Abstract
We investigated the outcome of idarubicin plus N4-behenoyl-1-β-D-arabinofuranosyl cytosine (BHAC)-based chemotherapy (BHAC group, n=149) compared to idarubicin plus cytarabine-based chemotherapy (cytarabine group, n=191) for childhood acute myeloid leukemia (AML). Between January 1996 and December 2005, 340 children with AML from 5 university hospitals in Korea received the BHAC-based or cytarabine-based chemotherapy, with or without hematopoietic stem cell transplantation. After induction therapy, 264 (77.6%) of 340 children achieved a complete remission (CR) and 43 (12%) achieved a partial remission (PR). The CR rate in the BHAC group was higher than in the cytarabine group (85.2% vs. 71.7%, P=0.004). However, the overall response rate (CR+PR) was not different between the two groups (93.3% vs. 87.9%, P=0.139). The 5-yr estimates of overall survival (OS) of children in the two groups were similar (54.9% for the BHAC group vs. 52.4% for the cytarabine group, P=0.281). Although the results were analyzed according to the treatment type and cytogenetic risk, the OS showed no significant difference between the BHAC group and the cytarabine group. In the present study, the clinical outcomes of the BHAC-based chemotherapy, consisting of BHAC, idarubicin, and 6-TG, are comparable to that of the cytarabine-based chemotherapy for childhood AML.
The prognosis of children with acute myeloid leukemia (AML) has improved over the past 30 yr (1). Reported survival figures range from 40 to 60%, and the proportion of patients achieving complete remission (CR) range from 70 to 90% (2-6). This success reflects the use of increasingly intensive induction chemotherapy followed by post-remission chemotherapy or allogeneic hematopoietic stem cell transplantation (HSCT). However, debate continues regarding the best chemotherapeutic regimen in induction and post-remission therapy. The most widely used combination of chemotherapy for AML is anthracycline and cytarabine (ara-C), often in combination with etoposide or 6-thioguanine (6-TG) (2-6).
Cytarabine is a major antimetabolic drug used in the treatment of AML. However, the drug is rapidly inactivated by cytidine deaminase, and has a very short plasma half-life (7). Many studies have been done on the administration schedule and dose of cytarabine in order to achieve optimum therapeutic effect with minimal adverse events. Other trials for overcoming the limitation of cytarabines include the development of cytarabine derivatives resistant to deamination (7). N4-behenoyl-1-β-D-arabinofuranosylcytosine (BHAC) is lipophilic, resistant to cytidine deaminase, and has strong antitumor activity against a wide variety of tumors regardless of administration schedules (8-10).
In clinical studies, BHAC combined with anthracycline showed a 60-80% CR rate, which was comparable to cytarabine-based chemotherapy for adult AML (11-14). Idarubicin (IDA)-BHAC combination regimen, which consists of IDA plus BHAC and 6-TG, has been widely used for induction or post-remission therapy for childhood AML in Korea. However, few reports have been made on IDA-BHAC chemotherapy for childhood AML (13, 15). In this retrospective, multicenter study, we report the results of IDA plus BHAC-based chemotherapy for childhood AML between 1996 and 2005. It is well established that multi-drug combination chemotherapy including cytarabine combined with anthracycline has shown a high CR rate and has been widely used in consolidation therapy as well as induction therapy for childhood AML (2-6). Therefore, we investigated the outcomes of BHAC-based chemotherapy compared to the cytarabine-based chemotherapy for childhood AML.
Between January 1996 and December 2005, 464 children from 5 university hospitals in Korea were diagnosed with AML. Patients included were younger than 20 yr at the time of diagnosis and had no prior treatment. Patients with Down syndrome, secondary AML, extramedullary leukemia without bone marrow involvement, or acute promyelocytic leukemia were excluded. Patients who underwent HLA-mismatched HSCT or cord blood transplantation after remission were also excluded. If the number of patients treated with each chemotherapy protocol was below 30, the data from the corresponding institution were not included. A total of 340 children were included in this study.
Initial diagnosis of AML was done at each hospital. Leukemia subtypes were recorded using the French-American-British (FAB) classification system (16). Bone marrow was analyzed for cytogenetic abnormalities and immunophenotype at diagnosis.
