This article has been
cited by other articles in ScienceCentral.
Abstract
The management system of occupational diseases in Korea can be assessed from the perspective of a surveillance system. Workers' compensation insurance reports are used to produce official statistics on occupational diseases in Korea. National working conditions surveys are used to monitor the magnitude of work-related symptoms and signs in the labor force. A health examination program was introduced to detect occupational diseases through both selective and mass screening programs. The Working Environment Measurement Institution assesses workers' exposure to hazards in the workplace. Government regulates that the employer should do health examinations and working conditions measurement through contracted private agencies and following the Occupational Safety and Health Act. It is hoped that these institutions may be able to effectively detect and monitor occupational diseases and hazards in the workplace. In view of this, the occupational management system in Korea is well designed, except for the national survey system. In the future, national surveys for detection of hazards and ill-health outcomes in workers should be developed. The existing surveillance system for occupational disease can be improved by providing more refined information through statistical analysis of surveillance data.
Keywords: Management System, Occupational Diseases, Surveillance, Fatal, Non-Fatal
INTRODUCTION
Workers' health may be protected by his/her own preventive behavior, despite numerous health hazards in the workplace. However, worker behavior is constrained by various workplace pressures such as working conditions, including what is considered to be accepted working behavior and overall morale of the working group. Based on the employment contract, every employer has a certain amount of control/power and the expectation that workers will follow work-related requests. This may lead to adverse health effects in workers; therefore, the Government has implemented regulations to protect worker health, such as the Occupational Safety and Health (OSH) Act.
Worker health can be affected by various health hazards in the workplace. Adverse health effects induced by unexpected incidents may present as occupational injuries, but occupational diseases can appear due to long term continuous exposure to harmful chemicals, dust, noise, etc. To prevent occupational diseases, it is important to manage worker health via health monitoring for early detection of abnormal conditions.
It is very important for worker health management to monitor the level of worker exposure to hazards in the workplace; for example, health check-ups including absorption of hazard materials, so called 'biological monitoring'. Noise levels in the workplace should also be measured in order to prevent worker's hearing loss. If a worker is exposed to high levels of noise, he/she should be transferred to another work area without noise or provided with proper personal protective equipment (PPE) such as earplugs, etc.
As above, information needed for workers' health management can be classified into three categories according to 3 questions: 1) What is the exact nature of the occupational hazards? 2) How much is the worker exposed to these hazards? 3) What health problems are induced by these hazards? These questions should be answered in order to manage workers' health effectively and efficiently.
Health management for workers is accomplished by two different strategies: 1) focusing on reduction of exposure to hazard factors in the workplace based on risk assessment using exposure information; 2) the provision of health care services and compensation for workers with adverse health effects. Recently, psychosocial factors such as work-related stressors have been included as hazard factors in the workplace, and health promotion activities have become an important component of worker health management before symptoms and signs of occupational diseases manifest.
In this article, we reviewed the various kinds of surveillance systems for occupational diseases in Korea and resultant data, and suggest reformation of the workers' health management system.
OCCUPATIONAL DISEASES SURVEILLANCE ACTIVITIES IN KOREA
There are various monitoring systems to detect occupational diseases. The workers' compensation insurance system is one of the old systems and ensures a worker's life and his/her family is secure after work-related accident. The second is the national survey on health status and experiences of occupational diseases.
Workers' compensation insurance report
Workers' compensation insurance has been continuously developing since 1960; in particular, its coverage has expanded from large-sized companies to small businesses. Now it is mandatory for all employees to be covered by workers' compensation insurance. During the early period of workers' compensation insurance, only traditional occupational diseases requiring the recuperation of 11 or more days were compensated, but now work-related diseases such as musculoskeletal disorder, cerebrovascular attack and cardiovascular attack requiring the recuperation of 4 or more days, may also be compensated.
Industrial accident is defined in the Industrial Accident Compensation Insurance Act, and occupational diseases are included as industrial accidents. Occupational injuries and illnesses can be covered by workers' compensation insurance as social insurance managed by the Korea Workers' Compensation and Welfare Service (COMWEL), supervised and funded by the Ministry of Employment and Labor (MOEL) Korea Government. Usually occupational illnesses have been classified as industrial accidents according to work relatedness. Work relatedness refers to work or the working environment causing occupational injuries and illnesses or occupational injuries and illness happening during work.
Data on occupational diseases compensated as industrial accidents are collected and analyzed by the Korea Occupational Safety and Health Agency (KOSHA). The OSH Act regulate employers to report occupational disease to MOEL at the time of onset. Statistics on occupational diseases in Korea include compensated cases and reported cases. The proportion of reported cases is very small (under 1% of total occupational diseases).
