Abstract
We evaluated the recent trend in the incidence of premalignant and malignant skin lesions between 1991 and 2006. Among 571,057 newly registered dermatology out-patients from our 8 affiliated university hospitals, 2,598 were diagnosed with a premalignant (899, 0.16%) or malignant skin lesions (1,699, 0.30%). Of 899 premalignant cases, 71.2% were actinic keratosis (AK), and 24.6% were Bowen's disease. Of 1,699 malignant cases, 46.2% were basal cell carcinoma, followed by squamous cell carcinoma (19.1%) and melanoma (7.1%). This 16-yr survey was divided equally into two time periods to compare the incidence of premalignant and malignant skin lesions at different time settings. Between 1991 and 1998, the incidence of cutaneous premalignancy was 0.10% which doubled during 1999-2006. For cutaneous malignancy, the incidence was 0.25% during 1991-1998 and 0.34% in 1999-2006. Incidence of AK among the new outpatients was 0.07% in 1991-1998 which staggered up to 0.15% in 1999-2006. These findings show an increase of both premalignant and malignant skin lesions, AK in particular in the dermatology outpatient-based incidence.
The incidence of skin cancer is increasing worldwide (1-3). Non-melanoma skin cancers (NMSCs) constitute more than one-third of all cancers in USA with an estimated incidence of over 600,000 cases per year. The NMSCs are the most common malignancies occurring in the white population (3). The incidence of melanoma is much lower than that of NMSCs; but it is the most rapidly increasing cancer in the white population (3). Meanwhile, the incidence of skin cancers in Asians was thought to be relatively low compared to Caucasians. However, a number of epidemiologic studies from Korea and Japan show a gradual increase in incidence of skin cancers in East Asia (4-12).
Although a number of reports have been made on the incidence of premalignant and malignant skin lesions in Korea, most had limitation in terms of patient number and location (i.e, based a single hospital) (5-12). To observe the recent trend in the incidence of cutaneous premalignant and malignant lesions in Korea, we investigated 571,057 dermatology outpatients from 8 affiliated university hospitals in Korea through 1991 to 2006. This is the largest hospital-based survey made on cutaneous premalignant and malignant lesions in Korea.
The dermatology outpatient department of 8 affiliated university hospitals in Korea participated in this study. Three hospitals are located in Seoul, 4 in Gyeonggi-do Province (Uijeongbu, Bucheon, Bupyeong and Suwon), and one in Daejeon. This research was approved by the Institutional Review Board (IRB) of Seoul St. Mary's Hospital.
Incident cases of melanoma, NMSCs and premalignant skin lesions, newly diagnosed in the hospitals between January 1, 1991 and December 31, 2006, were identified by reviewing the patients' medical record. The primary outcome measures were the dermatology outpatient-based incidence values of premalignant and malignant skin lesions during the 16-yr period and the change in their incidence over 2 consecutive periods (1991-1998 and 1999-2006). The proportion of an individual skin lesion (actinic keratosis [AK], Bowen's disease [BD], basal cell carcinoma [BCC], squamous cell carcinoma [SCC] and melanoma) among the respective premalignant or malignant skin lesions was calculated over the 16 yr period as well as the 2 consecutive 8-yr periods. In addition, the patients' distribution in terms of age, sex and the anatomical location of the premalignant and malignant skin lesions was calculated for the period of diagnosis (1991-2006).