The IDA plus BHAC-based induction regimen consisted of BHAC daily 200-250 mg/m2 intravenously (IV) for 7 consecutive days, IDA daily 12 mg/m2 IV 3 consecutive days (day 1 to 3), and 6-TG daily 100 mg/m2 orally for 7 days. The IDA plus cytarabine-based induction regimen consisted of cytarabine daily 100 mg/m2 continuously IV for 7 days or 100 mg/m2/12-hr b.i.d IV infusion for 7 days and IDA daily 12 mg/m2 IV 3 consecutive days (day 1 to 3). According to the each institutional principle, etoposide daily 150 mg/m2 IV for 3 days (day 4 to 6) and 6-TG daily 160 mg/m2 orally for 7 days were added in the IDA plus cytarabine-based induction chemotherapy.
Patients who had achieved a CR received consolidation therapy. Allogeneic HSCT was recommended to all patients in first remission with HLA-matched familial or unrelated donors. HLA typing for class I and class II antigens was performed using standard serologic techniques. Familial donor-patient pairs were considered fully matched by compatibility for HLA-A, -B, -C, and -DRB1. Unrelated donor-patient pairs were considered matched for HLA-A, -B, and -DRB1. The patients without an available donor received autologous HSCT or further intensive chemotherapy in accordance with the institutional principle. Patients who had not achieved remission received another course of chemotherapy. For convenience, treatment was subdivided into two groups as follows: the patients who underwent HSCT after induction therapy (Transplantation group) and the patients who did not receive HSCT (Chemotherapy group), including patients who died during induction chemotherapy or patients lacking an available donor.
In post-remission chemotherapy, each institution adopted a different chemotherapy protocol. Therefore, patients were classified into the "BHAC group" or the "cytarabine group" in accordance with the regimen administered for remission induction.
CR was defined as less than 5% leukemic blasts in the bone marrow with evidence of normal hematopoiesis, no leukemia cells in peripheral blood or anywhere else. Induction death was defined as a fatal event occurring within the first 6 weeks of treatment. Induction death occurring before starting treatment was not included in this study. Partial remission (PR) was defined as a bone marrow with 5-15% blast cells and evidence of regeneration of normal hematopoietic cells. Patients who did not achieve CR or PR and who survived after the first 6 weeks of treatment were defined as nonresponders (NR).
Cytogenetic abnormalities were classified into 3 risk groups: low risk, t(8;21), inv(16); high risk, 11q23 rearrangement, -5, del(5q), -7, del(7q), inv(3)/t(3;3)/ins(3;3); intermediate risk, normal karyotype or other numerical or structural abnormalities.
Event-free survival (EFS) was calculated from the date of diagnosis to last follow-up or first event (failure to achieve remission, demonstration of resistant leukemia, relapse, second malignancy or death due to any cause, whichever occurred first). Patients who did not attain CR were considered failures at time zero. Overall survival (OS) was defined as the time between diagnosis and death from any cause or time of last contact.
The characteristics of two chemotherapy groups were compared using chi-square test or Fischer's exact test for categorical data and Mann-Whitney U test for continuous variables. Probabilities of survival were estimated using the Kaplan-Meier method and were compared using the log-rank test. Data for all surviving patients were censored as of April 2007.
Patient characteristics of the two groups are given in Table 1. A total of 340 patients were included in the BHAC group and the cytarabine group. There was no significant difference in the patient characteristics between the two groups. The median age at presentation was 7.7 yr, 7% were infants less than 1 yr of age, 34% were 10-yr old or more at diagnosis. The median white blood cell count (WBC) at diagnosis was 15.8×109/L, and 25% of the children showed a WBC count of at least 50×109/L. Karyotypes were available for 92% of patients. The cytogenetics of patients in the two groups are presented in Table 2. A significant difference was noted with regards to the frequency of cytogenetic aberrations (P=0.03), with patients with the 11q23 rearrangement more frequently observed in the BHAC group than in the cytarabine group. In the cytarabine group, the different induction regimens were administered equally. HSCT was performed in 211 patients (62%) treated in both groups.
After induction chemotherapy, 264 (77.6%) of 340 children achieved a CR. The results of the BHAC group and the cytarabine group are compared in Table 3. The CR rate in the BHAC group was higher than in the cytarabine group (85.2% vs. 71.7%, P=0.004). However, the overall response (CR+PR) rates between the 2 groups were not significantly different (93.3% vs. 87.9%, P=0.139). The percentage of induction death and nonresponders showed no significant difference between the two groups. Five (33%) of 15 nonresponders after the first induction therapy in the two groups were alive at time of last follow-up. In the cytarabine group, the overall response rates of the three types of induction regimen (IDA+cytarabine, IDA+cytarabine+etoposide, and IDA+cytarabine+etoposide+6-TG) were 78.5%, 93.8%, and 91.9%, respectively (P=0.022).
