Abstract
The authors assessed the efficacy and antiviral resistance of 48-week clevudine therapy versus lamivudine in treatment of naïve patients with HBeAg positive chronic hepatitis B. In this retrospective study, a total of 116 HBeAg positive patients, who received 30 mg of clevudine once daily (n=53) or 100 mg of lamivudine once daily (n=63) for 48 weeks, were included. At week 48, clevudine therapy produced a significantly greater mean reductions in serum HBV DNA levels from baseline than lamivudine therapy (-5.2 vs. -4.2 log10IU/mL; P=0.005). Furthermore, a significantly higher proportion of patients on clevudine achieved negative serum HBV DNA by PCR (<13 IU/mL) at week 48 (60.4% vs. 38.1%; P=0.025). The incidence of virologic breakthrough in the clevudine group was significantly lower than in the lamivudine group (9.4% vs. 25.4%; P=0.031). However, rates of alanine aminotransferase normalization and HBeAg loss or seroconversion were similar in the two groups (83.0% vs. 81.0%, 11.3% vs. 11.1%; P=0.813, 1.000, respectively). In conclusion, clevudine is more potent for viral suppression and lower for antiviral resistance at week 48 than lamivudine in treatment of naïve patients with HBeAg positive chronic hepatitis B.
Recent treatment guidelines and algorithms for the management of chronic hepatitis B (CHB) take into account the importance of prolonged viral suppression in terms of preventing disease progression and hepatocellular carcinoma (HCC) development (1-3). Currently available oral nucleos(t)ide analogues (NUC) for the treatment of CHB include lamivudine, adefovir, entecavir, telbivudine, and recently tenofovir (3). Although NUCs are more convenient than interferon-based therapies and have fewer side effects, sustained viral suppression is usually not achieved after a 48-week course of NUC therapy, which necessitates long, and in many cases, indefinite treatment (1). Unfortunately, protracted NUC treatment is associated with an elevated risk of development drug resistance (4). Developments of new antiviral agents and regimens remain an important focus in terms of improving reductions in viral loads and resistance profiles.
Clevudine (1-[2-doxy-2fluoro-β-L-arabinofuranosyl] thymine, L-FMAU) is a novel pyrimidine nucleoside analogue with an unnatural β-L configuration and potent antiviral activity in vitro and in a woodchuck model (5, 6). In a phase I/II dose-escalating clinical study and in a randomized phase II clinical trial, 4-week and 12-week clevudine therapy induced potent viral suppression at an optimal dosage of 30 mg once daily (7-9). In randomized phase III clinical trials, 24-week clevudine therapy showed a potent antiviral effect and produced significant biochemical improvements without evidence of viral resistance during the treatment period in HBeAg-positive and HBeAg-negative CHB (10, 11). The ability to maintain antiviral activity in a significant proportion of patients following the discontinuation of therapy is a unique characteristic of clevudine. The above results show that clevudine is probably one of the most potent antivirals available for the treatment of hepatitis B virus (HBV). Clevudine is already licensed in Korea for anti-HBV therapy (Bukwang Pharmaceuticals, Seoul), but previous clinical trials were placebo-controlled studies of relatively short treatment duration. Accordingly, we need to determine the longer-term treatment outcomes of clevudine therapy and to determine whether clevudine is superior to the preexisting oral NUC, lamivudine.
The aim of this study was to compare the antiviral efficacies and resistances of clevudine and lamivudine after 48 weeks of administration in naïve patients with hepatitis B e antigen (HBeAg) positive CHB. In addition, we also analyzed associations between early viral suppression during therapy and 48 week treatment outcomes.
This was an open-labeled, retrospective, nonrandomized, comparative study. Data were collected from the medical records of all patients with CHB treated with clevudine or lamivudine at two tertiary referral hospitals, namely, Chonbuk National University Hospital and Wonkwang University Hospital, between January 2007 and December 2008. Patients with CHB who received either 30 mg of clevudine orally once daily or 100 mg of lamivudine orally once daily for at least 48 weeks were included in this analysis. Patients were eligible if they were 18-70 yr of age and had HBeAg positive CHB or compensated liver cirrhosis. CHB was defined as a detectable serum hepatitis B surface antigen (HBsAg) level for more than 6 months, a serum HBV DNA level greater than 105 copies/mL (or ≥20,000 IU/mL), and a serum alanine aminotransferase (ALT) level 1.5-10 times the upper limit of normal. Liver cirrhosis was demonstrated mainly by ultrasonography (i.e., a coarse liver architecture, a nodular liver surface, and blunt liver edges) and evidence of hypersplenism (i.e., splenomegaly on ultrasonography and a platelet count of <100,000/µL). Patients with decompensated liver disease or biochemical signs of renal impairment (a serum creatinine of ≥1.5 mg/dL or a creatinine clearance of <50 mL/min, as determined by the Cockroft method) were excluded. The other exclusion criteria applied were as follows: prior treatment with anti-HBV NUCs or interferon; coinfection with human immunodeficiency virus, hepatitis C virus, or hepatitis delta virus; a history of alcohol or drug abuse within the preceding 2 yr; documented or suspected HCC; prior organ transplantation; or pregnancy/lactation.
