Abstract
There has been no report about hereditary and clinical features of retinitis pigmentosa (RP) in Koreans. To evaluate these, data were collected from 365 RP patients including age, gender, visual acuity (VA), spherical equivalent (SE) of refractive errors, funduscopic findings, color vision test, visual field score (VFS) obtained from Goldmann perimetry, and the inheritance patterns from pedigrees. Simplex RP was the most common inheritance pattern (61.9%); followed by autosomal recessive RP (17.3%), autosomal dominant RP (12.1%) and X-linked recessive RP (8.8%). Myopia was the most common refractive errors (77.5%) including 16.1% of high myopia. The most common cataract type was posterior subcapsular cataract (25.8%). Observed retinal findings included changes of retinal pigment epithelium (88.8%), bony spicule-like pigmentation (79.7%), attenuation of retinal vessel (76.2%), waxy disc pallor (12.6%), golden ring around optic disc (2.2%), epiretinal membrane (0.8%) and cystoid macular edema (0.5%). Corrected VA and refractive errors did not show any significant difference between the inheritance patterns. VFS was significantly worse in autosomal recessive RP than in autosomal dominant RP. Color vision defect was noted in 66.1% on Hardy-Rand-Rittlers color vision test. In conclusion, Korean RP patients have the indigenous hereditary and clinical features as well as the ordinary ones.
Retinitis pigmentosa (RP) is the term used for a group of hereditary retinal diseases that are characterized by progressive degeneration of rod and cone cells. The prevalence is about 1:4,000 worldwide ranging from 1:1,878 to 1:7,000 across different racial groups (1-6). Typical clinical features include night blindness, various peripheral and central visual loss, color vision defects or light flashes (7, 8). Since most patients are legally blind by age 40 yr, RP is one of the major causes of visual impairment in adults, ultimately affecting overall quality of life (9, 10).
RP is a genetically heterogeneous disorder transmitted in accordance with the Mendelian inheritance pattern in most cases. So far at least 44 causal genes and loci have been identified (11). Clinical and hereditary features may vary according to the genetic backgrounds (12). It has been reported that the autosomal dominant inheritance type has the least severe impairment while the X-linked recessive RP has the most severe impairment in visual acuity (13, 14).
In Asian populations, a few studies of RP from China, Japan and India have presented the prevalence, the clinical features and the inheritance patterns (15-18). In these studies, higher prevalence (1/930-1/1,000) (17, 18) of RP and less proportion of autosomal dominant RP (11-15.4%) (15, 16) were noticed compared to the western populations. In Korea, however, there have been a very few reports regarding only clinical features, which were investigated with a small number of RP patients (19-21).
The present study aims to investigate hereditary and clinical features of RP patients in Korea and to compare the clinical features according to the inheritance patterns.
The patients were recruited through advertisements from the outpatient clinic at Seoul National University Hospital and the Korean Retinitis Pigmentosa Society, a non-profit support network for Korean RP patients between August 2006 and March 2007. All patients volunteered to participate in the study associated with the Korean Genome Project. All patients provided informed consent before being enrolled in the study, in accordance with the protocol approved by the Institutional Review Board at Seoul National University Hospital (IRB No; H-0606-0055-175). It was explained to the patients that data of their ophthalmologic examinations and family history involving the pedigree, and genomic information would be exploited only for the investigation of RP. Blood sampling for DNA acquisition was carried out if a patient agreed. All protocols used in this study were also in full accordance with the tenets of the Declaration of Helsinki.
The diagnosis of RP was made when a patient showed bilateral retinal degeneration with typical pigmentations on funduscopic examination or rod dysfunction on standard electroretinogram (ERG) with degenerative retina.
Ophthalmological evaluation included best-corrected visual acuities (BCVA), refraction, measuring intraocular pressure (IOP), slit-lamp biomicroscopy, funduscopy, Goldmann perimetry, electroretinogram, color vision test using Hardy-Rand-Rittlers (HRR) pseudoisochromatic plates. Refractive errors were measured with autorefractometer and classified as myopia (spherical equivalent [SE] ≤-0.5 D), high myopia (SE ≤-6.0 D), emmetropia (-0.5 D<SE<0.5 D) and hyperopia (SE ≥0.5 D). Goldmann perimetry with V4e target was achieved on the all patients who were able to cooperate. BCVA were converted into the logarithm of the minimum angle of resolution (logMAR) visual acuities, refractive errors into spherical equivalents and visual fields from Goldmann perimetry into visual field score (VFS) based on American Medical Association guides for the analyses (22, 23).