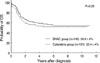
A total of 200 patients survived with a median follow-up of 4.1 yr. The 5-yr estimate of OS of 340 children was 53.3%. The 5-yr estimates of OS of children were not significantly different between the BHAC group and the cytarabine group (54.9% vs. 52.4%, P=0.281) (Fig. 1). Although the children were divided into the two groups (chemotherapy group and transplantation group), the OS and EFS showed no significant difference between the BHAC group and the cytarabine group (Fig. 2, 3). When the patients who died during induction chemotherapy were excluded in the chemotherapy group, a total of 111 patients received the further intensive chemotherapy. The 5-yr estimates of OS of the 111 children in the BHAC group and cytarabine group were 44.6% and 38.6%, respectively (P=0.591) and the EFS were 29.8% and 28.6%, respectively (P=0.679). For patients who received HSCT, the OS and EFS of children in the two groups were similar with regard to the type of HSCT (Table 4). The OS of patients in the two groups was also not significantly different in terms of the cytogenetic risk (Table 5).
The 5-yr estimates of OS and EFS of patients achieving a first CR were higher in the transplantation group (64.4% and 58.0%, respectively) than in the chemotherapy group (41.0% and 28.6%, respectively) (P<0.001).
In the present study, the clinical outcome of the BHAC-based regimen, consisting of BHAC, idarubicin, and 6-TG, are comparable to that of the cytarabine-based regimen for childhood AML. In a phase II study, BHAC monotherapy for adult AML produced a 36% CR rate and adverse events such as nausea and vomiting were less than for cytarabine (17). In a comparative study between BHAC and cytarabine in combination induction and consolidation therapy for adults with de novo AML, the efficacy of BHAC given with daunorubicin was found to be inferior to that of cytarabine in combination with daunorubicin (14). However, the dose of BHAC was not equivalent to that of cytarabine in terms of the mean leukocyte nadir of both groups (18). In Korea, the combination regimen consisting of IDA and BHAC has been widely used for induction or post-remission therapy for adult and childhood AML since 1996. Park et al. (13) reported that IDA-BHAC combination regimen for previously untreated adult and childhood AML showed a high CR rate (75%), which was similar or superior to results obtained with cytarabine and other anthracyclines. However, a small number of children (22%) were included in their study and follow-up duration was too short to draw a complete conclusion.
The anti-leukemic efficacy of IDA-BHAC regimen in remission induction appears to be effective, with a high CR rate (85.2%) compared to the CR rate (71.7%) of cytarabine-based regimen in our study. The proportion of NR is comparable between the 2 groups after remission induction chemotherapy (4% in the BHAC group; 4.7% in the cytarabine group). In the present study, children in the two groups have a similar 5-yr estimate of OS (55% in the BHAC group; 53% in the cytarabine group). These results are comparable to previously summarized results of the AML-BFM93, UK-MRC AML10, CCG-2891, and NOPHO-AML93, which enrolled patients between 1988 and 2001 (2-4, 6). Children with de novo AML in these studies showed CR rates of 78-93%, induction death rates of 2-7%, proportion of NR of 3-18%, and 5-yr estimates of OS of 47-66%. The addition of other agents to the standard "7+3" induction regimen did not improve the remission rate, OS or EFS in children and adolescents with AML in UK-MRC AML10 trial and CCG-213 study (2, 3). In our results, the addition of etoposide improves the remission rate. However, children who received the three types of induction regimen have shown similar long-term outcome in terms of OS and EFS.
Since the cytotoxic effect of cytarabine is time-dependent and S-phase specific, the standard dose of cytarabine is thought to have better therapeutic effects when administered by continuous IV infusions rather than by short-time IV infusion (7). Because BHAC, a new cytarabine analogue, has a long plasma half-life after IV administration and releases cytarabine slowly, it may give the same effect as continuous cytarabine infusion (19). Studies of Nara et al. (10) have demonstrated that BHAC is rapidly taken into leukemic blasts and converted to cytarabine, and has a suppressive activity on self-renewal of leukemic blast progenitors in vitro. Therefore, BHAC may contribute to these results which are comparable to those of cytarabine-based chemotherapy.
