Abstract
To evaluate the effects of cyclosporin A (CyA) on clinical outcome and pathologic changes in children with IgA nephropathy (IgAN), we retrospectively evaluated 14 children (mean age 8.9±2.9 yr; eight males, six females) who were treated with CyA and steroids. The starting dose of CyA was 5 mg/kg per day, and the drug level was maintained at 100-200 ng/mL. The mean CyA level was 183.8±48.3 ng/mL (range 120.7-276.0 ng/mL) and the mean duration of CyA therapy was 10.9±1.9 months (range 8-12 months). After CyA therapy the mean 24 hr urinary protein excretion declined from 107.1±35.1 mg/m2/hr to 7.4±2.4 mg/m2/hr (P<0.001) and serum albumin increased from 3.3±0.6 g/dL to 4.3±0.3 g/dL (P<0.001). At a follow-up biopsy the histological grade of IgAN was improved in seven (50%) of the 14 patients, remained the same in three (21%), and was aggravated in four (29%). Serum creatinine, creatinine clearance, and blood pressure did not differ before and after CyA therapy. Two patients (14%) showed CyA-induced nephrotoxicity at the second biopsy. Our findings indicate that CyA therapy may be effective in reducing proteinuria and regressing renal pathology in a subset of children with IgAN.
IgA nephropathy (IgAN) was first described by Berger and Hinglais in 1968 and is now recognized to be the most common form of primary glomerulonephritis worldwide (1, 2). The clinical course of IgAN is variable, with some patients having stable renal function over decades and others developing hypertension, nephrotic syndrome, and chronic renal failure (3). About 20-50% of adult patients with IgAN develop progressive renal failure, but the pathogenesis remains unknown and a treatment regimen has not been established (4). Although children have been reported to have a more benign prognosis for IgAN than adults, recent studies show that IgAN in children is not an entirely benign disease (4).
Cyclosporin A (CyA) is a potent immunosuppressive drug that is frequently used in the therapy of various immune-mediated glomerular diseases (5). Several reports have indicated its potential role in treating IgAN with encouraging results, such as significant reduction of proteinuria, in small randomized clinical trials or small uncontrolled trials (6-8). However, the histological effects of CyA in children with IgAN have not been reported previously.
The aim of this study was to evaluate the clinical and histological effects of CyA in children with IgAN.
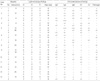
We retrospectively reviewed the charts of 14 patients (mean age 8.9±2.9 yr; eight males, six females) with IgAN who were treated with CyA and prednisolone from 1993 to 2001 (Table 1). Ten of the 14 children were ≤10 yr old. The median duration of follow-up was 4.6 yr (range 1.4-11 yr). All patients underwent a renal biopsy within one or two months before CyA therapy and a follow-up biopsy after CyA therapy. The glomerular changes were categorized according to the Haas classification (9): subclass I, minimal or no mesangial hypercellularity without glomerular sclerosis; subclass II, focal and segmental glomerular sclerosis without active cellular proliferation; subclass III, focal proliferative glomerulonephritis; subclass IV, diffuse proliferative glomerulonephritis; and subclass V, any biopsy showing ≥40% globally sclerotic glomeruli and/or ≥40% estimated cortical tubular atrophy or loss.
Renal biopsy specimens were also scored semiquantitatively using the modified scoring system of Andreoli et al. (10) and Foster et al. (11). Acute changes included mesangial hypercellularity (scored 0-3), mesangial matrix expansion (0-3), interstitial mononuclear infiltrate (0-2), cellular crescents (0-3), and basement membrane adhesion to Bowman's capsule (0-3). Chronic renal injury was scored by interstitial fibrosis and tubular atrophy (0-2), fibrous crescents (0-3), and segmental or global sclerosis (0-3). The sum of these scores for acute and chronic injury constituted the activity index and the chronicity index, respectively. Interstitial mononuclear infiltrate, interstitial fibrosis, and tubular atrophy were combined to give the tubulointerstitial (TI) scores. For immunofluorescent (IF) microscopy, a portion of fresh renal tissue was frozen and stained with fluorescein isothiocyanate (FITC)-conjugated antibodies against human IgG, IgA, IgM, C3, C4, and fibrinogen. The overall intensity of IF was scored semiquantitatively, where 0=negative, 0.5=trace (+/-), 1=mild (+), 2=moderate (++), and 3=severe (+++). We also performed electron microscopy on the biopsy specimens to confirm the mesangial location of the deposits.