Pedigrees were obtained from all patients through interviews. Inheritance patterns were determined based on the pedigrees as autosomal dominant (AD), autosomal recessive (AR), X-linked recessive (XL) or Simplex. AD inheritance was defined as RP showing direct vertical transmission in at least two generations with both males and females at equal risk and with no transmission to their offspring from unaffected persons. It was considered as AR inheritance when more than one member within the same sibship was affected and no other member of previous generation was affected. Males were involved almost exclusively in XL RP with no direct male-to-male transmission and involvement of half of the subsequent male offspring through their daughters from affected males. Simplex RP was diagnosed when there was no family history (24).
Mean age, refractive error, BCVA and VFS were compared between the inheritance patterns, using oneway ANOVA, Tukey's multiple comparison test and ANCOVA with age as a covariate. Linear regression analysis was applied for the relation between age and BCVA or VFS according to the inheritance patterns. Age, inheritance patterns and VFS were used as covariates in binomial logistic regression analysis to find the related factors of cataract development. SPSS 12.0 (SPSS Inc, Chicago, IL, USA) was employed to execute the statistical analyses. Statistical analyses were implemented with one of both eyes, i.e. the right eye, because of the strong correlation between both eyes. A P value of <0.05 was considered statistically significant.
A total of 365 patients with RP were included in this study. Mean age of the patients was 38.0±13.1 yr (range, 4 to 85 yr). Most common inheritance pattern was simplex RP (61.9%) followed by AR RP (17.3%), AD RP (12.1%) and XL RP (8.8%) (Table 1). Mean age of XL RP was significantly different from other inheritance patterns on P value of 0.05 (Tukey's multiple comparison test) (Table 1). Gender distribution was almost equal in AD RP (female 56.8%) and AR RP (female 49.2%); however, there were more males in simplex RP (female 33.6%) (P=0.004, Pearson's chi-square test). Five female patients (15.6%) were also diagnosed as XL RP from typical retinal change such as bony spicule and retinal pigment epithelial change.
Myopia was the most common refractive errors (193 of 249 eyes, 77.5%) including 16.1% (40 of 249 eyes) of high myopia whereas emmetropia was of 14.9% (37 of 249 eyes) and hyperopia of 7.6% (19 of 249 eyes). There was no significant difference in the refractive errors among the inheritance patterns (P=0.709, oneway ANOVA, Table 2). BCVA did not show any significant difference between the inheritance patterns (P=0.215; ANCOVA with age as a covariate, P=0.135; oneway ANOVA). However, BCVA (the logMAR vision) had a positive correlation with age (r2=0.025, P=0.013) (Fig. 1). A total of 113 of 365 patients (31.0%); 16 patients (36.4%) in AD RP, 21 patients (33.3%) in AR RP, 3 patients (9.4%) in XL RP and 73 patients (32.3%) in simplex RP were with BCVA 20/200 (1 logMAR) or less in a better eye.
VFS was significantly different between AD RP and AR RP on P value of 0.05 (Tukey's multiple comparison test, Table 2). The difference was also significant when age was considered as a covariate (P=0.008, ANCOVA). VFS decreased as the patients were aged in all inheritance patterns although the correlation strength was different between the groups (Fig. 2).
Among the fundus findings, change of retinal pigment epithelium was the most common (324 eyes, 88.8%) followed by bony spicule-like pigmentation (291 eyes, 79.7%), attenuation of retinal vessel (278 eyes, 76.2%), waxy disc pallor (46 eyes, 12.6%), golden ring around optic disc (8 eyes, 2.2%), epiretinal membrane (3 eyes, 0.8%) and cystoid macular edema (2 eyes, 0.5%) (Table 3).
Cataract was observed in 175 eyes (47.9%), of which 38 eyes (10.4%) had undergone cataract surgery (Table 3). Posterior subcapsular cataract (PSC) (94 eyes, 25.8%) was the most common type of cataract followed by nuclear sclerosis (54 eyes, 14.8%), cortical opacity (22 eyes, 5.9%), and anterior subcapsular cataract (14 eyes, 3.9%). According to the inheritance patterns, the presence of cataract or PSC was not significantly different when binomial logistic regression model was used with covariates of age, inheritance patterns and VFS.
Results of HRR color vision test were available in 124 eyes. Normal color vision was demonstrated in 42 eyes (33.9%) while achromatopsia was noted in 21 eyes (16.9%), blue-yellow color vision defect in 17 eyes (13.7%), red-green color vision defect in 36 eyes (29.0%) and both blue-yellow and red-green color vision defect in 8 eyes (6.5%), respectively.
This study revealed that the most common Mendelian inheritance pattern was simplex RP followed by AR RP, AD RP and XL RP in Korean RP patients. VFS was significantly worse in AR RP than in AD RP, while BCVA and refractive errors did not show any significant differences between the inheritance patterns.
Proportions of AD, AR, XL, and simplex RP from Asian countries were reported to be 11-16.9, 25.2-33.1, 0.5-7.7, and 48.3-56.3%, respectively (15, 16, 25). Compared to these reports, overall distribution of 365 RP patients was similar, although this study included more simplex RP and less AR RP.
