Abstract
The purpose of this article was to provide a literature review of occupational neurological disorders and related research in Korea, focusing on chemical hazards. We reviewed occupational neurological disorders investigated by the Occupational Safety and Health Research Institute of Korean Occupational Safety and Health Agency between 1992 and 2009, categorizing them as neurological disorders of the central nervous system (CNS), of the peripheral nervous system (PNS) or as neurodegenerative disorders. We also examined peer-reviewed journal articles related to neurotoxicology, published from 1984 to 2009. Outbreaks of occupational neurological disorder of the CNS due to inorganic mercury and carbon disulfide poisoning had helped prompt the development of the occupational safety and health system of Korea. Other major neurological disorders of the CNS included methyl bromide intoxication and chronic toxic encephalopathy. Most of the PNS disorders were n-hexane-induced peripheral neuritis, reported from the electronics industry. Reports of manganese-induced Parkinsonism resulted in the introduction of neuroimaging techniques to occupational medicine. Since the late 1990s, the direction of research has been moving toward degenerative disorder and early effect of neurotoxicity. To understand the early effects of neurotoxic chemicals in the preclinical stage, more follow-up studies of a longer duration are necessary.
The nervous system is particularly susceptible to the effects of exogenous toxins because of its high metabolic rate. With the advent of industrialization in Korea in the 1960s came an increased use of chemicals in the workplace. As a result, several kinds of neurological disorders have been reported as occupational diseases.
Hardly any official records on occupational neurological disorders existed before the 1990s. Prior to the 1990s, there were two important outbreaks of occupational neurological disorder in Korea. One of them was an outbreak of inorganic mercury intoxication from fluorescent lamp manufacturers (1) and thermometer manufacturers (2). The other was an outbreak of carbon disulfide intoxication, reported in 1987 (3), which resulted in 950 cases of occupational disorders, including neurotoxic diseases, and lasted until 2000 (4). These outbreaks called for the establishment of an occupational safety and health system by the Korean government (5).
Most official records of occupational diseases in Korea came from the Korea Workers' Compensation and Welfare Service (COMWEL), which is a public insurance system for workers. Because there were not detailed classifications for diseases in this system, it is difficult to know the scale of occupational neurological disorders in Korea. Since 1992, the Occupational Safety and Health Research Institute (OSHRI) of Korean Occupational Safety and Health Agency (KOSHA) have been conducting an epidemiological investigation for occupational diseases, which found 12 cases of neurologic diseases between 1992 and 1999 (6). Various kinds of neurotoxic disorders, such as chronic toxic encephalopathy by solvent (7), peripheral neuropathy by n-hexane (8), and amyotrophic lateral sclerosis (9) as well as Parkinsonism (10) induced by toxic metals, were reported from the investigations by OSHRI and academics.
Parkinsonism in welders exposed to manganese (Mn) were reported in 1998 (10). In contrast to previous Parkinsonism cases resulting from the exposure to high levels of Mn (11), the exposure level of welders reported in Korea were low. These cases evoked an attention from academics on the long-term effects of low-level exposure to neurotoxic chemicals. Studies of the low-level, long-term effects of neurotoxins provided tools by which subtle, pre-clinical effects on the neurological system could be detected. The World Health Organization-recommended the Neurobehavioral Core Test Battery (WHO-NCTB) was introduced into Korea in the early 1990s and has been applied to the study of workers exposed to neurotoxic chemicals (12). In this study, we reviewed occupational neurological disorders reported in Korea.
Although various non-chemical hazards can affect neurological functioning, this study focused mainly on chemical hazards, because disorders caused by non-chemical hazards such as direct trauma, heat stress, decompression, or vibration are reviewed by other papers in this issue. We reviewed occupational neurological disorders investigated by OSHRI during the period of 1992 to 2009. We categorized occupational neurological disorders according to the anatomical classification of the human nervous system, as neurological disorders of the central nervous system (CNS), of the peripheral nervous system (PNS) or as neurodegenerative disorders. The etiological hazards, both industry and job specific, were reviewed for each disorder.
In the cases of solvent-induced chronic toxic encephalopathy, we subdivided them into the categories of solvent-induced CNS disorders developed by the International Solvent Workshop (ISW) (13) and the World Health Organization (WHO)/Nordic Council of Ministers (14). Peer-reviewed journal articles and publications of OSHRI-related neurotoxicology, published from 1984 to 2009, including case reports, nationwide epidemiological studies, and preclinical neurotoxic agents, were reviewed.
Three major outbreaks of neurotoxic disorders that have occurred in Korea were CNS disorders, resulting from substances such as inorganic mercury (1, 2, 15-19), carbon disulfide (3, 20-22), and methyl bromide (19, 23-25). The other causes of occupational CNS disorders were organotin (26, 27), acetonitrile (19), and carbon monoxide (28). In addition, several chronic toxic encephalopathy cases (7, 19, 24, 25, 29-31) due to mixed solvents had been reported (Table 1).