In our study, the 5-yr estimates of EFS and OS for children appear to be much lower in the chemotherapy group than in the transplantation group. In this retrospective survey, the chemotherapy group includes induction deaths and has more nonresponders than the transplantation group. Although autologous and allogeneic HSCT represent approaches to dose intensification, several randomized studies in pediatrics have shown no advantage of autologous HSCT compared to chemotherapy alone and the majority of clinical trials have demonstrated a consistent advantage for allogeneic HSCT in terms of disease-free survival, but not always for OS (3, 6, 20-22). In our study period, allogeneic HSCT was recommended to all patients in first remission with HLA-matched familial or unrelated donors and autologous HSCT was performed for patients without an available donor. The patients who were not candidates for HSCT received intensive chemotherapy according to the institutional principle. Therefore, our study is not a prospective randomized trial comparing chemotherapy with HSCT and our results may have a selection bias in survival analysis. For this reason, our results do not suggest the superiority of transplantation over intensive chemotherapy but the comparable outcomes of IDA plus BHAC and 6-TG versus idarubicin plus cytarabine-based regimen in childhood de novo AML regardless of post-induction therapy.
The cytogenetic aberrations in our study show a high proportion of children with t(8;21) compared to other studies (2-6). In our pediatric population, the children with favorable karyotypes such as t(8;21) or inv(16) appear to show a better outcome than those with an unfavorable kayrotype in both the BHAC and cytarabine group. However, recent reports suggest that t(8;21) and inv(16) AMLs seem to be distinct clinical entities and should be stratified and reported separately when considering race, secondary cytogenetic abnormalities (23, 24). Karyotype markers with unfavorable implications also have been identified, such as -5/del(5q) and -7/del(7q) (3). In our data, the patients with -7/del(7q) show a very poor prognosis compared to the reported figure (21). Only two patients had -5/del(5q), a rare cytogenetic abnormality in children, so it appears difficult to draw any conclusion. This issue needs to be elucidated further in the future, as well as the other prognostic implications such as FLT3 internal tandem duplications (FLT3-ITDs) (25).
This study is limited by its retrospective nature. Patients are not equally randomized into the BHAC group and cytarabine group in induction or post-remission therapy at each institution. There is a little heterogeneity in the induction regimen and post-remission therapy in terms of administration schedule of cytarabine, addition of etoposide, and different consolidation schedule. However, the main point of our investigation is that BHAC shows a similar efficacy compared to cytarabine in combination chemotherapy in view of induction response and long term survival. Another limitation is that the information for adverse events during induction therapy is not enough to compare the two groups in terms of regimen-related toxicity. Since childhood AML is a rare disease, further studies with a prospective, randomized, multiinstitutional cohort are required to validate the results of our study and additional studies about risk-directed therapy including post-remission intensive chemotherapy and HSCT are warranted.
Figures and Tables
Table 1
Patient characteristics

*Comparison between the BHAC group and Cytarabine group.
M, male; F, female; FAB, French-American-British; WBC, white blood cell count; IDA, idarubicin; BHAC, N4-behenoyl-1-β-D-arabinofuranosyl cytosine; TG, 6-thioguanine; VP, etoposide; HSCT, hematopoietic stem cell transplantation; NS, not significant.
ACKNOWLEDGMENT
The authors are grateful to all members of the Korean Society of Pediatric Hematology-Oncology for data collection.
References
1. Kaspers GJ, Creutzig U. Pediatric acute myeloid leukemia: international progress and future directions. Leukemia. 2005. 19:2025–2029.
2. Smith FO, Alonzo TA, Gerbing RB, Woods WG. Arceci RJ for the Children's Cancer Group. Long-term results of children with acute myeloid leukemia: a report of three consecutive Phase III trials by the Children's Cancer Group: CCG 251, CCG 213 and CCG 2891. Leukemia. 2005. 19:2054–2062.
3. Gibson BE, Wheatley K, Hann IM, Stevens RF, Webb D, Hills RK, De Graaf SS, Harrison CJ. Treatment strategy and long-term results in paediatric patients treated in consecutive UK AML trials. Leukemia. 2005. 19:2130–2138.