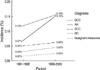
Among 571,057 newly registered outpatients (1991-2006) from the 8 affiliated university hospitals, 2,598 were diagnosed with either premalignant (899, 0.16%) or malignant skin lesions (1,699, 0.30%). We divided the 16-yr study period into two equal intervals (1991-1998 and 1999-2006) to compare the incidence of premalignant and malignant skin lesions among dermatology outpatients over time. The incidence of cutaneous premalignancies rose from 0.10% to 0.20% while that of malignant skin lesions rose from 0.25% to 0.34%. As for the individual disease entity, the incidence of AK among the dermatology outpatients was 0.11% (1991-2006), 0.07% (1991-1998) and 0.15% (1999-2006), respectively. The incidence of BD was 0.04% (1991-2006), 0.03% (1991-1998) and 0.05% (1999-2006). The overall incidence of BCC was 0.14% with 0.12% in the former 8 yr and 0.15% in the latter 8 yr. The incidence for SCC were 0.06% (1991-2006), 0.05% (1991-1998) and 0.06% (1999-2006), and for melanoma, 0.02% (1991-2006), 0.02% (1991-1998) and 0.03% (1999-2006) (Table 1, Fig. 1). The proportion of each of the major premalignant (AK, BD) and malignant skin lesion (BCC, SCC, melanoma) out of the respective premalignant and malignant cases were presented in Figs. 2, 3, over the whole 16 yr as well as the two consecutive 8 yr periods.
For both premalignant and malignant skin lesions, females outnumbered the male population (66.9% vs. 33.1% and 52.5% vs. 47.5%, respectively) (1991-2006). The female to male ratio of the individual disease were 2.9 for AK, 1.2 for BD, 1.1 for BCC, 1.4 for SCC and 0.9 for melanoma.
The age distribution of the individual skin lesion was examined. AK and SCC were most prevalent between the ages 71 and 80, and patients were most common in the 61-70 age group over the whole 16 yr for BD, BCC and melanoma. There was little difference in the peak age of the individual skin lesion between the former and latter 8 yr.
In terms of anatomical distribution, 73.4% of premalignant and 63.2% of malignant skin lesions occurred on the head and neck area, followed by the trunk (15.2% vs. 20.1%) and extremities (11.5% vs. 16.7%) (Figs. 4, 5). Within the head and neck area, the cheek was the most prevalent site for the premalignant lesion to appear (46.2%), followed by the forehead (15.5%), nose (10.0%), periorbital area (9.0%), lower lip (6.0%) and so on (Fig. 6). Within the head and neck, the nose was most commonly affected by a malignant skin lesion followed by the cheek (21.0%), periorbital area (13.8%), scalp (13.2%), and forehead (8.0%) (Fig. 7). For the individual disease entity, 94.7% of AK developed on the head and neck area, mostly on the cheek (43.7%), followed by the nose (10.1%), forehead (15.0%), periorbital area (8.3%), lip (6.9%), ear (4.6%), chin (2.0%), and neck (1.1%). 75.8% of BDs occurred on the trunk and extremities, especially on the legs (20.2%), followed by the hands and fingers (8.1%), back (9.0%), arm (4.0%), abdomen (7.6%), chest (7.6%), buttock (4.5%), genitalia (10.8%) and anus (1.4%). Among malignant tumors, 91.2% of BCCs and 70.6% of SCCs developed on the head and neck area. For BCCs, the nose was the most prevalent site (34.6%), followed by the cheek (15.9%), periorbital area (17.0%), scalp (7.5%), forehead (6.8%), ears (4.7%), lip (1.9%), neck (1.6%), and chin (1.3%). In SCCs, the cheek was the most prevalent site (22.3%), followed by the scalp (9.3%), lip (9.9%), nose (7.1%), forehead (7.1%), ears (6.8%), chin (3.1%), periorbital area (2.5%), and neck (2.2%). Melanoma preferred the extremities (66.9%), especially the feet (24.0%), followed by the fingers (12.4%), legs (10.7%), toes (8.3%), arms (8.3%), and hands (3.3%).