Reports of inorganic mercury intoxication in Korea began in 1985 when a woman employed at a thermometer manufacturer was diagnosed as having an organic mental disorder (15). She was 16-yr-old and had been working in the inspection and packing division. Two months later after she started working for the thermometer manufacturer, she showed erythematous rushes on her skin. Subsequent to that symptom, she developed hand tremor, convulsion and dysarthria. During the mental examination, she was diagnosed with depression, anxiety and generalized cognitive dysfunction, such as memory loss and decreased concentration.
In 1987, an epidemic from a fluorescent lamp manufacturer occurred when 18 out of the 25 workers at the manufacturer tested for more than 0.03 µg/mL of serum mercury concentration (1). At the factory, four cases of chronic mercury poisoning were reported (17). The workers had been working between 15 months and 7 yr, showing symptoms of tremor, dysarthria, anxiety, memory loss, decreased concentration, insomnia and gingivitis. After chelating treatment with D-penicillamine and British Anti-Lewisite (BAL) in the hospital, all workers recovered. A second report of inorganic mercury poisoning from the company included 6 male patients (16, 18), with 2 patients overlapping with the initial report (17). In the second report, the exposure level of airborne mercury was 0.005-0.144 mg/m3 (16).
In June 1988, a 15-yr-old boy, who had been working for 2 months in a precision instrument manufacturer located in Seoul, died (2). He had shown severe neuropsychiatric symptoms: anxiety, hallucination, inappropriate affection, articulation impairment, hand tremor, convulsion, insomnia and memory loss. The airborne concentration of mercury was 0.02-0.24 mg/m3. After this accident, as serious concerns began to be expressed by non-governmental organizations, the epidemiological investigation of mercury-exposed workers was conducted by Korea University on the request of the Ministry of Labor (5). During the investigation, special medical examinations were performed on 134 workers in 18 mercury-handling workplaces, and 27 (20%) were found to be suffering from mercury poisoning.
There were no more outbreaks of mercury poisoning until three cases of inorganic mercury intoxication were discovered in a waste treatment company in 2000 (19). Workers had extracted a silver compound from waste radiography film using inorganic mercury for about 1 month. The exposure level of airborne mercury was 0.03-1.235 mg/m3. All three workers showed pain in the arms and legs, memory loss and peripheral neuritis and had abnormal findings on magnetic resonance imaging (MRI). One showed hallucination and delirium and was diagnosed with brief reactive psychosis.
Nine out of 13 inorganic mercury poisoning cases showed neurological or psychiatric symptoms and signs (Table 2). Some showed the classic neurological signs of mercury intoxication, such as irritability (2 cases) and hand tremor (6 cases). Other symptoms, such as skin lesion, stomatitis and weight loss, were also reported in some cases.
Occupational carbon disulfide intoxication was diagnosed in 1981 (5) for the first time. In 1987, more employees who had worked for the previous 10 yr in the spinning process, making artificial silk thread from pulp dissolved in a carbon disulfide solution (3, 20-22), were diagnosed with carbon disulfide poisoning, turning into an outbreak that numbered a total of 950 victims by 2008 (4). The company was built by used machines imported from a viscose rayon company in Japan and started operation at 1966 (4). At the time, the number of employees reached 1,500 in the company but dwindled to 811 by the time it was closed down in 1993 (5).
The major characteristics of the carbon disulfide poisoning cases that developed in 1987 were CNS and PNS symptoms, which was well-described in 8 patients (3). Six of the 8 patients showed dysarthria, 5 showed hemiparesis, 5 showed organic brain syndrome, and all 8 workers showed polyneuropathy. The exposure duration was 6 to 18 yr (Table 3). The mean exposure level of the air concentration of carbon disulfide in the company was reported at 1.2-23.1 ppm (21). One study that evaluated the ex-employees of the rayon manufacturer reported that 61.5% and 15.4% of workers among the 117 chronic carbon disulfide poisoning patients had neurological disorders and psychiatric disorders, respectively (22).
Chronic toxic encephalopathy caused by mixed solvent was reported in 10 cases (7, 19, 24, 25, 29-31), including 3 female and 7 male workers (Table 4). All patients had been exposed to mixed solvents. However, toluene and trichloroethylene were the main components of the solvents. Because the exposure levels of the cases were measured only after the patients had been found and the work enviromment had been improved, the actual exposure level of the workers could be underestimated. Out of 10 cases, 4 patients could be classified as ISW category 3, and 2 patients could be classified as ISW category 2B. Two showed cerebellar syndrome and severe ataxia. One case of ISW category 3 from a footwear manufacturer showed a severe atrophic lesion on a brain MRI and had been exposed to a very high level of solvents--11.2 on the mixed solvent index (the reference level is 1.0).
All of 10 cases of methyl bromide intoxication were found in fumigation workers (19, 23-25) who had infused the pesticide into covered woodstacks or a container in which agricultural goods had been kept (Table 5). The first case of methyl bromide intoxication, found in 2000, was a 20-yr-old man, working for fumigation for two months. Subsequently, three cases of methyl bromide intoxication were reported before 2001. In 2008, an outbreak of methyl bromide intoxication was reported in which 6 workers from a fumigation company showed CNS and PNS symptoms.