Workers' compensation insurance is operated by COMWEL. KOSHA collects compensated cases from COMWEL and reported cases from the MOEL, and produces official statistics on all occupational diseases. Until now, some workers have been excluded from workers' compensation insurance:
Self-employed, unpaid family workers
Civil servants, teachers, soldiers
Agriculture, hunting, fishery, and forestry workplaces with less than 5 workers
Civil servants, as government employees, teachers and soldiers are covered by other insurance systems, while there is no compensation system for self-employed and unpaid family workers and workers of small companies in agriculture, hunting, fishery and forestry.
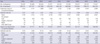
Since 2000, the number of occupational diseases has increased continuously from 4,051 in 2000 to 11,472 in 2007. However, after 2007 occupational disease cases decreased. In particular, occupational diseases accounted for 8,721 cases in 2009, representing a decrease of 1,013 persons (10.4%) compared to the previous year's 9,734 persons in 2008 (
1) (
Fig. 1).
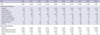
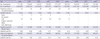
Among non-fatal occupational diseases, the percentage of work-related diseases was 70-80% in each year. The number of non-fatal work-related diseases stood at 6,626 in 2009, representing a decrease of 944 (12.5%) compared to the previous year's 7,570 persons. The increasing trend in the number of pneumoconiosis cases reversed to a decreasing trend in 2005. Non-fatal work-related diseases increased continuously until 2007, but recently statistics have shown decreasing trend. Specifically, brain and heart disease frequency have decreased since 2004 (
1) (
Table 1).
The number of fatal occupational diseases increased until 2003, but has since shifted to a decreasing trend. There is also a steadily increasing trend in fatal pneumoconiosis, while brain and heart disease cases have decreased.
Yearly trends in size of occupational diseases as industrial accidents in Korea may be reflected by changes in institutions of industrial accident compensation. In particular, brain and heart disease and musculoskeletal disorders have increased since the 1990s and 2000s, respectively. Recently, these work-related diseases were the most of compensated cases except for coal worker's pneumoconiosis (
Table 1,
2).
National survey report
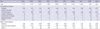
Another method of investigation of the magnitude and profile of occupational diseases is the national survey method; however, this method is less developed. Since 1998, there were three kinds of nationwide surveys: first, is the National Workers' Health Interview Survey; second, is the National Survey on Workplace Safety and Health Management; and third, is the Working Conditions Survey (WCS). The first one was done only one time in 1998 for workers in manufacturing sectors. The second one was done a total of 5 times between 2000 and 2008, and the sixth survey was done in 2009. The third one was conducted in 2006 and focused on psychosocial factors of workers' health in the workplace. This survey was based on the benchmark European Foundation's WCS. In 2010, the Working Conditions Survey is using the same questionnaire as the fifth survey of the European Founplace WCS in order to compare Korea and the EU. Every survey has included some questions about worker's experiences of occupational disease. According to the WCS, the magnitude of occupational diseases experienced as symptoms and signs is detailed hereafter: among the various symptoms and signs, the highest prevalence rate is that of musculoskeletal disorders (18.1%); the second most frequent is that of stress (17.9%); back pain is the third (16.8%); and overall fatigue is the fourth (16.7%). Prevalence rates of symptoms and signs are different between male and female workers. The prevalence rate of stress is the highest one among male workers, but musculoskeletal disorders are the highest among female workers (
2) (
Table 3).
HEALTH EXAMINATION SYSTEM
In Korea, there are some institutions for worker health management. These institutions are examine workers by the request of employers based on the OSH Act mandatorily. For example, health examinations are regulated by Government in order to protect worker health through early detection of occupational diseases. Health examinations for worker health protection are classified into two different types: Special Health Examination and General Health Examination. The Special Health Examinations are comprised of health screening tests for early detection of selective occupational diseases in workers exposed to specific hazard factors such as noise, dust, organic solvent, etc. The General Health Examination is a mass screening test for finding health problems including occupational diseases of workers without exposure to hazard factors.
The health examination is focused on early detection of occupational diseases, and its results are used as information for workplace management in order to protect worker health. Cases diagnosed as 'suspicious cases of occupational disease' are recommended to be transferred to non-hazardous workplaces. Some of them may be compensated based on diagnosis of occupational diseases through the workers' compensation insurance system.
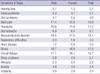
Detection rate of 'suspicious cases of occupational diseases' in the Special Health Examination was 0.46% in 2008, an increase from 2006. The detection rate of 'cases observed for occupational disease' was 12.85% in 2008 with an increasing trend. The health examination is defined as a screening test for occupational diseases, so there is no confirmatory diagnosis in the health examination process.
