Abstract
Papillary fibroelastoma is a rare benign cardiac tumor that represents 10% of all primary cardiac tumors. Diagnosis is accomplished incidentally by echocardiography that is usually performed for another purpose. Most papillary fibroelastomas are asymptomatic, but the lesions are recognized as a cause of embolisms. To the best of our knowledge, there has been no case report of computed tomography findings of a papillary fibroelastoma. We report a case of a papillary fibroelastoma in a 78-yr-old woman who had dyspnea and chest tightness. Echocardiography revealed a small lobulated mobile echogenic mass attached to the aortic valve, and CT demonstrated a lobulated soft tissue density mass with a thin stalk at the sinotubular junction of the aortic valve.
Although rare, papillary fibroelastomas are the second most common primary benign cardiac tumors after myxomas and represent 10% of all primary cardiac tumors (1, 2). Over 90% of papillary fibroelastomas occur in the cardiac valves, making the lesions the most common tumors of the valves (3). Most papillary fibroelastomas are incidentally found after an autopsy, echocardiography or coronary surgery, as the tumors are typically asymptomatic.
If symptoms are present, the symptoms are usually related to embolic events (4, 5). As most papillary fibroelastomas are discovered with the use of echocardiography, there have been few studies that have described the tumors with magnetic resonance (MR) findings, and there have been no reports describing computed tomography (CT) findings. Some reports have described the MR findings of a papillary fibroelastoma as a hypointense mobile mass on T2-weighted image (6, 7). Although echocardiography is the primary modality for imaging intracardiac disease, with the advent of multidetector-row CT (MDCT), CT and MR imaging have played an increasingly important role as the soft tissue contrast obtained with both modalities is superior to that of echocardiography and both CT and MR imaging allow evaluation of the extracardiac extent of disease (8). In addition, MDCT can also help to evaluate the coronary arteries and extracardiac abnormalities. In contrast to the use of these noninvasive techniques, the use of cardiac catheterization can be associated with an added risk to patients as a catheter may dislodge a fragment of a tumor or adherent thrombi (9). Thus, the use of cardiac catheterization is not usually recommended. Here, we report MDCT findings of a papillary fibroelastoma in an aortic valve.
A 78-yr-old woman visited our institution to evaluate dyspnea on exertion, palpitation and chest tightness. The patient had a history of a transient ischemic attack one year prior.
During an initial evaluation, the patient underwent echocardiography (Vivid 7 Dimension; GE Healthcare, Chalfont St. Giles, UK). On transthoracic echocardiography, a small echogenic mass was noted located at the noncoronary cusp of the aortic valve. On transesophageal echocardiography, a 15×10 mm sized mobile lobulated echogenic mass was detected (Fig. 1). The mass was seen as attached to the sinotubular junction between the right and left coronary cusps. The cardiac chamber size and left ventricular systolic function were normal. The valvular functions were normal except for trivial mitral regurgitation. The patient had no clinical evidence of endocarditis such as fever, leukocytosis and murmur, and the patient had no underlying valvular disease and no prosthetic valve was present. For further evaluation, coronary CT angiography was performed with a Sensation 64-MDCT scanner (Siemens Medical Solutions, Erlangen Germany). The amount of total injected contrast media was 60 mL (4 mL/sec). CT showed an 11 mm lobulated soft tissue density mass at the sinotubular junction between the right coronary cusp and noncoronary cusp of the aortic valve and the lesion had a thin stalk as seen on a volume-rendered image (Fig. 2). In the mid level of the left anterior descending coronary artery, focal calcified plaque was seen without significant stenosis. No abnormal findings were detected in the other coronary arteries and cardiac chambers.
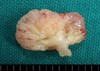
The patient had open surgery, and a small mass was found attached to the commissure between the right and the left coronary cusps. The size of the mass was 11 mm in the longest dimension and the lesion had multiple threads on the surface and some gelatinous materials in part of the mass (Fig. 3). Grossly, the aortic valve showed no abnormality.
On a microscopic examination, densely hyalinized central connective tissue core surrounded by a flat endocardial lining was seen, suggestive of a papillary fibroelastoma (Fig. 4).
A papillary fibroelastoma is a collection of avascular fronds of dense connective tissue lined by endothelium (2). As the lesions are usually asymptomatic, papillary fibroelastomas are likely underrepresented and the reported prevalence of papillary fibroelastoma varies. In a surgical series at the Mayo Clinic (1) and the Armed Forces Institute of Pathology (2), papillary fibroelastomas represented 10% of all primary cardiac tumors and were the second most common primary benign cardiac tumors after myxomas. Over 90% of papillary fibroelastomas occur on the valvular surface, and the lesions are the most common tumors in the cardiac valves (3). There is a slight predilection for left-sided valves (aortic and mitral valves) than right-sided valves (tricuspid and pulmonary valves) (10), but this predilection may be due to increased prevalence of symptoms associated with left-sided fibroelastomas. Grossly, papillary fibroelastomas are seen as gelatinous masses with a characteristic "sea anemone" appearance due to the presence of multiple delicate papillary fronds. The tumors are small, usually less than 15 mm in diameter, and are attached to the endocardium by a short thin stalk (5). Histologically, the fronds of a papillary fibroelastoma consist of myxoid connective tissue containing abundant mucopolysaccharide matrix and elastic fibers, covered by endothelial cells (11).
Most papillary fibroelastomas are discovered with echocardiography. The tumors appear as small, mobile, homogenous valvular or endocardial masses attached to valves or the endocardium by a short pedicle (4, 8). The tumors may be seen with a speckled appearance with a stippled pattern near the edges, which correlates with the papillary projection on the tumor surface (12). As the lesions are small and attached to moving valves, they are usually not seen on CT or MR images (8). There have been few descriptions of the appearance of a fibroelastoma on MR images. An MR image demonstrates a mobile mass on a valve leaflet or on the endocardial surface of the affected cardiac chamber as seen on cine gradient echo images (4, 6, 7, 13).
The differential diagnosis of a cardiac papillary fibroelastoma includes other cardiac tumors, thrombi and vegetations. A cardiac myxoma is a predominant atrial tumor, especially in the left atrium. The tumors are rarely found on valves. Thrombi can be differentiated by an irregular shape and absence of a pedicle. Bacterial vegetation has a valvular location and mobility, which makes it difficult to differentiate from a papillary fibroelastoma. However, bacterial vegetation has a more irregular appearance and is usually associated with clinical signs of endocarditis and valvular destruction (9).
In our case, although the mass was small and mobile, CT images showed a lobulated contour and a thin stalk, which made it possible to diagnose a pedunculated tumor rather than a thrombus. As seen on CT images, the tumor was located between the right coronary cusp and noncoronary cusp. However, the echocardiographic findings and surgery revealed that the tumor was located between the right coronary cusp and left coronary cusp. This finding indicates mobility of the tumor by the stalk.
With the use of current technology, MDCT can sometimes be used to detect a papillary fibroelastoma even though the tumor is small and mobile, especially when the lesion is seen with a stalk that enables the differentiation of the tumor from a thrombus.
Figures and Tables
Fig. 1
Transesophageal echocardiography shows a 15×10 mm sized lobulated echogenic mass attached to the sinotubular junction of the aortic valve.
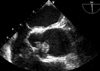
Fig. 2
Axial (A) and coronal (B) CT images show an 11 mm lobulated soft tissue density mass (arrow) at the sinotubular junction between the right coronary cusp (R) and noncoronary cusp (N) of the aortic valve. A volume-rendered image (C) shows a thin stalk (arrow) that is connected between the lesion and the aortic valve. A virtual aortoscopic image (D) shows a lobulated mass (arrow).