A total of 116 patients were included in this analysis. Fifty-three patients were treated with clevudine for 48-96 (median 71.2) weeks and sixty-three with lamivudine for 48-108 (median 82.4) weeks. Routine blood tests and liver enzymes were performed every 3 months and adverse events were assessed at each visit. Liver panel, creatinine, HBeAg, anti-HBe, and quantitative HBV DNA were checked at commencement of therapy, and then every 3 months in all patients. All 116 patients were included in the analysis of treatment outcomes at 24 and 48 weeks. The myopathy associated with clevudine therapy has not been well defined by previous clinical trials, and therefore, serum creatine kinase (CK) was not checked regularly during this study. Only patients who presented with progressive proximal muscular weakness were tested for serum CK level. This study was conducted in compliance with the World Medical Association Declaration of Helsinki and was approved by the Ethics Committee at our institution (CBIRB 1003-30).
HBsAg, anti-HBs, HBeAg, and anti-HBe were detected using commercial enzyme-linked immunosorbent assay (ELISA) kits (AXSYM, Abbott Laboratories, Chicago, IL, USA). Serum HBV DNA levels were determined using polymerase chain reaction (PCR) assays (mainly real-time PCR assays) using the COBAS TaqMan HBV Test (Roche Diagnostics, Branchberg, NJ, USA; detection limit 13 IU/mL). In a small proportion of patients, the COBAS Amplicor HBV Monitor Test (Roche Diagnostics) with a detection limit of 300 copies/mL was used to quantify serum HBV DNA level at baseline. We rechecked serum HBV DNA levels by real-time PCR in patients with an undetectable HBV DNA level using the Amplicor PCR assay during treatment. The World Health Organization (WHO) has established an international reference standard for HBV DNA testing based on IU/mL (12). To compare serum HBV levels expressed in different units, we converted 'copies/mL' of serum HBV DNA levels to 'IU/mL' using (1 IU/mL=5.6 copies/mL), which was provided by the manufacturer (13).
Genotypic analysis of HBV DNA polymerase was performed in patients showing virologic breakthrough during therapy using a matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) based genotyping assay, termed the Restriction Fragment Mass Polymorphism (RFMP) assay, as previously described (14).
The primary endpoints of this study were a reduction in serum HBV DNA at week 48 versus baseline, and the proportions of patients that achieved undetectable serum HBV DNA levels by PCR (<13 IU/L) and serum ALT normalization (≤40 IU/L). The secondary endpoints included the proportion of patients showing HBeAg loss or seroconversion, primary treatment failure, and virologic breakthrough. Primary treatment failure was defined as the inability of antiviral treatment to reduce serum HBV DNA by ≥1 log10IU/mL after the first 3 months of treatment (15). Virologic breakthrough, which is usually associated with drug resistance, was defined as a ≥1 log10IU/mL increase in serum HBV DNA level from its nadir in two consecutive samples 1 month apart while on treatment, after achieving an initial response, in medically compliant patients on antiviral medication(s) (15).
Data from all study subjects were pooled, regardless of treatment group, and subjects were categorized according to serum HBV DNA level at week 24; undetectable (<13 IU/mL), from 13 to <200 IU/mL, from 200 to <2,000 IU/mL, and ≥2,000 IU/mL. Treatment outcomes at week 48, including, HBV DNA non-detectability, HBeAg loss or seroconversion, ALT normalization, and viral breakthrough were analyzed according to residual serum HBV DNA category at week 24.
Results are reported as means±standard deviations (SD). HBV DNA levels were logarithmically transformed for analysis. Continuous variables were compared using the 2-tailed Student's t-test. Categorical data were analyzed using the chi-square test or Fisher's exact test. Factors associated with viral breakthrough were analyzed by univariate analysis and multivariate logistic regression analysis. P values of <0.05 were considered statistically significant. Data was collated in Microsoft EXCEL (Microsoft Excel 2003; Microsoft Corporation, Seattle, WA, USA), and analyzed using SPSS for Windows (version 15.0; SPSS Inc., Chicago, IL, USA).