'Cases to be observed for occupational diseases' are the result of an examination showing marginal figures for 'suspicious cases for occupational diseases'. Based on results from the health examination, suspicious cases will be recommended to undergo medical treatment, change jobs or tasks for reduction of exposure to hazard workplace, etc. Cases to be observed are not in need of any immediate intervention; however, these cases may be also recommended similar treatment, such as wearing personal protective equipment (PPE), changing jobs or tasks, etc. Among suspicious cases and cases to be observed detected by the Special Health Examination, hearing loss due to noise was the most prevalent (
3) (
Table 4).
Detection rate of 'suspicious cases of occupational diseases' during the General Health Examination was 0.001% in 2008, and has been very steady since 2004. In contrast, the detection rate of 'suspicious cases of general diseases' has shown fluctuations between 4 and 5% in the last ten years (
3) (
Table 5).
Health examinations are very effective in finding asymptomatic chronic diseases, such as pneumoconiosis, hearing loss and some poisonings. However, it can barely detect symptomatic diseases with no signs, like asthma, and easily curable diseases like dermatitis because of the characteristics of the periodic screening test. Employers are also very reluctant to reveal and report occupational diseases. Therefore, statistics from the health examination include mostly pneumoconiosis and noise-induced hearing loss (
4) (
Table 4).
MONITORING SYSTEM FOR WORKER HAZARD EXPOSURE
The Working Environment Measurement Institution, regulated by the OSH Act, is in charge of assessing and, ultimately, reducing the level of worker exposure to hazard factors in the workplace. Every employer should do working environment measurement in order to identify hazard factors in the workplace and the level of worker exposure to these factors. The Special Health Examination is based on working environment measurement, such as selection of the examinee. If the level of worker exposure is higher than the Occupational Exposure Level in Korea, the employer should immediately act to reduce it.
DISCUSSION
The magnitude of occupational diseases and associated fatality rate in Korea have gradually increased since 2007. The reason may be the expansion of workers' compensation insurance coverage. The trend in fatality rate can be reflected by the trend in fatal pneumoconiosis and brain and heart disease, as these two categories of occupational diseases predominate total occupational diseases. Most pneumoconiosis cases were coal workers' pneumoconiosis; however, nowadays most coal mines have closed due to restructuring of the energy production system in Korea. Fatal cases of pneumoconiosis can be from old cases of coal workers' pneumoconiosis. The future trend of fatal pneumoconiosis will most likely be downward. Other dominant fatal occupational diseases, such as brain and heart diseases, will also decrease because general health programs have focused on prevention of hypertension, one of the most important causal factors of brain and heart diseases in workers. In the general population, the morbidity rate of brain and heart diseases has shown a recent downward trend.
Management of occupational diseases may be focused on two different targets. One is the causal factors of occupational diseases for prevention, and the other is affected workers of occupational diseases in order to rehabilitate them through recovery of the labor force.
Occupational diseases are induced by worker exposure to various hazard factors in the workplace, such as physical, chemical, biological and psychosocial factors. Workers with abnormal conditions can detect acute occupational diseases through self-diagnosis just after exposure to high levels of hazard factors, such as lead, mercury, etc. However, it is not so easy to identify abnormal conditions of chronic occupational diseases, such as asbestos-induced diseases. Furthermore, exposure to low levels of hazard factors may have long-term cumulative effects on worker health (
Fig. 2).
Occupational diseases are defined as ill-health due to work and work environment. If there is no evidence of work-relatedness, no ill-health can be confirmed as an occupational disease. Work-relatedness may be classified into two different types: direct and indirect causality. First, based on direct causality between work or work environment and ill-health, it is easy to determine work-relatedness, but it is very difficult to evaluate indirect work-relatedness. The same condition diagnosed as occupational disease by a physician can also be categorized as non-work-related because a particular hazard factor cannot be detected in the working history. Final determination of work-related illness or death in any individual case requires detailed occupational and non-occupational information (
5). In the United States, there exists occupational health surveillance, such as death certificates, hospital discharge data, physician reports, laboratory reports, workers' compensation reports, national surveys, employer surveillance programs and occupational health clinics (
5).