The airborne concentration of methyl bromide in the total of 10 cases ranged from an undetected level to 15.1 ppm as the Occurpational Exposure Level of Korea. In one company, where the short-term exposure level (STEL) was measured, the exposure level reached 28.8 ppm. The levels of bromide in serum and urine of the 10 cases were 11.7-39.6 mg/L and 2.6-94.6 mg/L, respectively. All but one worker showed gait disturbance. Two showed objective findings of polyneuropathy from electromyography. Five showed mild to diffuse lesions on a brain. The loci of brain lesions in the MRI were the cerebellum, midbrain, globus pallidus, olive, pons, periaqueductal white matter region, 4th ventricle and corpus callosum (Table 5).
A patient suffering from organotin poisoning (26, 27) had been working as a tank cleaner for several different companies in the previous eight years. He had cleaned a tank containing dimethyltin for four days. A day after finishing the job, he suffered decreased memory, behavioral changes and progressive mental deterioration when he arrived at the emergency room. The result of spinal tapping was negative, but on the fourth day of admission, he deteriorated into a state of coma along with metabolic acidosis and severe hypokalemia. High levels of DMT and trimethyltin (TMT) were detected in a highly sensitive urine analysis.
Acetonitrile is the simplest organic nitrile and used in various industries. It can be metabolized to produce hydrogen cyanide, which is the source of the toxic effects (32). Two male pharmaceutical workers (37 and 38 yr old) had been exposed to acetonitrile dust during polymerization process since 1994 and were diagnosed with acute acetonitrile intoxication in 1995 (19). Both felt stiffness in their legs and arms, beginning after a few days of working at the process. In January 1995, they felt dizziness and severe fatigue after the polymerization. The next morning, both felt stiffness on the tongue, experienced nausea and vomiting and talked deliriously. They were admitted to the hospital and diagnosed with chemical-induced CNS disorder.
Carbon monoxide intoxication was found in an apartment building guard (male, 58 yr old), who had to sleep in the boiler room where the carbon monoxide was generated. His duties were the operation of the boiler and other security jobs in the apartment building. He was working in 24-hr shifts. The exposure level of carbon monoxide, which was measured in the outlet of the duct through which the exhausted gas was ventilated, was 103.2 ppm. In January 2006, he was discovered in the boiler room in an unconscious state. He was admitted to hospital and given a conservative treatment. One week after he discharged, he showed cognitive loss and motor dysfunction. He was admitted hospital again and diagnosed with delayed hypoxic encephalopathy (28).
The most commonly reported neurological disorder of the PNS was peripheral neuritis (Table 6). Among 15 cases of peripheral neuritis reported, 10 cases were caused by n-hexane and another case was exposed to 2,5-hexanedion, known for the metabolite of n-hexane (19, 33-35). Others included 3 cases of mixed solvent caused by peripheral neuritis (24, 28) and an acrylamide-induced case (36).
Fifteen cases of peripheral neuritis were reported by 2009 (Table 6). All cases but one of n-hexane-induced peripheral neuritis were reported from workers in the electronics industry, such as a LCD-frame manufacturer and a cellular phone manufacturer. A cleaning process using n-hexane was the most common job in these cases. Eight cases (from cases numbered 6 to 13) were an outbreak from an LCD frame manufacturer in 2005. Eight female workers whose job had been cleaning the LCD frame were discovered to have been exposed to 114.4-281 ppm of n-hexane; they were diagnosed with peripheral neuritis (35).
In 1999, the subclinical effects on nerve conduction velocity (NCV) were measured in the workers exposed to low-level n-hexane (8). The results from this study showed that chronic (mean exposure duration=15 yr) low-level (mean exposure level=23 ppm) exposure to n-hexane caused subclinical impairment of the peripheral nervous system.
Neurological disorders other than peripheral neuritis were anosmia (24, 37, 38), sixth cranial nerve palsy (19) and reflex sympathetic dystrophy (28). Anosmia was reported in workers using mixed solvent at a bicycle manufacturer (24), in two workers who were exposed to chloride at a train manufacturer (37), and in a worker who was exposed to metalworking fluid during the heat treatment of metal processing (38).
A patient suffering from reflex sympathetic dystrophy was exposed to pesticide while spraying it on a garden. He was using the organophosphorous pesticide for 3 days and accidentally splashed it on his body. One week later, he experienced decolorization of the skin, chronic pain and atrophy of the arm muscle (24).
Occupational cases of neurodegenerative disorder that had been reported in Korea were Mn-induced Parkinsonism and amyotrophic lateral sclerosis (ALS).
The classical description of Mn-induced Parkinsonism was in a report of Mn-mining workers at a refinery who were exposed to high levels of manganese (39). In Korea, however, the first report of Mn poisoning was reported from a welding rods manufacturer from crushing ferromanganese (40). Three cases of Mn-induced Parkinsonism, showing postural instability, gait difficulty and bradykinesia, had been working at the company for one to three years (Table 7).
