Abstract
Maze operation could alter P wave morphology in electrocardiogram (ECG), which might prevent exact diagnosis of the cardiac rhythm of patients. However, characteristics of P wave in patients with sinus rhythm after the operation have not been elucidated systematically. Consecutive patients who underwent the modified Cox Maze operation from January to December 2007 were enrolled. The standard 12-lead ECG and echocardiography were evaluated in patients who had sinus rhythm at 6 months after the operation. The average axis of P wave was 65±30 degrees. The average amplitude of P wave was less than 0.1 mV in all 12-leads, with highest amplitude in V1. The most common morphology of P wave was monophasic with positive polarity (49%), except aVR lead, which was different from those in patients with enlarged left atrium, characterized by large P-terminal force in the lead V1. There were no significant differences in P-wave characteristics and echocardiographic parameters between patients with LA activity (30.6%) versus without LA activity (69.4%) at 6 months after the operation. In conclusion, the morphology of P wave in patients after Maze operation shows loss of typical ECG pattern of P mitrale: P wave morphology is small in amplitude, monophasic and with positive polarity.
Cox Maze procedure has remained the gold standard for the surgical treatment of atrial fibrillation for almost two decades. In 1991, James Cox and associates introduced this openheart surgical approach, to block the reentrant pathways by making multiple atrial incisions and to block propagation of microreentrant wavelets (1). After multiple modifications (2, 3), Cox Maze III and more recently, Cox Maze IV operation reported success rate that ranges from 79 to 99% (4, 5). Preoperative left atrium size and duration of atrial fibrillation have been identified as two important determinants in restoring sinus rhythm (6-9).
However, much of the studies were focused on the success rate and predictors of sinus conversion and less is known about the electrocardiographic characteristics in those who maintain sinus rhythm. Maze operation divides the atria into several compartments, which are electrically isolated. Therefore this type of procedure could alter P wave morphology in the surface ECG, which might prevent exact diagnosis of the cardiac rhythm of patients. However, characteristics of P wave in these patients have not been yet elucidated systematically. This study was aimed to describe the characteristics of P wave morphology and amplitude using standard 12-lead ECG in patients with normal sinus rhythm at 6 months after the Cox Maze procedure.
Between January and December 2007, total 61 consecutive patients underwent the Modified Cox Maze III or IV operation at Seoul National University Hospital. All patients were in atrial fibrillation at least 3 months before the operation. The standard 12-lead surface ECG and 2-dimensional transthoracic echocardiography were performed at 6 months after the operation. Six-month ECG was not available in 7 patients and 18 patients did not show normal sinus rhythm on the 6-month ECG. Therefore total 36 patients were included to evaluate the P wave.
In Cox Maze III operation, specific 'maze' of incisions is made along both atria by 'cut and sew' technique, and left atrium appendage is excised. The Cox Maze IV operation is rather simplified by replacing many of the traditional cut and sew lesions with linear lines of ablation by using a bipolar radiofrequency energy device. The Cox Maze IV operation isolates right and left pulmonary veins as two islands, preserves right atrial appendage and leaves most of the left atrium in electrical continuity with remainder of the atrium.
All electrocardiograms were reviewed by two independent electrocardiographers. Amplitude and duration of P waves of all 12 leads were measured using an electronic caliper in each patient. Numerical values are expressed as mean, standard deviation. Statistical significance was determined by using twotailed Student's t test. Paired sample t-test was used to compare the preoperative and postoperative echocardiographic parameters. A P value of less than 0.05 was considered to be significant.
The average age of the patients was 54.2±10.3 yr old. Fourteen patients (38.9%) were males and the mean heart rate was 78±13 beats per minute. Twenty patients (55.6%) were on amiodarone therapy at 6 months. Twenty patients had undergone the modified Cox Maze III operation and 16 patients had the modified Cox Maze IV operation. Twenty-three patients had been diagnosed as mitral stenosis and all patients had undergone concomitant cardiac procedures, most of which was mitral valve replacement (33/36, 91.7%, Table 1). The preoperative and postoperative left atrium (LA) diameters were 56.5±7.6 mm and 48.3±6.5 mm, respectively. The preoperative left ventricle ejection fraction was 54.5±9.7%.