4. Lie SO, Abrahamsson J, Clausen N, Forestier E, Hasle H, Hovi L, Jonmundsson G, Mellander L, Siimes MA, Yssing M, Zeller B, Gustafsson G. Nordic Society of Pediatric Hematology and Oncology (NOPHO). AML Study Group. Long-term results in children with AML: NOPHO-AML Study Group--report of three consecutive trials. Leukemia. 2005. 19:2090–2100.
5. Ravindranath Y, Chang M, Steuber CP, Becton D, Dahl G, Civin C, Camitta B, Carroll A, Raimondi SC, Weinstein HJ. Pediatric Oncology Group. Pediatric Oncology Group (POG) studies of acute myeloid leukemia (AML): a review of four consecutive childhood AML trials conducted between 1981 and 2000. Leukemia. 2005. 19:2101–2116.
6. Creutzig U, Zimmermann M, Ritter J, Reinhardt D, Hermann J, Henze G, Jürgens H, Kabisch H, Reiter A, Riehm H, Gadner H, Schellong G. Treatment strategies and long-term results in paediatric patients treated in four consecutive AML-BFM trials. Leukemia. 2005. 19:2030–2042.
7. Hamada A, Kawaguchi T, Nakano M. Clinical pharmacokinetics of cytarabine formulations. Clin Pharmacokinet. 2002. 41:705–718.
8. Aoshima M, Tsukagoshi S, Sakurai Y, Oh-ishi JI, Ishida T, Kobayashi H. N4-Behenoyl-1-beta-D-arabinofuranosylcytosine as a potential new antitumor agent. Cancer Res. 1977. 37:2481–2486.
9. Aoshima M, Tsukagoshi S, Sakurai Y, Oh-ishi J, Ishida T, Kobayashi H. Antitumor activities of newly synthesized N4-acyl-1-beta-D-arabinofuranosylcytosine. Cancer Res. 1976. 36:2726–2732.
10. Nara N, Tohda S, Suzuki T, Nagata K, Yamashita Y, Imai Y, Maruyama Y, Tomiyama J. Effects of N4-behenoyl-1-beta-D-arabinofuranosylcytosine on blast progenitors of acute myeloblastic leukemia. Cancer Res. 1990. 50:7587–7592.
11. Ohno R, Kato Y, Nagura E, Murase T, Okumura M, Yamada H, Ogura M, Minami S, Suzuki H, Morishima Y, Yokomaku S, Ezaki K, Kodera Y, Kawashima K, Saito H, Yamada K. Behenoyl cytosine arabinoside, daunorubicin, 6-mercaptopurine, and prednisolone combination therapy for acute myelogenous leukemia in adults and prognostic factors related to remission duration and survival length. J Clin Oncol. 1986. 4:1740–1747.
12. Nagura E, Kimura K, Yamada K, Ohta K, Maekawa T, Takaku F, Uchino H, Masaoka T, Amaki I, Kawashima K, Kariyone S, Toyama K, Ichimaru M, Nomura T, Sakai Y, Takatsuki K, Hamajima N. Nationwide randomized comparative study of daunorubicin and aclarubicin in combination with behenoyl cytosine arabinoside, 6-mercaptopurine, and prednisolone for previously untreated acute myeloid leukemia. Cancer Chemother Pharmacol. 1994. 34:23–29.
13. Park HS, Kim DW, Kim CC, Kim HK, Kim JS, Hwang TJ, Kim HJ, Kim HS, Song HS, Park JW, Ahn HS, Chung TJ, Cho KS, Lee KS, Choi YM. Induction chemotherapy with idarubicin plus N4-behenoyl-1-beta-D-arabinofuranosylcytosine in acute myelogenous leukemia: a newly designed induction regimen--a prospective, cooperative multicenter study. Semin Hematol. 1996. 33:4 Suppl 3. 24–29.
14. Kobayashi T, Miyawaki S, Tanimoto M, Kuriyama K, Murakami H, Yoshida M, Minami S, Minato K, Tsubaki K, Ohmoto E, Oh H, Jinnai I, Sakamaki H, Hiraoka A, Kanamaru A, Takahashi I, Saito K, Naoe T, Yamada O, Asou N, Kageyama S, Emi N, Matsuoka A, Tomonaga M, Ohno R. The Japan Leukemia Study Group. Randomized trials between behenoyl cytarabine and cytarabine in combination induction and consolidation therapy, and with or without ubenimex after maintenance/intensification therapy in adult acute myeloid leukemia. J Clin Oncol. 1996. 14:204–213.