After the report, most of the Mn-induced Parkinsonism cases in Korea were found in welders (10, 19, 28, 31). In 1998, three welders with more than 10 yr of welding experience were diagnosed with Mn-induced Parkinsonism (10). They did not match the classical appearance of Mn intoxication; however, their brain MRI showed high signal intensity in the basal ganglia area on T1-weighted film. Because welders were not considered at risk for serious Mn exposure before this report, large concern for Mn toxicity in Korean workers began, especially in the welders' union. The Ministry of Labor asked OSHRI for a nationwide investigation to clarify the clinical significance of increased signal intensities on T1-weighted MRI. The investigation examined 750 workers from welding, alloy furnace and welding-stick manufacturing. The neurobehavioral core test battery (NCTB) and signal change on brain MRI scan were conducted (41, 42). OSHRI did not discover any Parkinsonism or severe neurologically disabled cases out of the total subjects. The proportion of workers with increased signal intensities of T1 weighted image among the Mn-exposed workers was higher than among the non-exposed. In particular, 73.5% of the welders showed increased signal intensities. Because the intensities were not correlated with neurological lesions, the study concluded that high signals of brain MRI was not necessarily Mn-induced Parkinsonism, even if the patient had recent exposure to Mn (43). However, Mn exposure was significantly correlated with neurobehavioral performance on the NCTB (44, 45). This implied that, even though the signal changes of T1 weighted image on brain MRI were not an exact index for Mn-induced Parkinsonism, it might reflect the preclinical effects such as neurobehavioral performance.
By 2008, 8 cases of Mn-induced neurological disorders had been reported, including three workers from a welding rod manufacturer (40), 4 welders (19, 31, 42) and 1 painter (46) (Table 7). The working duration of the 8 cases, aged 39 to 51 yr old, was 15 months to 15 yr. Most showed one of the major characteristics of Parkinson's syndrome. All of the welders but one had shown high signal intensity of T1 weighted image on a brain MRI. One case was not related to Mn exposure but had been exposed to organic solvents during 13 yr of working. Even though several studies had been conducted to find a relationship between Parkinsonism and organic solvents (46), the relationship between the two is still inconclusive.
The reports on the three welders (10) and the nationwide investigation by OSHRI (42) provoked more studies on welders' brain MRIs and Mn exposure (47-50). These studies found that a high percentage of high signal intensity in Mn-exposed workers, however, could not confirm a correlation between the intensity of MRI and objective neurological signs. Kang et al. (48) reported that the signal intensity of the globus pallidus on a brain MRI was a suitable single variable representing the effect of Mn accumulation in the CNS; however, it would be of limited value without the neuropathological index. In 2007, Kim et al. (51) analyzed the data from an epidemiological investigation by OSHRI using structural equation modeling; they reported that airborne Mn contributed to the pallidal index (PI) of a brain MRI and that the PI is the most effective predictor of neurobehavioral performance, after adjusting for age and level of education. These findings were confirmed by Shin et al. (52), supporting the cut-off line of the PI index value of 107.
Further evaluations of brain imaging techniques, such as 1H magnetic resonance spectroscopy (MRS) in welders, were conducted until 2007 (53, 54). In those studies, a N-acetylaspartate/creatine ratio of MRS in the basal ganglia seems to reflect the cumulative effects of Mn exposure on the human brain. There was one case-control study on Mn and Parkinson's diseases (PD). The result of this study was not able to find a correlation between exposure to Mn and Parkinson's disease (55).
ALS is a neurodegenerative disease affecting the motor neurons of the spinal cord and brain. Although the definite etiology of ALS remains unclear, occupational or environmental exposure has been considered as one of the potential causes of ALS. In Korea, 2 cases of ALS have been reported (9, 19). A patient had been working as a spray painter at an industrial machine manufacturer for 20 yr (19) and was diagnosed with ALS. Other cases were 39-yr-old male workers from an electronic parts manufacturing company, reported to be related to lead exposure (9).
With the aim of detecting earlier changes in neurological function in the workers who were exposed to neurotoxic chemicals, several studies had been conducted since early 1990. At first, these efforts concentrated on developing a questionnaire about subjective symptoms (56, 57). Since 1993, the WHO-NCTB was introduced into the study of neurotoxicity of workers who were exposed to mixed solvents to determine the applicability of the tool (58). Because the WHO-NCTB was not an electronic device, there have been requested for more standardized tools for a neurobehavioral test. Since 1994, a computerized tool that had been developed by Korean researchers was used instead of the WHO-NCTB (59, 60). The computerized test battery, called the Korean computerized neurobehavioral system (KCN), acquired validity and reliability through verification, testing intercultural difference (61) and difference between the computerized test and the non-computerized test (62, 63). Another computerized neurobehavioral battery, called the Behavioral Assessment and Research System (BARS), was also introduced in Korea and applied to Korean workers (64).
This study reviewed occupational neurological disorders reported in Korea since the late 1980s. The major occupational disorders in Korea are pneumoconiosis (8.2%), cardio-cerebral-vascular disorder (8.3%) and musculoskeletal disorder (76.9%) (65). Although counts of occupational neurological disorder compose only a small part of the overall occupational disorders, it has had a significant impact on the occupational safety and health system of Korea.