Prevalence of myopia was reported to be higher in Asian populations compared to the western populations (26). However, only a few restricted data are available for the prevalence of myopia in adult Koreans. In one report, the prevalence of myopia in 19-yr-old Korean males was 56.4% with 12.9% of prevalence of high myopia (27). Even if considering this higher prevalence of myopia in Koreans, myopia was more common (77.5%) among RP patients in this study.
Significant difference of visual function between the inheritance patterns was demonstrated only in VFS between AD RP and AR RP when age was considered as a confounding factor. The association between the inheritance pattern and the degree of visual impairment is a controversial matter. Some reported worse visual function in AR RP as in this study, but others reported the opposite results (28, 29). The disparity in the reported vision impairment between the studies may be due to the various types and proportion of causal genes included in those studies. Less proportion of XR RP patients with VA less than 20/200 in our study might be due to relatively younger patients involved with that genetic type than those with other inheritance patterns (Table 4).
VFS had significant negative correlation with age in XL and simplex RP compared to AD and AR RP, although the correlation was weak. This might imply that AD and AR RP patients had more various clinical features in the disease onset and severity.
To reveal the factors associated with cataract and PSC formation, we used age, inheritance patterns and VFS as covariates in binomial logistic regression analysis because cataract develops more in aged population and might be affected by genetic types or disease severity; disease severity can be represented by a visual field. Only age was a statistically significant factor in the presence of cataract, whereas no aforementioned factor was significantly related with the PSC formation.
This study might be limited by the lacking values for ophthalmological examinations. Lacking data from the poor cooperation and the refusal from participants might overestimate the visual function of the patients. Moreover, voluntary enrollment of the patients from the clinic and the Korean RP society might underestimate the advanced RP patients. Population survey and the follow-up for the data of disease progression are needed.
To the author's knowledge, however, this is the first and largest report about hereditary and clinical features of RP in Koreans. The result of this study may be the basic information for RP patients in Korea. And the data about RP patients with significant visual impairment with BCVA 20/200 or less in a better eye (31.0%) from this study may offer basic information for the welfare policy for RP patients in Korea.
In conclusion, Korean RP patients have the indigenous hereditary and clinical features as well as the ordinary ones. The different features including high proportion of myopia require further investigations.
Figures and Tables
Fig. 1
Scattergram between best-corrected visual acuity (logMAR) of the right eye and age according to the inheritance patterns.
AD, autosomal dominant; AR, autosomal recessive; RP, retinitis pigmentosa; VA, visual acuity; XL, X-linked recessive.

Fig. 2
Scattergram between visual field score (VFS) of the right eye and age according to the inheritance patterns.
AD, autosomal dominant; AR, autosomal recessive; RP, retinitis pigmentosa; XL, X-linked recessive.

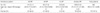
Table 2
Refractive error (spherical equivalent), best-corrected visual acuity (BCVA), and visual field score (VFS) in the right eye according to the inheritance patterns

*Values are presented as mean±standard deviation; †P=0.709, oneway ANOVA; ‡P=0.215 (ANCOVA with age as covariate), P=0.135 (oneway ANOVA); §P=0.008 (ANCOVA with age as covariate), P=0.022 (oneway ANOVA); ∥The same letters indicate non-significant difference of VFS between groups based on Tukey's multiple comparison test. Mean VFS of AD RP was significantly better than that of AR RP.
AD, autosomal dominant; AR, autosomal recessive; RP, retinitis pigmentosa; XL, X-linked recessive.
References
1. Grondahl J. Estimation of prognosis and prevalence of retinitis pigmentosa and Usher syndrome in Norway. Clin Genet. 1987. 31:255–264.
2. Haim M, Holm NV, Rosenberg T. Prevalence of retinitis pigmentosa and allied disorders in Denmark. I Main results. Acta Ophthalmol (Copenh). 1992. 70:178–186.
3. Bunker CH, Berson EL, Bromley WC, Hayes RP, Roderick TH. Prevalence of retinitis pigmentosa in Maine. Am J Ophthalmol. 1984. 97:357–365.
4. Heckenlively J, Friederich R, Farson C, Pabalis G. Retinitis pigmentosa in the Navajo. Metab Pediatr Ophthalmol. 1981. 5:201–206.
5. Bundey S, Crews SJ. A study of retinitis pigmentosa in the City of Birmingham. I Prevalence. J Med Genet. 1984. 21:417–420.
6. Hartong DT, Berson EL, Dryja TP. Retinitis pigmentosa. Lancet. 2006. 368:1795–1809.
7. Berson EL, Rosner B, Simonoff E. Risk factors for genetic typing and detection in retinitis pigmentosa. Am J Ophthalmol. 1980. 89:763–775.