15. Takashima Y. Clinical use of intermediate to high dose of N4-behenoyl-1-beta-D-arabinofuranosylcytosine in children with acute leukemia. J Clin Pharmacol. 1988. 28:356–362.
16. Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, Sultan C. Proposals for the classification of the acute leukaemias. French-American-British (FAB) co-operative group. Br J Haematol. 1976. 33:451–458.
17. Kimura K, Ohno R, Amaki I, Hattori K, Hirota Y, Hoshino A, Ichimaru M, Ito M, Kimura I, Maekawa T, Masaoka T, Nakamura T, Ogawa M, Oguro M, Ohta K, Osamura S, Shimoyama M, Takaku F, Uzuka Y, Yamada K. Treatment of acute myelogenous leukemia in adults with N4-behenoyl-1-beta-D-arabinofuranosylcytosine. Cancer. 1985. 56:1913–1917.
18. Miyawaki S, Kobayashi T, Tanimoto M, Kuriyama K, Murakami H, Yoshida M, Minami S, Minato K, Tsubaki K, Omoto E, Oh H, Jinnai I, Sakamaki H, Hiraoka A, Kanamaru A, Takahashi I, Saito K, Naoe T, Yamada O, Asou N, Kageyama S, Emi N, Ueda T, Tomonaga M, Ohno R. The Japan Adult Leukemia Study Group. Comparison of leukopenia between cytarabine and behenoyl cytarabine in JALSG AML-89 consolidation therapy. Int J Hematol. 1999. 70:56–57.
19. Ueda T, Nakamura T, Ando S, Kagawa D, Sasada M, Uchino H, Johno I, Akiyama Y. Pharmacokinetics of N4-behenoyl-1-beta-D-arabinofuranosylcytosine in patients with acute leukemia. Cancer Res. 1983. 43:3412–3416.
20. Ravindranath Y, Yeager AM, Chang MN, Steuber CP, Krischer J, Graham-Pole J, Carroll A, Inoue S, Camitta B, Weinstein HJ. Pediatric Oncology Group. Autologous bone marrow transplantation versus intensive consolidation chemotherapy for acute myeloid leukemia in childhood. N Engl J Med. 1996. 334:1428–1434.
21. Alonzo TA, Wells RJ, Woods WG, Lange B, Gerbing RB, Buxton AB, Neudorf S, Sanders J, Smith FO, Feig SA. Postremission therapy for children with acute myeloid leukemia: the children's cancer group experience in the transplant era. Leukemia. 2005. 19:965–970.
22. Oliansky DM, Rizzo JD, Aplan PD, Arceci RJ, Leone L, Ravindranath Y, Sanders JE, Smith FO 3rd, Wilmot F, McCarthy PL Jr, Hahn T. The role of cytotoxic therapy with hematopoietic stem cell transplantation in the therapy of acute myeloid leukemia in children: an evidencebased review. Biol Blood Marrow Transplant. 2007. 13:1–25.
23. Marcucci G, Mrózek K, Ruppert AS, Maharry K, Kolitz JE, Moore JO, Mayer RJ, Pettenati MJ, Powell BL, Edwards CG, Sterling LJ, Vardiman JW, Schiffer CA, Carroll AJ, Larson RA, Bloomfield CD. Prognostic factors and outcome of core binding factor acute myeloid leukemia patients with t(8;21) differ from those of patients with inv(16): a Cancer and Leukemia Group B study. J Clin Oncol. 2005. 23:5705–5717.
24. Narimatsu H, Yokozawa T, Iida H, Tsuzuki M, Hayakawa M, Takeo T, Iino M, Ichihashi T, Kato C, Sawamoto A, Sao H, Yanada M, Emi N, Kiyoi H, Yamaguchi T, Naoe T, Suzuki R, Sugiura I. Clinical characteristics and outcomes in patients with t(8;21) acute myeloid leukemia in Japan. Leukemia. 2008. 22:428–432.
25. Meshinchi S, Alonzo TA, Stirewalt DL, Zwaan M, Zimmerman M, Reinhardt D, Kaspers GJ, Heerema NA, Gerbing R, Lange BJ, Radich JP. Clinical implications of FLT3 mutations in pediatric AML. Blood. 2006. 108:3654–3661.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download