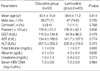
Of the 116 patients, 85 (73.3%) were male with a mean age of 40.2 yr and 12 (10.3%) patients had compensated cirrhosis. The two treatment groups were comparable with respect to demographic and baseline laboratory features, including age, sex, presence of cirrhosis, serum ALT level, and serum HBV DNA level (Table 1).
Serum HBV DNA levels declined markedly after treatment commencement in both treatment groups. Clevudine had a more potent antiviral effect at week 24, and subsequently the mean reduction in serum HBV DNA level remained consistently greater in the clevudine group than in the lamivudine group (Fig. 1). At week 24, mean reductions of serum HBV DNA levels from baseline were -5.0 vs. -4.2 log10IU/mL in the clevudine and lamivudine groups, respectively (P=0.007). Furthermore, mean reduction of serum HBV DNA level from baseline at week 48 was significantly greater in the clevudine group (-5.2 vs. -4.2 log10IU/mL; P=0.005) and a significantly higher proportion of patients on clevudine achieved negative serum HBV DNA by PCR (<13 IU/mL) at week 48 (60.4% vs. 38.1%; P=0.025) (Table 2). Group distributions of patients according to serum HBV DNA levels at weeks 24 and 48 are shown in Fig. 2. At week 24, more patients in the clevudine group than in the lamivudine group were non-detectable for serum HBV DNA level by PCR (<13 IU/mL), whereas residual serum HBV DNA levels greater than 2,000 IU/mL were more frequent in patients in the lamivudine group than in those in the clevudine group (P=0.041). The distribution of patients according to HBV DNA levels at week 48 was also consistent with the greater early viral suppression observed with clevudine (P=0.002).
However, clevudine and lamivudine treated patients had similar biochemical and serological responses. At week 48, 83.0% in the clevudine group and 81.0% in the lamivudine group had achieved serum ALT level normalization (P=0.813), and the rate of HBeAg loss and/or HBeAg seroconversion was 11.3% in the clevudine group and 11.1% in the lamivudine group (P=1.000) (Table 2).
Five (9.4%) of the 53 clevudine treated patients and 16 (25.4%) of the 63 lamivudine treated patients showed virologic breakthrough during the 48-week treatment period. The clevudine group had a significantly lower rate of virologic breakthrough than the lamivudine group (P=0.031) (Table 2). In addition, three (4.8%) patients in the lamivudine group but no patient in the clevudine group showed primary treatment failure (P=0.249).
Mutations associated with resistance to clevudine and lamivudine were analyzed using RFMP assays in all patients that developed viral breakthrough during therapy. Of the 5 patients in the clevudine group with viral breakthrough, 4 patients had the rtM204I mutation alone and one patient harbored rtM204I+rtL180M mutations. Of the 16 patients in the lamivudine group with viral breakthrough, 8 patients had rtM204V±rtL180M mutations, 7 patients had rtM204I mutation±tL180M mutations, and one patient had the rtM204I+rtM204V+rtL180M mutations.
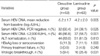
We assessed factors associated with virologic breakthrough over the 48-week treatment period by univariate analysis (Table 3). In the clevudine group, age, sex, presence of cirrhosis, baseline serum ALT and baseline serum HBV DNA levels, and serum HBV DNA level (≥2,000 IU/mL at week 24) were not found to be associated with virologic breakthrough. However, in the lamivudine group, virologic breakthrough was found to be associated with a high baseline serum HBV DNA level (P=0.001), and a serum HBV DNA level of ≥2,000 IU/mL at week 24 (P=0.014).
We also analyzed factors associated with virologic breakthrough by logistic regression analysis after pooling data from all study subjects (Table 4). It was found that baseline serum HBV DNA level (odds ratio 3.13, 95% confidence interval 1.22-7.99; P=0.017), serum HBV DNA level at week 24 (≥2,000 IU/mL vs. <2,000 IU/mL) (odds ratio 3.87, 95% confidence interval 1.28-11.74; P=0.017), and treatment type (lamivudine vs clevudine) (odds ratio 3.86, 95% confidence interval 1.16-12.82; P=0.027) were significantly associated with virologic breakthrough.
Data from all study subjects were pooled, and categorized according to serum HBV DNA level at week 24. Treatment outcomes at week 48 were found to be strongly associated with degree of viral suppression at week 24 (Fig. 3). As shown in Fig. 3, the likelihood of HBV DNA becoming undetectable at week 48 was found to be inversely related to viral load at week 24. Furthermore, 32 (94.1%) of the 34 patients with an undetectable HBV DNA level by PCR (<13 IU/mL) at week 24 maintained an undetectable HBV DNA level at week 48, whereas only 3 (8.3%) of 36 patients with a serum HBV DNA level ≥2,000 IU/mL at week 24 achieved an undetectable HBV DNA level at week 48. Rates of HBeAg loss or seroconversion and ALT normalization at week 48 were also higher in patients with a non-detectable serum HBV DNA level at week 24 than in patients with a residual viral load of ≥2,000 IU/mL (23.5% vs. 0%, 88.2# vs. 66.7#, respectively). Moreover, at week 48, viral breakthrough occurred in only 1 (2.9#) of 34 patients with a non-detectable HBV DNA level at week 24, as compared with 13 (36.1#) of 36 patients with residual viremia of ≥2,000 IU/mL at week 24.