CyA (Cipol-N, Chong Kun Dang Pharma, Seoul, Korea) was administered to patients with severe nephritis defined as nephrotic syndrome, heavy proteinuria (>1 g/day), or biopsy specimen class III or more, except for one patient (No. 7) who received CyA because of persistent proteinuria. The starting dose of CyA was 5 mg/kg/day and the blood level was maintained at 100-200 ng/mL. We monitored the CyA level weekly at the beginning of treatment and thereafter every month. The mean (±SD) CyA level was 183.8±48.3 ng/mL (range 120.7-276 ng/mL) and the mean duration of CyA therapy was 10.9±1.9 months (range 8-12 months). Prednisolone (1-2 mg/kg/day) was given in three divided doses for four weeks and was gradually reduced to a single dose of 5-10 mg/day on alternate days during CyA therapy. The median duration of prednisolone tapering was 3.2 yr (range 1.4-8.5 yr). An angiotensin converting enzyme (ACE) inhibitor (captopril or cilazapril) was concurrently used in 12 patients (median treatment time 3.5 yr, range 1.7-5.2 yr) and calcium channel blocker in 10 patients (median three yr, range 1-3.7 yr).
Clinical state at the end of CyA therapy or at the latest observation was classified as follows (12): A, normal urine and renal function; B, microscopic hematuria without proteinuria (B1), or proteinuria of <40 mg/m2/hr with or without hematuria (B2); C, active renal disease with proteinuria of >40 mg/m2/hr and GFR of ≥60 mL/min/1.73 m2; D, renal insufficiency.
Statistical analysis was performed using the Medcalc statistical package. Continuous variables were expressed as mean±standard deviation (SD) or standard error of the mean (SEM), or as a median with ranges. Differences between biopsy findings before and after therapy were assessed by Wilcoxon's signed rank test. P<0.05 was considered significant.
Clinical characteristics of the 14 patients with IgAN are shown in Table 1. Five patients had non-nephrotic proteinuria (one class II, one class III, three class IV), seven had nephrotic-range proteinuria (three class III, four class IV), and two had nephrotic syndrome (class IV). Gross hematuria was present in 10 patients and one showed acute renal failure at presentation (No. 11). At the end of CyA therapy, two patients showed normal urinalysis and renal function (state A) findings, nine had microscopic hematuria without proteinuria (state B1), two had proteinuria of <40 mg/m2/hr (state B2), and one had active renal disease with proteinuria of >40 mg/m2/hr (state C). At the latest follow-up, six patients showed state A, three state B1, three state B2, and two state C (Fig. 1). CyA was well tolerated in all patients and none required drug discontinuation or had any adverse event that warranted hospitalization.
The mean 24-hr urinary protein excretion declined from 107.1±35.1 mg/m2/hr to 7.4±2.4 mg/m2/hr (P<0.001) (Fig. 2) and serum albumin increased from 3.3±0.6 g/dL to 4.3±0.3 g/dL (P<0.001) after CyA therapy. Serum creatinine, creatinine clearance, systolic blood pressure, and diastolic blood pressure did not differ before and after CyA therapy (Table 2).
Light microscopic and IF findings of the 14 patients are shown in Table 3. At a follow-up biopsy the histological grade of IgAN was improved in seven (50%) of the 14 patients, remained the same in three (21%), and was aggravated in four (29%) (pre-therapy: one class II, four class III, and nine class IV; post-therapy: two class I, one class II, six class III, four class IV, and one class V). Two (Nos. 9, 13) of the four patients (Nos. 1, 7, 9, 13) who had aggravated Haas classes also showed an improvement in clinical state at the last follow-up (state B1 → A).
The activity index decreased from 5.1±1.9 to 3.9±2.1, but this decrease was not statistically significant (P=0.121). The chronicity index and tubulointerstitial scores did not differ before and after CyA therapy. Two patients (14%) showed possible CyA-induced nephrotoxicity at a second biopsy (No. 3, TI score 1 → 4; No. 5, TI score 2 → 4), but one patient (No. 5) showed an improvement of TI score (score 1) at the third biopsy performed eight yr later. IF analysis at the first and second biopsy showed that mesangial IgA depositions were reduced in seven (50%) of the 14 patients (Table 3).
IgAN is the most common form of glomerulonephritis throughout the world and has a very heterogeneous clinical course, leading to end-stage renal failure in 20-30% of patients over 20 yr (1-4, 13). Despite the fact that IgAN patients with hypertension, renal insufficiency, heavy proteinuria, and severe histological findings at presentation are at a high risk of developing end stage renal failure (14), there is no consensus for the treatment of patients with IgAN. Although not established in clinical practice, several types of treatment, including steroids, ACE inhibitors, cytotoxics, immunosuppressants, tonsillectomy, fish oil, and vitamin E, either alone or in various combinations, have been used to modulate the rate of progression (15).