Research on occupational neurological disorder in Korea gained momentum after the outbreak of inorganic mercury poisoning and carbon disulfide intoxication in the late 1980s. Particularly, the outbreak of carbon disulfide intoxication was the most influential event in history of occupational disorders in Korea, resulting in more than 950 occupational disease patients (4). Because one of the major target organs of carbon disulfide and inorganic mercury is the neurological system, many researchers started to be interested in occupational neurotoxic disorders. After the carbon disulfide outbreak, Korean government paid more attention to developing the legal system of occupational safety and health as well as a chemical management system in the workplace (4).
Ten of the 13 cases of inorganic mercury poisoning were reported before 1990. Among the 10 cases, three were teenagers, who showed severe neuropsychiatric symptoms and signs. In the past, it seemed that the Ministry of Labor's supervision of the workplace did not prevent child labor in dangerous working environments. Furthermore, the chemical information, including neurotoxicity, was inadequate until the material safety data sheets (MSDS) system was introduced in 1997. Therefore, most neurotoxic disorders until the middle 1990s were related to exposure to high concentrations of chemicals.
Nowadays, high exposure to organic solvents, including n-hexane, is not common, due to workplace improvements in Korea, by the reinforcement of the legal system in occupational safety and health. Thus, the classical chronic toxic encephalopathy case with high exposure to organic solvents is rarely found any longer. Some cases of chronic toxic encephalopathy patients reported in this study were found in those companies where the organic solvent level was relatively high. The diagnosis of chronic toxic encephalopathy was dependent on diagnostic criteria and the assessment of the cumulative exposure to solvents. Only one case among the chronic toxic encephalopathy cases reported in this study were categorized as ISW category 1 (Table 4). Because the symptoms and signs are nonspecific and mild, it would be difficult to diagnose chronic toxic encephalopathy in ISW category 1. To solve the difficulty, researchers have been developing diagnostic tools such as neurobehavioral test batteries.
Most of the cases of n-hexane intoxication were reported in the electronics industry (Table 6). Because of the expansion of the electronics industry in Korea, the usage of n-hexane was concentrated in the industry. The exposure level of n-hexane was to be reported as less than 10 ppm in some cases (Table 6). However, most of the patients worked in cleaning jobs, which is a manual handling process, and the exposure level of n-hexane could be high for those workers. Some cases of polyneuritis developed by mixed solvents, including various organic solvents, which implied that with long-exposure duration, not only to n-hexane but to other solvents, could also affect the peripheral nervous system (Table 5). Therefore, as with chronic toxic encephalopathy, researchers should consider that peripheral polyneuritis might be related to long-term, low-level exposure to mixed chemicals.
There are a few blind spots for occupational health management in Korea, such as service industries using chemicals where the exposure level cannot be properly controlled. All of the cases of methyl bromide intoxication had resulted in serious lesions on the CNS (Table 5). Because the fumigation process is irregular, the workers had not been notified about personal protective equipment before using this chemical. Many workers in this industry were temporary workers, and the workers were not informed of the toxicity of methyl bromide.
Recently, studies on neurotoxicology in Korea have begun to consider the early effects of neurotoxicity. In this view, Mn-induced Parkinsonism had an important impact on the studies of occupational health in Korea. This new line of inquiry addressed the problem regarding long-term, low-level exposure. Even if the exposure level to Mn is lower than the proposed level, the accumulation of these effects can result in neurotoxic diseases, like Parkinsonism. Since the mid-1990s, there have been many studies on neurobehavioral tests to detect the early effects of toxic chemicals (12). Neurobehavioral tests on the workers exposed to neurotoxic chemical continued to be performed, resulting in the development of a new computerized battery of a neurobehavioral test for Korean workers (63).
Because the industrial development of Korea began in the 1960s, and the use of chemicals in workplace was expanded during the 1970s to 1980s, many cases of neurotoxic disorders were underreported. Few chemicals, such as carbon disulfide, n-hexane, acrylamide, trichloroethylene, methyl bromide, lead and Mn, were found to be the cause of occupational neurological disorder in Korea. However, in 2007, 229,262 and 265,827 workers had reported to have been exposed to organic chemicals and toxic metals, respectively (66). In Korea, 177 kinds of chemicals were listed in the Occupational Safety and Health Act that employers should control in their workplace; 41% (73 kinds) of the chemicals on the list have neurotoxicity (67). Therefore, there might be even more occupational neurological disorders that have not been reported.
Since the early 1980s, many studies have been conducted on occupational neurological disorders in Korea. Most of the studies have been reported on overt neurotoxicity which has specific symptoms and signs such as carbon disulfide intoxication, mercury intoxication, and n-hexane induced peripheral neuritis. Since the late 1990s, the direction of researches has been moving toward degenerative disorder and early effect of neurotoxicity. Majority of them were cross-sectional studies, and cohort or case-control studies were not conducted at all, except for one study on Parkinson's disease and Mn (55). To understand the early effects of neurotoxic chemicals in the preclinical stage, more follow-up studies of a longer duration are necessary.
Figures and Tables
Table 3
Characteristics of the reported cases of carbon sulfide neurotoxicity
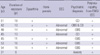
Source from Kim et al. (3).