During the treatment period, no specific serious adverse event was encountered in any patient. Adverse events occurred with similar frequencies in both groups. The most frequent HBV, hepatitis B virus. adverse events in both groups were; fatigue, upper respiratory symptoms, headache, and dyspepsia. However, all symptoms were mild and relatively well tolerated. No significant changes were observed over the treatment period in serum creatinine or in any other laboratory parameter, and no patient with cirrhosis in either group experienced hepatic decompensation.
In this retrospective study, clevudine (30 mg daily for 48 weeks) showed potent antiviral activity in HBeAg positive CHB patients. In particular, it suppressed mean serum HBV DNA by -5.2 log10IU/mL during the 48-week treatment period, and 60.4% of clevudine treated patients had an undetectable serum HBV DNA level by PCR assay after treatment. Although this study was not randomized and the study groups were not matched on a patient-to-patient basis, the degree of HBV DNA reduction achieved by clevudine at 30 mg daily at week 48 was found to be significantly greater than that achieved by lamivudine at 100 mg daily (-5.2 log10IU/mL vs. -4.2 log10IU/mL; P=0.005). Furthermore, the proportion of patients that achieved a non-detectable serum HBV DNA level by PCR (<13 IU/mL) at week 48 was also significantly greater in the clevudine group (60.4% vs. 38.1%; P=0.025). Clevudine also showed potent early virologic response, and this was greater than that achieved by lamivudine. At week 24, mean serum HBV DNA reductions from baseline and the proportion of patients with a serum HBV DNA level of <2,000 IU/mL at week 24 were also significantly greater in the clevudine group. In a previous 24-week clevudine treatment study (11), 68.2% of patients achieved serum ALT normalization, which concurs with the high normalization rate of 83.3% at week 48 found in the present study. However, despite the more potent antiviral suppression of clevudine, clevudine and lamivudine induced similar biochemical and serological responses.
The presence of drug-resistant mutations is a primary concern when considering oral NUC therapy. In previous 24-week treatment trials, clevudine showed no virologic breakthrough (10, 11). In contrast, during the present 48-week study, virologic breakthrough occurred in 9.4% of clevudine treated patients. When we compared this with that of the lamivudine group, it was found that the incidence of virologic breakthrough was significantly lower in the clevudine group (9.4% vs. 25.4%; P=0.031). A recent study from Korea found that rates of viral breakthrough at 1 yr were 10.0% in treatment naïve patients and 44.4% in patients with a history of previous lamivudine treatment (P<0.001) (16). These results indicate that viral breakthrough during clevudine therapy is not negligible in treatment naïve CHB patients. Furthermore, previous lamivudine treatment was found to be associated with a substantially higher rate of viral breakthrough, which may have been due to an increased risk of cross resisresistance between two drugs. Therefore, care is required when clevudine is administered to patients previously treated with lamivudine. In addition, the cumulative incidence of clevudine resistance is likely to increase with therapy duration. More long-term studies are needed to understand the cumulative incidences and clinical effects of resistance to clevudine.
Our resistance profiles confirm that the rtM204I mutation is the primary clevudine resistance mutation. Lee et al. also reported that rtM204I is most common mutation of HBV DNA polymerase in treatment naïve patients; other sites of mutation were rtL80I, rtL180M, rtA181V/T, rtV207I (16). Furthermore, the rtM204I mutation is cross resistant with other L-nucleosides, such as, lamivudine, emtricitabine, and telbivudine (15, 17). In vitro studies have demonstrated that adefovir, tenofovir, and entecavir have antiviral activity against L-nucleoside-resistant HBV mutants, but the activity of entecavir against these mutants is substantially lower than against wild type HBV (17). In previous studies in patients with lamivudine-resistant CHB, a combination of lamivudine and adefovir was found to be more effective at preventing subsequent adefovir resistance (18, 19). Tenofovir has also been shown to be effective in patients with HBV resistance to both lamivudine and adefovir (20), on the other hand, entecavir monotherapy was found to have a high risk of entecavir resistance in lamivudine-resistant patients (21). Accordingly, the addition of adefovir or tenofovir may be preferable to switching to adefovir or entecavir in patients with clevudine-resistant CHB.