8. Heckenlively JR, Yoser SL, Friedman LH, Oversier JJ. Clinical findings and common symptoms in retinitis pigmentosa. Am J Ophthalmol. 1988. 105:504–511.
9. Szlyk JP, Seiple W, Fishman GA, Alexander KR, Grover S, Mahler CL. Perceived and actual performance of daily tasks: relationship to visual function tests in individuals with retinitis pigmentosa. Ophthalmology. 2001. 108:65–75.
10. Hahm BJ, Shin YW, Shim EJ, Jeon HJ, Seo JM, Chung H, Yu HG. Depression and the vision-related quality of life in patients with retinitis pigmentosa. Br J Ophthalmol. 2008. 92:650–654.
11. Retinal Information Network. The University of Texas Health Science Center. accessed on 12 October 2009. Available at http://www.sph.uth.tmc.edu/retnet.
12. Kaplan J, Bonneau D, Frezal J, Munnich A, Dufier JL. Clinical and genetic heterogeneity in retinitis pigmentosa. Hum Genet. 1990. 85:635–642.
13. Fishman GA. Retinitis pigmentosa. Visual loss. Arch Ophthalmol. 1978. 96:1185–1188.
14. Grover S, Fishman GA, Alexander KR, Anderson RJ, Derlacki DJ. Visual acuity impairment in patients with retinitis pigmentosa. Ophthalmology. 1996. 103:1593–1600.
15. Hu DN. Genetic aspects of retinitis pigmentosa in China. Am J Med Genet. 1982. 12:51–56.
16. Hayakawa M, Matsumura M, Ohba N, Matsui M, Fujiki K, Kanai A, Tamai M, Shiono T, Tokoro T, Akazawa Y. A multicenter study of typical retinitis pigmentosa in Japan. Jpn J Ophthalmol. 1993. 37:156–164.
17. Xu L, Hu L, Ma K, Li J, Jonas JB. Prevalence of retinitis pigmentosa in urban and rural adult Chinese: The Beijing Eye Study. Eur J Ophthalmol. 2006. 16:865–866.
18. Sen P, Bhargava A, George R, Ve Ramesh S, Hemamalini A, Prema R, Kumaramanickavel G, Vijaya L. Prevalence of retinitis pigmentosa in South Indian population aged above 40 years. Ophthalmic Epidemiol. 2008. 15:279–281.
19. Shin WK, Ohn YH, Shin H, Lee HK. Three cases of atypical retinitis pigmentosa: diagnostic value of electroretinography. J Korean Ophthalmol Soc. 1994. 35:1295–1299.
20. Yoon IH, Kim SD. Fundus fluorescence angiographic classifications of the pericentral retinitis pigmentosa. J Korean Ophthalmol Soc. 1994. 35:1233–1240.
21. Kim KH, Park YH, Hahn DH. A case of unilateral retinitis pigmentosa. J Korean Ophthalmol Soc. 1996. 37:1090–1094.
22. Cocchiarella L, Anderson G. Guides to the evaluation of permanent impairment. 2001. 5th ed. Chicago: American Medical Association Press.
23. Colenbrander A. Guide for the evaluation of visual impairment. 1999. San Francisco: Pacific Vision Foundation.
24. Fishman GA. Retinitis pigmentosa. Genetic percentages. Arch Ophthalmol. 1978. 96:822–826.
25. Hayakawa M, Fujiki K, Kanai A, Matsumura M, Honda Y, Sakaue H, Tamai M, Sakuma T, Tokoro T, Yura T, Kubota N, Kawano S, Matsui M, Yuzawa M, Oguchi Y, Akeo K, Adachi E, Kimura T, Miyake Y, Horiguchi M, Wakabayashi K, Ishizaka N, Koizumi K, Uyama M, Ohba N. Multicenter genetic study of retinitis pigmentosa in Japan: I. Genetic heterogeneity in typical retinitis pigmentosa. Jpn J Ophthalmol. 1997. 41:1–6.
26. McCarty CA, Livingston PM, Taylor HR. Prevalence of myopia in adults: implications for refractive surgeons. J Refract Surg. 1997. 13:229–234.
27. Kang SH, Kim PS, Choi DG. Prevalence of myopia in 19-year-old Korean males: the relationship between the prevalence and education or urbanization. J Korean Ophthalmol Soc. 2004. 45:2082–2087.
28. Merin S, Auerbach E. Retinitis pigmentosa. Surv Ophthalmol. 1976. 20:303–346.
29. Pearlman JT. Mathematical models of retinitis pigmentosa: a study of the rate of progress in the different genetic forms. Trans Am Ophthalmol Soc. 1979. 77:643–656.
30. Fishman GA, Farber MD, Derlacki DJ. X-linked retinitis pigmentosa. Profile of clinical findings. Arch Ophthalmol. 1988. 106:369–375.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download