EEG, electrocephalography; EMG/NCV, electromyography and nerve conduction; CD, conversion disorder; OBS, organic brain syndrome. All of the cases were male.
Table 5
Methyl bromide intoxication in the fumigation industry

*TLV-TWA (ppm); †mg/L.
aSTEL (Short term exposure level), Because of the case no 5-10 were from the same company, thus, they had the same ambient methyl bromide level and bromide in urine and serum. All the cases were male.
MRI, magnetic resonance imaging; EMG, Electromyography test; ND, not detected; -, not available; Ref, reference; Year, the reported year.
References
1. Hong YC, Kim BS, Kim JY, Lee JK, Huh BY, Choi CJ. An epidemiological survey on mass outbreak of mercury poisoning in a fluorescent lamp manufacturing factory. J Korean Acad Fam Med. 1988. 9:13–19.
2. Park HS, Lim HS, Huh BL, Han HK, Hwang YS, Moon HR, Hong KY. A case report of a fatal mercury poisoning. J Korean Acad Fam Med. 1991. 12:66–71.
3. Kim SD, Song DB, Yum YT. Clinical analysis of 8 cases of chronic carbon disulfide poisoning in workers engaged in the viscose rayon industry. Korean J Occup Environ Med. 1989. 1:186–196.
4. Occupational Safety and Health Research Institute. Looking back Won-Jin rayon accident 20 years. OSH Res Brief. 2010. 32:8–34.
5. Park JS, Kim YH. The history of occupational health service in Korea. Ind Health. 1998. 36:393–401.
6. Kang SK, Kim KS, Kim Y, Choi JK, Ahn YS, Jin YW, Choi BS, Kim E, Chae CH, Choi YH. Analysis of claimed cases as an occupational disease at Korea Occupational Safety and Health Agency from 1992 to 1999. Korean J Occup Environ Med. 2000. 12:292–301.
7. Cheon YH. Toxic encephalopathy in a worker exposed to organic solvents; a case report. Korean J Occup Environ Med. 1991. 3:216–219.
8. Kim H, Park YJ, Lee SJ, Song J, Jang EC, Lee KY, Shim S. Effect of chronic exposure to low-levels of n-hexane on peripheral nervous system. Korean J Occup Environ Med. 1999. 11:350–360.
9. Oh SS, Kim EA, Lee SW, Kim MK, Kang SK. A case of amyotrophic lateral sclerosis in electronic parts manufacturing worker exposed to lead. Neurotoxicology. 2007. 28:324–327.
10. Hong YS, Lim MA, Lee YH, Cheong HK, Kim JY, Lim HS, Lee JJ, Sa KJ, Kim JY. Three cases of high signal intensity by brain magnetic resonance imaging in CO2 arc welders. Korean J Occup Environ Med. 1998. 10:290–298.
11. Martin CJ. Manganese neurotoxicity: connecting the dots along the continuum of dysfunction. Neurotoxicology. 2006. 27:347–349.
12. Kang SK. The applicability of WHO-NCTB in Korea. Neurotoxicology. 2000. 21:697–701.
13. Human aspects of solvent neurobehavioral effects. Neurotoxicology. 1986. 7:43–56.
14. WHO Nordic Council of Ministers. Organic solvents and the central nervous system, EH5. 1985. Copenhagen, Denmark: World Health Organization and Nordic Council of Ministers.
15. Jeong WS, Cheon JS, Chang JI. A case of organic mental disorder associated with subacute mercury poisoning. J Korean Neuropsychiatr Assoc. 1985. 24:167–172.
16. Jang MY, Yum YT. An intervention study on the outbreak of occupational mercury poisoning. Korea Univ Med J. 1989. 26:67–77.
17. Kim BS, Hong YC, Lim HS, Kim JY, Lee JK, Huh BL, Choi CJ. Four cases of chronic mercury poisoning. J Korean Acad Fam Med. 1988. 9:27–32.
18. Wee KS, Choi TS, Lee SJ, Cho WY, Kim HK, Choi WC. A clinical study of chronic mercury poisoning. Korean J Intern Med. 1990. 38:51–57.
19. Occupational Safety and Health Research Institute. Results of epidemiological investigation for occupational diseases, 2000. 2002. Incheon, Korea: Occupational Safety and Health Research Institute, Korea Occupational Safety and Health Agency.
20. Kim DS, Kim SS, Cha CW. A study of the peripheral neuropathy among the workers exposed to carbon disulfide. Korean J Prev Med. 1993. 26:282–292.
21. Choi JW, Jang SH. A review of the carbon disulfide poisoning experiences in Korean. Korean J Occup Environ Med. 1991. 3:11–20.
22. Kim BS, Choi HR, Won CW. Related factors of diagnosis of chronic carbon disulfide poisoning. Korean J Occup Environ Med. 1997. 9:1–11.
23. Lee HJ, Oh SW, Lee JS, Chae HJ, Moon JD. A case of polyneuropathy associated with methyl bromide intoxication. Korean J Occup Environ Med. 2007. 19:238–243.