Based on the clinical records of dermatology outpatients from 8 affiliated university hospitals, a total of 571,057 cases were retrospectively reviewed. We believe this is the largest hospital-based study for premalignant and malignant skin lesions in Korea. The percentage of patients diagnosed with a premalignant skin lesion among the newcomers in the dermatology department was 0.10% during 1991-1998 but rose to 0.20% in 1999-2006. For malignant skin lesions, the incidence was 0.25% and 0.34%, respectively. Chung et al. (5) performed a similar study from 1982 to 1996 on both premalignant and malignant skin disease. The incidence of the premalignant skin lesions was 0.03% (1982-1986), 0.06% (1987-1991) and 0.11% (1991-1997) whereas that of the malignant skin lesions was 0.13% (1982-1986), 0.19% (1987-1991) and 0.36% (1991-1997). The incidence of premalignant skin lesions during 1991-1998 in our case (0.10%) was similar to that of Chung et al. (5) (1991-1997, 0.11%), but for cutaneous malignancies, our values were slightly lower (0.25% vs. 0.36%). However, in another study (6), the incidence of cutaneous malignancies during 1991-1998 was 0.14% which was lower than ours. A number of studies were performed from a single university hospital in Seoul at different time settings (8, 10, 11) where the reported incidence of both the premalignant and malignant skin lesions were substantially higher (premalignant, 0.50%; malignant, 1.02%, 1990-1995) than others. In this particular hospital, severe disease is manifested in a large proportion of patients and this likely have attributed to the findings. A recent study from a university hospital in Gwangju city and Chonnam province reported a similarly high incidence of malignant skin lesions as well (12). Based on the data from previous studies (5-12) and ours, the incidence of the premalignant and malignant skin lesions seem to be in a continuous rise since the early 1980s. As for the incidence of an individual lesion, AK showed a sharp increase compared to others (BD, BCC, SCC, and melanoma). There was a subtle increase in BCC and BD, whereas the incidence of SCC and melanoma were fairly constant. It was assumed that the early detection of skin cancer in the so called pre-SCC stage (AK, BD) and proper management of burn scars or skin tuberculosis suppressed the rise in the incidence of SCC.
The ratio between the premalignant and malignant skin lesions was 29.3%/70.7% in 1991-1998 and 37.5%/62.5% in 1999-2006. The increase in the proportion of cutaneous premalignancies was a consistent trend in all of 8 affiliated hospitals (data not shown). AK (71.2% of all premalignancies) and BD (24.6%) were the two most common premalignant skin lesions whereas for skin cancers, BCC (46.2% of all malignancies), SCC (19.1%), metastatic cancer and melanoma (7.1%) were common in a decreasing order. In our study, the change in the proportion of 2 major premalignant (AK, BD) and 3 major malignant skin lesion (BCC, SCC, melanoma) over their respective premalignant and malignant lesions was calculated over 2 different time periods (1991-1998, 1999-2006) for comparison. Among the premalignancies, only AK showed an increase in its proportion over time. The increase in the proportion of AK reflects increased UV exposure as well as a better understanding of skin cancer in general population. The increase in cancer surveillance and early detection is likely a result of increased public relations on skin cancer.
The proportion of BD was about one third of that of AK, and decreased over time. This may be explained by the fact that BD is not associated with solar radiation. In addition, arsenicals, which has been major cause of BD in the past, is now banned from Korean herbal medication.
The incidence of BCC increased with negligible decrease in its proportion among the malignant skin lesions in the later 8 yr (1999-2006) compared to the former half (1991-1998). BCC proved to be the most prevalent form of skin cancer. The ratio of BCC to SCC increased over time; 2.4 in 1991-1998 and 2.5 in 1999-2006. SCC used to be the most common of skin cancer in Korea, but the trend changed. BCC became the most prevalent type since the 1990s. BCC is now universally accepted as the most common form of skin cancer worldwide.
During this study period (1991-2006), for both premalignant and malignant skin lesions, females outnumbered males (66.9% vs. 33.1% and 52.5% vs. 47.5% respectively). In previous reports, males generally outnumbered females for cutaneous malignancies whereas there was slight predominance of females for cutaneous premalignancies (5, 8-11). The recent increased proportion of women with skin cancer is probably due to increased UV exposure and their longer life-span compared to men.