Since 1998, there were some suggestions for the introduction of a surveillance system for occupational diseases in Korea because worker health examinations and work environment measurements had limitations for management of occupational diseases (
6,
7). The magnitude of occupational diseases in Korea is assessed mainly by the workers' compensation system. Statistics might exclude unclaimed occupational diseases and those of workers from the public sector and workers who are not covered by compensation insurance (
4). This means that non-compensated cases can be neglected and latent cases can always emerge as compensated cases in the immediate future. Moreover, statistics based on compensated cases of occupational diseases are not stable because different acceptance criteria for work-relatedness have been applied by the Korea Labor Welfare Corporation (former name of COMWEL) and Judiciary Branch (
8). In Korea, there are two different kinds of health insurance: national health insurance and workers' compensation insurance. Every worker with occupational ill-health can be covered by either of these two. If some occupational diseases cases are covered by the national health insurance system, official statistics on occupational diseases cannot include these cases. In order to determine the correct number, all occupational diseases covered by the two different insurances must be detected. Unfortunately, the national health insurance system has no screening and confirming system for occupational diseases. This limitation should be solved by integration of the two social insurance systems.
Management of occupational diseases should focus on three stages of prevention. Occupational disease compensation will focus on the treatment, compensation, and rehabilitation as secondary or tertiary prevention. Primary prevention of occupational diseases is based on only the health examination system. National surveys of worker health can provide useful information about ill-health workers without treatment or compensation. This information can be used to prevent occupational diseases by detection of at-risk workers as a target population for management of occupational diseases.
Occupational hazard surveillance is the monitoring and analysis of data characterizing workplace exposures. The primary prevention of occupational diseases and injuries depends more directly on hazard surveillance, since the identification of hazards enables their reduction prior to the onset of ill-health. Occupational health surveillance is less well developed than its health counterpart due to scarcity of data sources and, with the exception of the Occupational Safety and Health Administration and the National Institute for Occupational Safety and Health surveys in the USA, the proprietary and inaccessible nature of hazard data collected by employers (
5).
Occupational health surveillance entails the systematic monitoring of health events and exposures in working populations in order to prevent and control occupational hazards and their associated diseases and injuries (
5). Medical surveillance refers to the ongoing application of medical tests and procedures to individual workers who may be at risk for occupational morbidity to determine whether an occupational disorder may be present (
5). If an individual or population is exposed to a toxin with known effects, and the tests and procedures are highly targeted to detect the likely presence of one or more effects in these persons, then this surveillance activity is more aptly described as medical screening (
9).
In occupational health, there are two kinds of surveillance activities, one is public health and medical surveillance and the other is hazard surveillance. The main purpose of occupational health surveillance is to identify the incidence and prevalence of known occupational diseases and injuries (
5). A second broad function is to identify individual cases of occupational disease and injury in order to find and evaluate other individuals from the same workplaces who may be at risk for similar disease and injury. Another purpose of case identification may be to assure that the affected individual receives appropriate clinical follow-up, an important consideration in view of the scarcity of clinical occupational medicine specialists (
10,
11). Finally, occupational health surveillance is an important means of discovering new associations between occupational agents and accompanying diseases. Discovery of rare diseases, patterns of common diseases, or suspicious exposure-disease associations through surveillance activities in the workplace can provide vital leads for a more conclusive scientific evaluation of the problem and possible verification of new occupational diseases (
5).
Periodic medical screening and surveillance examinations are another frequent service provided by occupational medicine physicians. The term screening focuses on the individual; screening tests are tools for secondary prevention with the goal of early diagnosis and treatment of disease in exposed workers. True 'surveillance' aggregates information about individuals in order to examine patterns within a population. Properly applied, surveillance is a tool for primary prevention through the identification and elimination of the cause of disease (
12). Screening examinations may be target-organ specific or substance specific, and thus tend to be more focused than preplacement evaluations (
12-
14).
CONCLUSION
Based on considerable information, occupational disease management can be accomplished in order to protect and promote worker health. Many kinds of information are required to suggest the etiology of poor worker health, such as hazard, exposure level and related information in workplace. The present system of surveillance for management of occupational diseases mainly depends upon the workers' compensation and health examination systems. These two systems cannot cover all kinds of occupational diseases. In order to focus on primary prevention of occupational diseases, various data sources on hazards and exposure levels in workplaces should be collected by a new surveillance system. Especially, prevention of occupational diseases may be focused on the reduction of worker exposure to the occupational hazards. The workers' compensation insurance system reviews each claim case for evaluating its work-relatedness. This means that hazard factors and worker exposure to those hazard factors may be assessed. These review data can be some of the most important information for prevention of ill-health by surveillance.
Most of the current surveillance system in Korea depends upon the OSH Act. From the viewpoint of surveillance, the occupational management system in Korea is well designed except for the national survey system. In the future, national surveys for detection of occupational hazards and ill-health outcomes of workers should be developed. The existing surveillance system of occupational disease can be improved by providing more refined information through statistical analysis of surveillance data. Recently, data mining has been used in order to estimate the national burden of occupational disease with other international statistics. In Korea, this technique can be also introduced for development of the management system of occupational diseases.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download