24. Occupational Safety and Health Research Institute. Results of Epidemiological Investigation for Occupational diseases, 2001. 2002. Incheon, Korea: Occupational Safety and Health Research Institute, Korea Occupational Safety and Health Agency.
25. Occupational Safety and Health Research Institute. Results of Epidemiological Investigation for Occupational diseases, 2008. 2009. Incheon, Korea: Occupational Safety and Health Research Institute, Korea Occupational Safety and Health Agency.
26. Kim SH, Yoo CI, Kwon JH, Bae JH, Weon YC, Kim Y. A case of cerebellar dysfunction after acute organotin poisoning. Korean J Occup Environ Med. 2009. 21:289–292.
27. Kim YJ, Kim Y, Jeong KS, Sim CS, Choy N, Kim JC, Eum JB, Endo Y, Yoo CI. A case of acute organotin poisoning. Korean J Occup Environ Med. 2006. 18:255–262.
28. Occupational Safety and Health Research Institute. Results of Epidemiological Investigation for Occupational diseases, 2006. 2007. Incheon, Korea: Occupational Safety and Health Research Institute, Korea Occupational Safety and Health Agency.
29. Kim JH, Ryu SJ, Kim BG, Jhun HJ, Park JT, Kim HJ. A case of trichloroethylene intoxication with neuropsychiatric symptoms. Korean J Occup Environ Med. 2008. 20:54–61.
30. Kang SK, Rhee KY, Chung HK, Lee YJ. A case of demyelinating lesion in central nervous system due to organic solvents. Korean J Occup Environ Med. 1992. 4:110–117.
31. Occupational Safety and Health Research Institute. Results of Epidemiological Investigation for Occupational diseases, 2002. 2003. Incheon, Korea: Occupational Safety and Health Research Institute, Korea Occupational Safety and Health Agency.
32. World Health Organization. International Programme on Chemical Safety, Environmental Health Criteria 154. Acetonitrile. 1993. Geneva, Swiss: World Health Organization.
33. Cho SY, Jang YS, Choi EK, Kim JS, Yu JY, Woo KH, Choi TS. A case of peripheral polyneuropathy induced by occupational 2,5-hexanedione exposure. Korean J Occup Environ Med. 2007. 19:73–80.
34. Shin JY, Leem JH, Kim YK, Park SG, Lee JN, Kim HC, Kim CH, Cho KU, Jang M. A case of peripheral polyneuropathy occurring in a small enterprise processing mobile phone cases. Korean J Occup Environ Med. 2005. 17:138–143.
35. Occupational Safety and Health Research Institute. Peripheral neuritis of the workers from LCD frame manufacturer, 2005. 2005. Incheon, Korea: Korea Occupational Safety and Health Agency.
36. Cheong HK, Kwon YW, Uh KY, Kim BJ, Yang JS, Jung C, Jin Y, Lee MY, Kang SK. Polyneuropathy by occupational exposure to acrylamide. Korean J Occup Environ Med. 1998. 10:388–403.
37. Ku SM, Kim HJ. Two cases of anosmia suspected to be caused by chronic chlorine exposure in cleansing works. Korean J Occup Environ Med. 2005. 17:155–159.
38. Occupational Safety and Health Research Institute. Results of epidemiological investigation for occupational diseases, 2007. 2008. Incheon, Korea: Korea Occupational Safety and Health Agency.
39. Kim Y. Health Effects of manganese and some recent issues in manganese neurotoxicity research. Korean J Occup Environ Med. 2009. 21:87–105.
40. Lim Y, Yim HW, Kim KA, Yun IJ. Review on the manganese poisoning. Korean J Occup Health. 1991. 30:13–18.
41. Kim Y, Kim KS, Yang JS, Park IJ, Kim E, Jin Y, Kwon KR, Chang KH, Kim JW, Park SH, Lim HS, Cheong HK, Shin YC, Park J, Moon Y. Increase in signal intensities on T1-weighted magnetic resonance images in asymptomatic manganese-exposed workers. Neurotoxicology. 1999. 20:901–907.
42. Occupational Safety and Health Research Institute. Final report for epidemiological investigation on the manganese exposed workers, 1998. 1998. Incehon, Korea: Korea Occupational Safety and Health Agency.
43. Kim Y, Kim JW, Ito K, Lim HS, Cheong HK, Kim JY, Shin YC, Kim KS, Moon Y. Idiopathic Parkinsonism with superimposed manganese exposure: utility of positron emission tomography. Neurotoxicology. 1999. 20:249–252.
44. Kim KS, Kim YH, Jin YW, Kim EA, Yang JS, Kwon KR, Kim JW, Roh JH, Moon YH. Factors associated with psychoneurobehavioral outcomes in workers exposed to manganese. Korean J Occup Environ Med. 1999. 11:213–228.
45. Jin Y, Kim Y, Kim KS, Kim E, Cho YS, Shin YC, Chai C, Choi Y, Lee SH, Moon YH. Performance of neurobehavioral tests among welders exposed to manganese. Korean J Occup Environ Med. 1999. 11:1–12.