We also assessed factors associated with virologic breakthrough. By univariate analysis, virologic breakthrough in the clevudine group was not found to be associated with baseline factors or early viral response. However, because the number of patients with virologic breakthrough was small in the clevudine group, statistical power may have been underestimated. By multivariate analysis after pooling data from all study subjects, regardless of treatment group, baseline serum HBV DNA level (odds ratio 3.13, 95% confidence interval 1.22-7.99; P=0.017), serum HBV DNA level at week 24 (≥2,000 IU/mL vs. <2,000 IU/mL) (odds ratio 3.87, 95% confidence interval 1.28-11.74; P=0.017), treatment type (lamivudine vs. clevudine) (odds ratio 3.86, 95% confidence interval 1.16-12.82; P=0.027) were found to be significantly associated with virologic breakthrough.
In the clinical trials of agents with lower genetic barriers to viral resistance, such as, lamivudine and telbivudine, early maximal reductions in HBV DNA levels at 24 weeks were found to predict improved clinical outcomes at 1 and 2 yr (22-24). Similar trends were observed in the present study. When we pooled data from all of our study subjects and examined relations between treatment outcomes at week 48 with respect to serum HBV DNA levels at week 24, it was found that treatment outcomes at week 48 were strongly associated with degree of viral suppression at week 24. Patients with an undetectable HBV DNA level by PCR at week 24 showed higher rates of HBV DNA non-detectability, HBeAg loss or seroconversion, ALT normalization, and a lower rate of viral breakthrough than those with residual viral viremia of ≥2,000 IU/mL at week 24. The results of the present study support the utility of the recently proposed 'roadmap' concept as a strategy to improve long-term treatment results (3).
Previous 24-week clinical trials have shown that the incidences of adverse events are similar for patients on clevudine or placebo (10, 11). We also encountered no meaningful serious adverse events in either treatment group. However, a recent study reported that the long-term use of clevudine can induce mitochondrial DNA depletion and lead to mitochondrial myopathy associated with myonecrosis (25). Lee et al. also reported that 10 of 339 (2.9%) patients complained of prominent fatigue and had elevated serum levels of aspartate aminotransferase and CK after 1 yr of clevudine therapy. Furthermore, two of these patients presented with severe myopathy, from which they recovered completely after quitting clevudine. We also reviewed the follow up medical records and laboratory data of both treatment groups after 48 weeks. Myopathy, characterized by muscle pain and weakness and moderately elevated CK levels during treatment, was observed in three (5.7%) of patients in the clevudine group and none of those in the lamivudine group. All three patients who developed myopathy during clevudine therapy were treated with clevudine for more than 52 weeks (52-60 weeks). When clevudine was discontinued, CK levels returned to normal within 2 months and symptoms resolved over a period of 2 to 4 months in all patients. Therefore, we suggest that patients on long-term clevudine therapy should be monitored carefully for skeletal muscle dysfunction.
In conclusion, we found that 48-week clevudine therapy induced more potent, earlier virologic response and produced better treatment outcomes at 48 weeks than lamivudine in patients with HBeAg positive CHB. Nevertheless, viral breakthrough was observed during the 48-week clevudine administration period. Furthermore, treatment outcomes at week 48, in both treatment groups, were found to be strongly associated with degree of viral suppression at week 24. The present study is limited by its open-label, nonrandomized, retrospective design. Accordingly, a longer-term, randomized, controlled clinical trial is needed to confirm our preliminary findings.
Figures and Tables
Fig. 1
Mean reductions of serum HBV DNA levels during the study period. At weeks 24, 36, and 48, clevudine therapy produced a significantly greater mean reduction in serum HBV DNA level from baseline than lamivudine therapy
*P=0.007; †P<0.001; and ‡P=0.005, respectively.
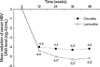
Fig. 2
Patient distributions with respect to serum HBV DNA levels. The distributions of patients according to HBV DNA levels at week 24 and 48 were consistent with the greater viral suppression observed with clevudine (*P=0.041 and †P=0.002, respectively).