CyA has been used as a useful therapeutic agent in various glomerular diseases (5). The action mechanism of CyA in these conditions is not known, but may involve the following: 1) immunomodulation by T-cell mediated cytokines, resulting in restoration of glomerular basement membrane charge selectivity (6, 16); 2) inhibition of vascular permeability factor (17); or 3) non-specific alteration of renal hemodynamics, resulting in reduction of proteinuria (18).
There have been only a few clinical trials on the use of CyA for adults with IgAN (6, 7) and even fewer on the efficacy of CyA in childhood IgAN (8). Furthermore, the histological effect of CyA on childhood IgAN has not been reported previously.
The first randomized prospective single-blind study of CyA in adults with IgAN indicated that short term CyA therapy was beneficial in reducing proteinuria in some patients with IgAN, but transient renal impairment was observed despite maintaining CyA concentrations within a narrow therapeutic range (6). Therefore, the authors concluded that indiscriminate use of CyA in IgAN should be discouraged.
Another study also demonstrated that CyA significantly reduced moderate to high proteinuria with a much lower decrease of GFR in six adults (four males, two females; aged 21-31 yr) with IgAN and proteinuria >3.5 g/day that did not respond to corticosteroids (7). The authors speculated that the significant decrease in the proteinuria/GFR ratio strongly suggests some non-hemodynamic mechanism of CyA action. In one of the few studies on the use of CyA in young children with IgAN, we previously demonstrated a beneficial effect of CyA on relapsing nephrotic syndrome associated with IgAN in two children (8).
Although CyA did not cause histological changes in ddY mice, an animal model of IgAN (19), the current study showed that CyA therapy was effective in regressing renal histologic changes in a subset of patients (about 50%) with IgAN. Allen et al. (20) also found that CyA suppressed IgA production by peripheral blood mononuclear cells from patients with IgAN, and Lai et al. (6) demonstrated that serum IgA concentrations were reduced after CyA therapy in seven of 19 patients with IgAN. Our rationale for using CyA in childhood IgAN was that these immunosuppressive drugs might reduce IgA production, and thus alleviate the abnormal immune response and inflammatory reactions to IgA-mediated immune deposits. However, the concurrent use of steroids or ACE inhibitor might also play a role in reducing the degree of proteinuria in our patients (21-23). Recently, Yoshikawa et al. (22) confirmed the beneficial effect of steroids on childhood IgAN and an European placebo-controlled, randomized trial of ACE inhibitor showed that treatment with ACE inhibitor was an independent predictor of prognosis in children and young people with IgA nephropathy and moderate proteinuria (23). We also used calcium channel blockers for their additional renoprotective effects beyond lowering blood pressure (24). Therefore, we cannot conclude that the histological regression of IgAN observed in our study was due only to CyA therapy.
Although there were no serious complications of CyA therapy during the period of study, two patients had chronic CyA-induced nephrotoxicity at a second biopsy. Therefore, it is important to use the lowest effective dosage of CyA and to monitor the CyA level closely. In addition, this study has the following limitations: small sample size, retrospective study design, lack of a control group receiving steroids or ACE inhibitor alone, and the relatively short length of treatment and follow-up.
In conclusion, our study is the first systematic analysis of CyA use in childhood IgAN and suggests that CyA combined with steroids and ACE inhibitor may be effective in reducing proteinuria and attenuating histologic progression in a proportion of children with IgAN.
References
1. Berger J, Hinglais N. Intercapillary deposits of IgA-IgG. J Urol Nephrol (Paris). 1968. 74:694–695.
3. D'Amico G. Natural history of idiopathic IgA nephropathy: the role of clinical and histological prognostic factors. Am J Kidney Dis. 2002. 36:227–237.
4. Yoshikawa N, Tanaka R, Iijima K. Pathophysiology and treatment of IgA nephropathy in children. Pediatr Nephrol. 2001. 16:446–457.

