korea, so there have been very few recent reports of toxic hepatitis caused by these chemicals. However, a Korean company has used incidentally these hepatotoxic chemicals in an overseas workplace, with several toxic hepatitis cases. Carbon tetrachloride and chloroform were found in a detergent that the company used, exceeding twice the occupational exposure limits. Eighteen (64.3%) of 28 workers who used the detergent had signs of typical toxic hepatitis. Of particular note, 8 workers (28.6%) showed severely decreased liver function with ALT levels higher than 100 IU/L, and one worker presented with laboratory findings indicative of serious liver damage (10).
DMF is a colorless, water-soluble liquid with a faint ammonia-like odor. It is widely used as a solvent, especially for resins and polar polymers, and is also employed as a booster or co-solvent in applications such as protective coatings, adhesives, films, and printing inks. DMF is a component of many paint removers and is used in selective gas absorptions and solvent extractions (11).
According to the data of the surveillance system in Gumi, Gyeongsangbuk-do, 34 cases of toxic hepatitis were reported from 1 January 2001 to 30 April 2002. All these cases occurred in 2 synthetic fiber producing companies which used DMF and DMAc. And 28 of the 34 cases were detected through the surveillance system that included liver function tests every 10 days for 3 months. In 30 cases (88.2%), toxic hepatitis occurred within 3 months of workers starting work at the company (Table 2) (12). Table 3 shows the cases of toxic hepatitis caused by DMF or DMAc in Korea (Table 3). Most cases occurred within 2 or 3 months of starting work, but the shortest period was 4 days. Synthetic fiber (spandex) production and synthetic leather production companies were the sources of DMF and DMAc. Most workers recovered from the disease with treatment after early detection, but there were also cases of death in spite of proper treatment.
The close observation of 997 workers who worked in synthetic fiber production using DMAc from 1 February 2000 to 30 June 2004 revealed 72 cases of suspected toxic hepatitis (13). There were no cases that occurred within 2 weeks of starting employment, with most cases occurring between 2 and 17 weeks of starting employment. The incidence was high between 2 and 9 weeks after starting work, and the highest incidence was seen between 4 to 5 weeks after starting work. Most workers quickly improved after exposure was discontinued; and at 48-week follow up all cases had resolved. These cases of toxic hepatitis thus seem to have been induced by an idiosyncratic mechanism.
TCE is a colorless, nonflammable liquid with a sweetish odor resembling chloroform. In the past, TCE was used as an extractant in food-processing, but this was discontinued in 1975 and it is now used for vapor degreasing and as a solvent. It is sometimes used as a surgical anesthetic and analgesic (14).
In one report, as many as 10% of workers exposed over 30-work-years to TCE became jaundiced, with subacute or massive hepatic necrosis and postnecrotic scarring noted at autopsy (15). Exposure to TCE can also result in hepatic necrosis similar to that seen with carbon tetrachloride.
In addition to the intrinsic pathway mechanisms mentioned above, several cases of TCE toxic hepatitis induced through idiosyncratic pathways have also been reported in Korea. Table 4 shows some cases of toxic hepatitis caused by TCE exposure. In these cases most toxic hepatitis occurred about 30 days after exposure began (Table 4) (16-20). These findings are similar to those of Phoon et al., who showed that symptoms related to toxic hepatitis were reported approximately 2 to 5 weeks after exposure to TCE (21).
Toxic hepatitis caused by DMF, DMAc and TCE, which have been characteristically reported in Korea, is considered to occur through idiosyncratic mechanisms for two reasons: it occurs approximately one month or longer after starting work, and it even occurred in workplaces with exposure levels lower than the occupational exposure limit.
Such toxic hepatitis can be detected early by pre-placement medical examinations and regular follow-up every 10 days after placement. Because this kind of toxic hepatitis is still reported in the 2000s, and victims of these chemicals were mostly immigrant workers and workers of small enterprises, it is necessary to intensify education and supervision of employers. Furthermore, active involvement of an occupational physician is also required in prevention and treatment.
Viral hepatitis is an endemic disease in Korea. It is also commonly reported as an occupational disease. Health care workers and intravenous drug users are especially at risk for HBV and HCV infections (3). According to the data of Korean health care providers, 4 cases of viral hepatitis were approved in 1999 and 5 cases in 2000 (Table 5). These cases were nurses, doctors and clinical pathology technicians, and they were infected while collecting blood (22). Accidental blood contamination such as needle stick injury seems to be the main route of infection.
Vinyl chloride monomer (VCM) exposure can induce hepatocellular carcinoma and hepatic angiosarcoma. While hepatic malignancy due to VCM has not been reported in Korea yet, active surveillance is clearly required for the many employees currently exposed to VCM while working at chemical industrial complexes.
While 3 cases of occupational hepatic malignancy due to overwork were approved by the court in 1999 (4), only 1 case was approved between 2001 and 2003 (5). In the past, many cases of hepatic malignancy were approved as occupational diseases by the court, despite the disagreement of COMWEL, because the court deemed it legally reasonable that high levels of job stress and overwork hastened the natural course of the disease, especially in hepatitis B carriers and even in the absence of chemical exposure. However, such approvals have decreased recently because of the lack of scientific evidence.
Overwork has typically been legally accepted as a cause of occupational hepatic malignancy in Korea. This reflects the recognition of the high prevalence of overwork in Korea and the fact that, despite the efforts of Industrial Accident Compensation Insurance, the Korean social security service is unable to adequately compensate hepatic malignancy patients. Occupational hepatic malignancy due to overwork may decrease in the future, if overwork decreases and if other social security services, such as health insurance, expand their roles.