Fig. 3
Effect of early viral response on treatment outcomes at week 48. Treatment outcomes at week 48 were found to be strongly associated with degree of viral suppression at week 24.

References
2. European Association for the Study of the Liver. EASL Clinical Practice Guidelines: management of chronic hepatitis B. J Hepatol. 2009. 50:227–242.
3. Keeffe EB, Dieterich DT, Han SH, Jacobson IM, Martin P, Schiff ER, Tobias H. A treatment algorithm for the management of chronic hepatitis B virus infection in the United States: 2008 update. Clin Gastroenterol Hepatol. 2008. 6:1315–1341.

4. Fung SK, Lok AS. Management of hepatitis B patients with antiviral resistance. Antivir Ther. 2004. 9:1013–1026.
5. Balakrishna Pai S, Liu SH, Zhu YL, Chu CK, Cheng YC. Inhibition of hepatitis B virus by a novel L-nucleoside, 2'-fluoro-5-methyl-beta-L-arabinofuranosyl uracil. Antimicrob Agents Chemother. 1996. 40:380–386.

6. Chin R, Shaw T, Torresi J, Sozzi V, Trautwein C, Bock T, Manns M, Isom H, Furman P, Locarnini P. In vitro susceptibilities of wild-type or drug-resistant hepatitis B virus to (-)-beta-D-2,6-diaminopurine dioxolane and 2'-fluoro-5-methyl-beta-L-arabinofuranosyluracil. Antimicrob Agents Chemother. 2001. 45:2495–2501.
7. Marcellin P, Mommeja-Marin H, Sacks SL, Lau GK, Sereni D, Bronowicki JP, Conway B, Trepo C, Blum MR, Yoo BC, Mondou E, Sorbel J, Snow A, Rousseau F, Lee HS. A phase II dose-escalating trial of clevudine in patients with chronic hepatitis B. Hepatology. 2004. 40:140–148.