5. Klein M, Radhakrishnan J, Appel G. Cyclosporine treatment of glomerular diseases. Annu Rev Med. 1999. 50:1–15.
6. Lai KN, Lai FM, Li PK, Vallance-Owen J. Cyclosporin treatment of IgA nephropathy: a short term controlled trial. Br Med J. 1987. 295:1165–1168.

7. Chabova V, Tesar V, Zabka J, Rychlik I, Merta M, Jirsa M Jr, Stejskalová A. Long-term treatment of IgA nephropathy with cyclosporin A--a preliminary report. Nephrol Dial Transplant. 1997. 12:2206–2207.

8. Kim PK, Kim KS, Pai KS, Kim JH, Choi IJ. Long-term results of cyclosporine-induced remission of relapsing nephrotic syndrome in children. Yonsei Med J. 1997. 38:307–318.

9. Haas M. Histologic subclassification of IgA nephropathy: a clinicopathologic study of 244 cases. Am J Kidney Dis. 1997. 29:829–842.

10. Andreoli SP, Bergstein JM. Treatment of severe IgA nephropathy in children. Pediatr Nephrol. 1989. 3:248–253.

11. Foster BJ, Bernard C, Drummond KN, Sharma AK. Effective therapy for severe Henoch-Schönlein purpura nephritis with prednisone and azathioprine: a clinical and histopathologic study. J Pediatr. 2000. 136:370–375.
12. Meadow SR, Glasgow EF, White RHR, Moncrief MW, Cameron JS, Ogg CS. Schünlein-Henoch nephritis. Q J Med. 1972. 41:241–258.
14. Goumenos DS, Brown CB. Therapeutic approach of patients with IgA nephropathy. Ren Fail. 2004. 26:171–177.

15. Chan JC, Trachtman H. Modulating the progression in IgA nephropathy. Nephron Clin Pract. 2006. 104:c61–c68.

16. Meyrier A. Ciclosporin in the treatment of nephrosis. Minimal change disease and focal-segmental glomerulosclerosis. Am J Nephrol. 1989. 9:Suppl 1. 65–71.
17. Maruyama K, Tomizawa S, Seki Y, Arai H, Kuroume T. Inhibition of vascular permeability factor production by ciclosporin in minimal change nephrotic syndrome. Nephron. 1992. 62:27–30.

18. Zietse R, Wenting GJ, Kramer P, Schalekamp MA, Weimar W. Effects of cyclosporin A on glomerular barrier function in the nephrotic syndrome. Clin Sci (Lond). 1992. 82:641–650.

19. Chung WY, Lim IS, Lee SY, Lee SK. Immunologic and morphologic study of experimental IgA nephropathy in ddY mice after administration of cyclosporin A (CyA) (Abstract). Kidney Int. 1992. 41:1952–1953.
20. Allen AC, Layward L, Harper SJ, Feehally J. In vitro immunoglobulin isotype suppression in immunoglobulin A nephropathy. Exp Nephrol. 1994. 2:166–170.
21. Lv J, Zhang H, Chen Y, Li G, Jiang L, Singh AK, Wang H. Combination therapy of prednisone and ACE inhibitor versus ACE-inhibitor therapy alone in patients with IgA nephropathy: a randomized controlled trial. Am J Kidney Dis. 2009. 53:5–8.

22. Yoshikawa N, Honda M, Iijima K, Awazu M, Hattori S, Nakanishi K, Ito H. Japanese Pediatric IgA Nephropathy Treatment Study Group. Steroid treatment for severe childhood IgA nephropathy: a randomized, controlled trial. Clin J Am Soc Nephrol. 2006. 1:511–517.

23. Coppo R, Peruzzi L, Amore A, Piccoli A, Cochat P, Stone R, Kirschstein M, Linné T. IgACE: a placebo-controlled, randomized trial of angiotensin-converting enzyme inhibitors in children and young people with IgA nephropathy and moderate proteinuria. J Am Soc Nephrol. 2007. 18:1880–1888.

24. Tikkanen I, Johnston CI. Comparison of renin-angiotensin to calcium channel blockade in renal disease. Kidney Int Suppl. 1997. 63:Suppl. S19–S22.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download