Alcoholic hepatic disease and viral hepatitis are very common in Korea and this characteristic makes it hard to diagnose occupational hepatic disorders. Deaths from toxic hepatitis due to DMF have been reported quite recently, and this indicates that sufficient preventive measures have not yet to be taken. Health care providers are a high-risk group for occupational hepatic diseases in that they have a high possibility of exposure to blood and there are many hepatitis B virus carriers in Korea. Sufficient education and preventive measures, including active strategies like vaccination for health care providers, are therefore required. Occupational hepatic malignancies should be a topic of active research in the near future.
Figures and Tables
Fig. 1
Prevalence of major diseases found in the the National Health and Nutrition Examination Survey conducted in 2007 (number per million).

Table 1
Occupational liver disease approved by Korea Worker's Compensation and Welfare Service in 1999 (4)

References
1. Ministry for Health and Welfare. Results of Korean National Health & Nutrition Examination Survey III. accessed on 15 Oct 2009. Available at http://knhanes.cdc.go.kr/.
2. Statistics on occupational injuries and diseases 2008. Ministry of Employment and Labor. accessed on 15 Oct 2009. Available at http://www.molab.go.kr/policyinfo/safety/view.jspcate=10&sec=1&bbs_cd=105.
3. Johnson D, Groopman JD. Rom WN, editor. Toxic Liver Disorders. Environmental and Occupational Medicine. 2007. Philadelphia: Lippincott;789–799.
4. Ahn YS, Kang SK, Kwon HG, Chung HK. Analysis of occupational disease approved by Korea Labor Welfare Corporation in 1999. Korean J Occup Environ Med. 2001. 13:449–460.
5. Ahn YS, Kang SK, Kim KJ. Analysis of occupational diseases compensated with the industrial accident compensation insurance from 2001 to 2003. Korean J Occup Environ Med. 2004. 16:139–154.
6. Ha BG, Kim JS, Yu JY, Woo KH, Ham JO, Yoon SY, Jang YS, Jung SJ. A case of toxic hepatitis in a worker exposed to a cleansing agent mainly composed of methylene chloride. Korean J Occup Environ Med. 2004. 16:210–219.
7. Benichou C, Danan G, Flahault A. Causality assessment of adverse reactions to drugs-II. An original model for validation of drug causality assessment methods: case reports with positive rechallenge. J Clin Epidemiol. 1993. 46:1331–1336.
8. Danan G, Benichou C. Causality assessment of adverse reactions to drugs--I. A novel method based on the conclusions of international consensus meetings: application to drug-induced liver injuries. J Clin Epidemiol. 1993. 46:1323–1330.
9. Maria VA, Victorino RM. Development and validation for a clinical scale for the diagnosis of drug-induced hepatitis. Hepatology. 1997. 26:664–669.
10. Kang SK. Occupational toxic hepatitis. Occup Health. 2000. 143:5–12.
11. American Conference of Governmental Industrial Hygienists. Dimethylformamide. 2005 TLVs and BEIs: based on the documentation of the threshold limit values for chemical substances and physical agents and biological exposure indices. 2005. Cincinnati, OH: American Conference of Governmental Industrial Hygienists;1–3.
12. Kim SA, Kim JS, Jeon HR, Jung SJ, Kim SW, Lee CY, Ham JO, Yoo JY, Choi TS, Goo HB, Cho MH, Woo KH. Surveillance of work-related diseases in Kumi. Korean J Occup Environ Med. 2003. 15:95–110.
13. Jang YS, Yoon SY, Jo SY, Choi TS, Yoo JY, Woo KH, Ha BG, Jung SJ, Chun BY, Kim JS. Incidence of dimethylacetamide-induced toxic liver injury among workers in a synthetic fiber manufacturing company. Korean J Occup Environ Med. 2006. 18:246–254.
14. American Conference of Governmental Industrial Hygienists. Trichloroethylene. 2005 TLVs and BEIs: based on the documentation of the threshold limit values for chemical substances and physical agents and biological exposure indices. 2005. Cincinnati, OH: American Conference of Governmental Industrial Hygienists;1–6.
15. Klockars M. Riihimaki V, Ulfvarson U, editors. Solvents and the liver. Safety and health aspects of organic solvents. 1986. New York: Alan R. Liss;139–154.
16. Hong DP, Kim JS, Kim SH, Kim JM, Lee ES. A case of toxic erythema, toxic hepatitis and exfoliative dermatitis due to trichloroethylene. Korean J Dermatol. 1985. 23:785–789.
17. Chae HB, Kim JA, Lee KS, Park SM, Yoon TY, Yoon SJ. A case of hepatitis after occupational exposure of trichloroethylene. Korean J Hepatol. 1999. 5:59–64.
18. Kang S, Chae H, Lee N. Report of an epidemiological survey in a Korean overseas affiliated company in the Philippines. 1999. Incheon: Occupational Safety and Health Institute, Korea Occupational Safety and Health Agency;1–9.
19. Chae HJ, Lee SK, Lee KJ, Kim JY, Lee SC, Shin DH, Moon JD. Exfoliative dermatitis and toxic hepatitis associated with occupational exposure to trichloroethylene. Korean J Occup Environ Med. 2003. 15:111–117.
20. Lee SW, Kim EA, Kim DS, Koh DH, Kang SK, Kim BK, Kim MK. Exposure level of trichloroethylene in Stevens-Johnson syndrome due to occupational exposure: 3 case reports and a review of other cases. Korean J Occup Environ Med. 2008. 20:132–146.
21. Phoon WH, Chan MO, Rajan VS, Tan KJ, Thirumoorthy T, Goh CL. Stevens-Johnson syndrome associated with occupational exposure to trichloroethylene. Contact Dermatitis. 1984. 10:270–276.
22. Lim HS, Ahn YS. Occupational diseases among health care workers approved by Korea Labor Welfare Corporation. Korean J Occup Environ Med. 2003. 15:196–204.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download