8. Lee HS, Chung YH, Lee K, Byun KS, Paik SW, Han JY, Yoo K, Yoo HW, Lee JH, Yoo BC. A 12-week clevudine therapy showed potent and durable antiviral activity in HBeAg-positive chronic hepatitis B. Hepatology. 2006. 43:982–988.

9. Lim SG, Leung N, Hann HW, Lau GK, Trepo C, Mommeja-Marin H, Moxham C, Sorbel J, Snow A, Blum MR, Rousseau F, Marcellin P. Clinical trial: a phase II, randomized study evaluating the safety, pharmacokinetics and anti-viral activity of clevudine for 12 weeks in patients with chronic hepatitis B. Aliment Pharmacol Ther. 2008. 27:1282–1292.
10. Yoo BC, Kim JH, Kim TH, Koh KC, Um SH, Kim YS, Lee KS, Han BH, Chon CY, Han JY, Ryu SH, Kim HC, Byun KS, Hwang SG, Kim BI, Cho M, Yoo K, Lee HJ, Hwang JS, Kim YS, Lee YS, Choi SK, Lee YJ, Yang JM, Park JW, Lee MS, Kim DG, Chung YH, Cho SH, Choi JY, Kweon YO, Lee HY, Jeong SH, Yoo HW, Lee HS. Clevudine is highly efficacious in hepatitis B e antigen-negative chronic hepatitis B with durable off-therapy viral suppression. Hepatology. 2007. 46:1041–1048.

11. Yoo BC, Kim JH, Chung YH, Lee KS, Paik SW, Ryu SH, Han BH, Han JY, Byun KS, Cho M, Lee HJ, Kim TH, Cho SH, Park JW, Um SH, Hwang SG, Kim YS, Lee YJ, Chon CY, Kim BI, Lee YS, Yang JM, Kim HC, Hwang JS, Choi SK, Kweon YO, Jeong SH, Lee MS, Choi JY, Kim DG, Kim YS, Lee HY, Yoo K, Yoo HW, Lee HS. Twenty-four-week clevudine therapy showed potent and sustained antiviral activity in HBeAg-positive chronic hepatitis B. Hepatology. 2007. 45:1172–1178.

12. Saldanha J, Gerlich W, Lelie N, Dawson P, Heermann K, Heath A. WHO Collaborative Study Group. An international collaborative study to establish a World Health Organization international standard for hepatitis B virus DNA nucleic acid amplification techniques. Vox Sang. 2001. 80:63–71.