In AK, BD, and BCC, the peak age group was 61-80 yr. However, when the values between the two 8 yr-period were compared, a higher proportion of patients in the latter 8 yr were in the older age group. The peak age group of SCC was slightly higher, ranging from 71-90 yr. A relatively even age distribution was seen in melanoma. The longer life span and frequent hospital visits in the elderly have likely contributed to the increase in patients' age. It is nevertheless natural that the elderly have higher incidence of skin cancer with the accumulated exposure to UV and deteriorated innate protective means of the skin. The age distribution of premalignant and malignant skin lesions in this study was slightly higher compared to those performed in the 1980s (5-12).
In terms of anatomical location, 73.4% of the premalignant and 63.2% of all malignant skin lesions were found on the head and neck followed by the trunk and extremities. Within the head and neck, a majority of the premalignant lesions developed on the cheek, followed by the forehead, nose and periorbital area. The nose was the most common site of involvement within the head and neck area by a malignant skin lesion followed by the cheek, periorbital area and scalp. The location of AK, BD, BCC, SCC and melanoma was fairly similar to those previously reported.
The limitation of this study is that it is retrospective. Because we were not able to standardize our patients to the Korean standard population, our data did not represent the incidence or trend of premalignant and malignant skin lesions in Korea. A large scale study conducted prospectively in randomly selected multi-centers will be warranted.
In conclusion, data of this study showed an increased incidence of both premalignant and malignant skin lesions, with AK in particular. Skin cancer prevention by sunscreen and early detection should be emphasized.
Figures and Tables
References
1. Stang A, Stegmaier C, Jockel KH. Nonmelanoma skin cancer in the Federal State of Saarlang, Germany, 1995-1999. Br J Cancer. 2003. 89:1205–1208.
2. de Vries E, van de Poll-Franse LV, Louwman WJ, de Gruijl FR, Coebergh JW. Predictions of skin cancer incidence in the Netherlands up to 2015. Br J Dermatol. 2005. 152:481–488.
3. Diepgen TL, Mahler V. The epidemiology of skin cancer. Br J Dermatol. 2002. 146:Suppl 61. 1–6.
4. Ishihara K, Saida T, Otsuka F, Yamazaki N. Prognosis and Statistical Investigation Committee of the Japanese Skin Cancer Society. Statistical profiles of malignant melanoma and other skin cancers in Japan: 2007 update. Int J Clin Oncol. 2008. 13:33–41.
5. Chung HG, Moon TK, Bang DS, Lee MG. Clinical observation of cutaneous malignant tumors and premalignant lesions over 15 years (1982-1996). Korean J Dermatol. 1999. 37:1413–1422.
6. Shin JH, Cho S, Whang KK, Hahm JH. An epidemiologic analysis of cutaneous malignant tumors over 15 years (1984-1998). Korean J Dermatol. 1999. 37:1743–1751.
7. Seo JJ, Won YH, Kim SJ, Lee SC, Chun IK. A clinical observation of cutaneous malignant tumors over 10 years (1987-1996, Chonnam province). Korean J Dermatol. 1998. 36:812–819.
8. Moon SE, Cho KH, Hwang JH, Kim JA, Youn JI. A statistical study of cutaneous malignant tumors. Korean J Dermatol. 1998. 36:7–15.
9. Jeong KB, Kim HC, Shin DH, Choi JS, Kim KH. A clinical observation of cutaneous premalignant and malignant tumors. Korean J Dermatol. 2002. 40:924–931.
10. Seo PG, Moon SE, Cho KH. A statistical study of cutaneous malignant tumors (1996-2000). Korean J Dermatol. 2002. 40:129–137.
11. Kim DH, Kwon IH, Cho KH. A statistical study of cutaneous malignant tumors (2001-2005). Korean J Dermatol. 2008. 46:1581–1587.
12. Chun JS, Yun SJ, Lee JB, Kim SJ, Won YH, Lee SC. A statistical observation on 1430 cases of cutaneous malignant tumors over 20 years (1987-2006) in Gwangju city and Chonnam province. Korean J Dermatol. 2009. 47:667–673.




 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download