References
1. Tazelaar HD, Locke TJ, McGregor CG. Pathology of surgically excised primary cardiac tumors. Mayo Clin Proc. 1992. 67:957–965.

2. Burke A, Virmani R. Tumors of the heart and great vessels. Atlas of tumor pathology: fasc 16, ser 3. 1996. Washington, DC: Armed Forces Institute of Pathology;1–98.
3. Edwards FH, Hale D, Cohen A, Thompson L, Pezzella AT, Virmani R. Primary cardiac valve tumors. Ann Thorac Surg. 1991. 52:1127–1131.

4. Grebenc ML, Rosado de Christenson ML, Burke AP, Green CE, Galvin JR. Primary cardiac and pericardial neoplasms: radiologicpathologic correlation. Radiographics. 2000. 20:1073–1103.

5. Sparrow PJ, Kurian JB, Jones TR, Sivananthan MU. MR imaging of cardiac tumors. Radiographics. 2005. 25:1255–1276.

6. Wintersperger BJ, Becker CR, Gulbins H, Knez A, Bruening R, Heuck A, Reiser MF. Tumors of the cardiac valves; imaging findings in magnetic resonance imaging, electron beam computed tomography and echocardiography. Eur Radiol. 2000. 10:443–449.

7. Shiraishi J, Tagawa M, Yamada T, Sawada T, Tatsumi T, Azuma A, Shimada Y, Yaku H, Kitamura N, Nakagawa M. Papillary fibroelastoma of the aortic valve: evaluation with transoesophageal echocardiography and magnetic resonance imaging. Jpn Heart J. 2003. 44:799–803.
8. Araoz PA, Mulvagh SL, Tazelaar HD, Julsrud PR, Breen JF. CT and MR imaging of benign primary cardiac neoplasms with echocardiographic correlation. Radiographics. 2000. 20:1303–1319.

9. Ramesh MG, Ijaz AK, Chandra KN, Nirav JM, Balendu CV, Terrence JS. Cardiac papillary fibroelastoma: A comprehensive analysis of 725 cases. Am Heart J. 2003. 146:404–410.
10. Grinda JM, Couteil JP, Chauvaud S, D'Attellis N, Berrebi A, Fabiani JN, Deloche A, Carpentier A. Cardiac valve papillary fibroelastoma: surgical excision for revealed or potential embolization. J Thorac Cardiovasc Surg. 1999. 117:106–110.

11. Frederick JS. Ramzi SC, Vinay K, Tucker C, editors. The Heart. Robbins pathologic basis of disease. 1999. 6th ed. USA: W.B. Sanders Company;590–591.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download