46. Lim Y, Yim HW, Kim KA, Yun IG. Review on manganese poisoning. Korean J Occup Health. 1991. 30:13–18.
47. Jo MH, Ryu HW, Kim EA. One case of Parkinson's syndrome in a shipyard painter exposed to mixed organic solvents. Korean J Occup Environ Med. 2009. 21:192–200.
48. Hong YS, Kim JI, Jung KY, Kim JY. Study on clinical significance of high signal intensity by brain magnetic resonance imaging in mild steel/arc welders. Korean J Occup Environ Med. 1999. 11:415–429.
49. Kang DM, Park HC, Son HS, Park JH, Lee YJ. The significance of increased signal intensity in MR Imaging among male welders. Korean J Occup Environ Med. 1998. 10:41–52.
50. Yim HW, Kim JH, Phee YG, Koo JW, Lee KS, Park CY, Lee JW, Han SR, Jang HS. An association between brain MRI and neurologic findings in welders exposed to manganese fume. Korean J Occup Environ Med. 1998. 10:161–171.
51. Kim GH, Lim HS, Yu SH. A study on manganese health hazards among experienced welders. Korean J Prev Med. 1998. 31:644–665.
52. Kim E, Kim Y, Cheong HK, Cho S, Shin YC, Sakong J, Kim KS, Yang JS, Jin YW, Kang SK. Pallidal index on MRI as a target organ dose of manganese: structural equation model analysis. Neurotoxicology. 2005. 26:351–359.
53. Shin YC, Kim E, Cheong HK, Cho S, Sakong J, Kim KS, Yang JS, Jin YW, Kang SK, Kim Y. High signal intensity on magnetic resonance imaging as a predictor of neurobehavioral performance of workers exposed to manganese. Neurotoxicology. 2007. 28:257–262.
54. Choi DS, Kim EA, Cheong HK, Khang HS, Ryoo JW, Cho JM, Sakong J, Park I. Evaluation of MR signal index for the assessment of occupational manganese exposure of welders by measurement of local proton T1 relaxation time. Neurotoxicology. 2007. 28:284–289.
55. Kim EA, Cheong HK, Choi DS, Sakong J, Ryoo JW, Park I, Kang DM. Effect of occupational manganese exposure on the central nervous system of welders: 1H magnetic resonance spectroscopy and MRI findings. Neurotoxicology. 2007. 28:276–283.
56. Park J, Yoo CI, Sim CS, Kim HK, Kim JW, Jeon BS, Kim KR, Bang OY, Lee WY, Yi Y, Chung SE, Kim Y. Occupations and Parkinson's disease: a multicenter case-control study in South Korea. Neurotoxicology. 2005. 26:99–105.
57. Cho SH, Kim SM, Kwon HJ, Yim YH, Lim HS. Development of an on site diagnostic tool to detect neuropsychiatric impairment due to chronic organic solvent exposure. Korean J Prev Med. 1993. 26:127–164.
58. Kwon HJ, Cho SH, Lim HS. Validity and reliability of data derived from questionnaire on neurobehavioral symptoms. Korean J Occup Environ Med. 1995. 7:21–27.
59. Kang SK, Chung HK, Hong JP, Kim KW, Cho YS. A study to the workers exposed to organic solvents by neurobehavioral tests. Korean J Prev Med. 1993. 26:210–221.
60. Chung JH, Kim CY, Sakong J. A computer-administered neurobehavioral evaluation of workers exposed to organic solvents. Korean J Occup Environ Med. 1994. 6:219–241.
61. Sa KJ, Chung JH. Effect on computerized neurobehavioral test performance of the car painters exposed to organic solvents. Korean J Prev Med. 1994. 27:487–504.
62. Chung JH, Sakong J, Kang PS, Kim CY, Lee KS, Jeon MJ, Sung NJ, Ahn SH, Won KC. Cross-cultural comparison of neurobehavioral performance in Asian workers. Neurotoxicology. 2003. 24:533–540.
63. Sakong J, Chung JH, Lee HY. Interrelation of neuropsychiatric symptom and neurobehavioral test among workers exposed to organic solvents. Korean J Occup Environ Med. 1997. 9:49–60.
64. Sakong J, Kang PS, Kim CY, Hwang TY, Jeon MJ, Park SY, Lee SJ, Won KC, Lee SB, Chung JH. Evaluation of reliability of traditional and computerized neurobehavioral tests. Neurotoxicology. 2007. 28:235–239.
65. Kang SK, Rohlman DS, Lee MY, Lee HS, Chung SY, Anger WK. Neurobehavioral performance in workers exposed to toluene. Environ Toxicol Pharmacol. 2005. 19:645–650.
66. Ministry of Labor. Statistics on occupational injuries and diseases. 2008. Gwacheon, Korea: Ministry of Labor.
67. Occupational Safety and Health Research Institute. Annual report of the special health examination for workers in 2007. 2009. Gwacheon, Korea: Ministry of Labor.
68. Occupational Safety and Health Research Institute. Practicial guideline for workers health examination. 2009. 2009. Incheon, Korea: Korea Occupational Safety and Health Agency.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download