13. Gish RG, Locarnini SA. Chronic hepatitis B: current testing strategies. Clin Gastroenterol Hepatol. 2006. 4:666–676.

14. Hong SP, Kim NK, Hwang SG, Chung HJ, Kim S, Han JH, Kim HT, Rim KS, Kang MS, Yoo W, Kim SO. Detection of hepatitis B virus YMDD variants using mass spectrometric analysis of oligonucleotide fragments. J Hepatol. 2004. 40:837–844.
15. Lok AS, Zoulim F, Locarnini S, Bartholomeusz A, Ghany MG, Pawlotsky JM, Liaw YF, Mizokami M, Kuiken C. Hepatitis B Virus Drug Resistance Working Group. Antiviral drug-resistant HBV: Standardization of nomenclature and assays and recommendations for management. Hepatology. 2007. 46:254–265.

16. Lee HJ, Eun JR, Lee CH, Hwang JS, Suh JI, Kim BS, Jang BK. Long-term clevudine therapy in nucleos(t)ide-naïve and lamivudine-experienced patients with hepatitis B virus-related chronic liver diseases. Korean J Hepatol. 2009. 15:179–192.

17. Yang H, Qi X, Sabogal A, Miller M, Xiong S, Delaney WE 4th. Cross-resistance testing of next-generation nucleoside and nucleotide analogues against lamivudine-resistant HBV. Antivir Ther. 2005. 10:625–633.
18. Lampertico P, Viganó M, Manenti E, Iavarone M, Sablon E, Colombo M. Low resistance to adefovir combined with lamivudine: a 3-year study of 145 lamivudine-resistant hepatitis B patients. Gastroenterology. 2007. 133:1445–1451.

19. Manolakopoulos S, Bethanis S, Koutsounas S, Goulis J, Vlachogiannakos J, Christias E, Saveriadis A, Pavlidis C, Triantos C, Christidou A, Papatheodoridis G, Karamanolis D, Tzourmakliotis D. Long-term therapy with adefovir dipivoxil in hepatitis B e antigen-negative patients developing resistance to lamivudine. Aliment Pharmacol Ther. 2008. 27:266–273.

20. van Bömmel F, Zollner B, Sarrazin C, Spengler U, Hüppe D, Müller B, Feucht HH, Wiedenmann B, Berg T. Tenofovir for patients with lamivudine-resistant hepatitis B virus (HBV) infection and high HBV DNA level during adefovir therapy. Hepatology. 2006. 44:318–325.

21. Sherman M, Yurdaydin C, Sollano J, Silva M, Liaw YF, Cianciara J, Boron-Kaczmarska A, Martin P, Goodman Z, Colonno R, Cross A, Denisky G, Kreter B, Hindes R. AI463026 BEHoLD Study Group. Entecavir for treatment of lamivudine-refractory, HBeAg-positive chronic hepatitis B. Gastroenterology. 2006. 130:2039–2049.

22. Lai CL, Leung N, Teo EK, Tong M, Wong F, Hann HW, Han S, Poynard T, Myers M, Chao G, Lloyd D, Brown NA. Telbivudine Phase II Investigator Group. A 1-year trial of telbivudine, lamivudine, and the combination in patients with hepatitis B e antigen-positive chronic hepatitis B. Gastroenterology. 2005. 129:528–536.

23. Liaw YF, Gane E, Leung N, Zeuzem S, Wang Y, Lai CL, Heathcote EJ, Manns M, Bzowej N, Niu J, Han SH, Hwang SG, Cakaloglu Y, Tong MJ, Papatheodoridis G, Chen Y, Brown NA, Albanis E, Galil K, Naoumov NV. GLOBE Study Group. 2-Year GLOBE trial results: telbivudine is superior to lamivudine in patients with chronic hepatitis B. Gastroenterology. 2009. 136:486–495.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download