All the medications of the patients were reviewed, which included digoxin, amiodarone, beta blockers, calcium channel blockers, ACE inhibitors and ARBs. Neither medications nor type of the operation affect characteristics of P wave on ECG.
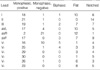
On surface ECG at 6 months after the operation, the patients with sinus rhythm showed average P-wave axis of 65±30 degrees. None of the recruited patients showed sinus node dysfunction including severe sinus bradycardia, sinus pauses, or atrial tachyarrhythmias. The average amplitude of P wave was less than 0.1 mV in all 12-leads, with highest amplitude in V1, which was 0.07±0.03 mV (Table 2). Fig. 1 shows the typical ECG found in our patients after Maze operation. The morphology of P wave were mostly monophasic with positive polarity (49%), except the lead aVR which appeared monophasic with negative polarity. Table 3 shows frequency of different morphologies in ECG after Cox Maze procedure, according to each leads. P mitrale or large negative P terminal force in lead V1, which are commonly accepted as typical ECG of left atrial enlargement, were not found in our patients.
Among 36 patients, 30.6% of patients showed mechanical activity of the LA on 6-month echocardiography. When we compared the patients with LA activity versus those without LA activity, there were no significant differences in characteristics of P wave and echocardiographic parameters (Table 4). Also, the morphology of P wave did not show significant difference when two types of Maze operation were compared.
In this study, the morphology of P wave was different from what is usually seen in LA enlargement, which is characterized by wide and notched P wave, so called P mitrale, in the leads I and II and large P-terminal force in V1. The most common morphology of P wave in our study was different from these, despite enlarged LA. After the modified Cox Maze procedure, most of the LA, especially posterior wall and appendage, become electrically isolated. These regions are mainly responsible for notched wide P wave in I and II and large P-terminal force in V1. Therefore this could explain the different morphology of P wave in our study. Our result was somewhat similar to a previous study by Lo et al. (10). They studied P wave morphology of patients undergoing atrial compartment operation for chronic atrial fibrillation, and found that 93% of patients showed altered P wave, which was small with average amplitude of 1.0±0.3 mm, and increased negative terminal force was not seen in V1. Study of Lo et al. differed from our study in the aspects that their surgical management was not the Cox Maze operation and the number of enrolled patient was smaller (n=15) than that of our study. They showed terminal negative deflection in inferior leads which corresponds to the right atrial appendage activation. This finding was not seen in our patients because the right atrial appendage as well as the left appendage is isolated or obliterated in the Cox Maze operation. Therefore the results of the present study would be the first systematical evaluation of P wave morphology in patients with successful outcome of the modified Cox Maze operation.
Our study showed that P waves in ECG of these patients were very small with amplitude less than 0.1 mV, as a result of the Cox Maze procedure. The maze circuit lengthens the period of atrial depolarization which leads to small or even absent P waves and make it hard to identify P waves in a standard 12 lead ECG. The difficulty in identifying the P wave may also be due to the low gain of the standard 12-lead ECG, which can be overcome by amplifying the gain and frequency of the ECG. Pasic et al. (11) reported that adding right precordial leads from V3R through V6R to the standard 12-lead surface ECG can improve detection of P waves and identification of atrial electrical activity. They studied 30 patients after combined Cox-Maze III procedure and mitral valve surgery, and reported right precordial ECG, especially V4R, is a helpful tool for visualization P waves.
Our data showed 30.6% of patients with recovered LA activity at 6 months after the Maze operation. The low rate of LA activity may be due to delayed recovery of atrial function after the atrial compartment operation, which has been reported from earlier studies (12, 13). This "period of left atrial paralysis" may have contributed to the low rate of atrial activity in our patients.
The limitations in our study are as follows. First, this is a single-center study and the number of patients enrolled in the present study was not large. However, we think that the data would be representative enough to observe the ECG characteristics of the patients after Cox Maze operation because the patients were consecutively enrolled and the same design of suture or cryoablation line was applied to all patients.
Second, none of the enrolled patients underwent electrophysiological study, which might be the most accurate method to identify the patient's rhythm. In our series of 61 patients, 18 were not recognized as sinus rhythm electrocardiographically. Small portion of these 18 patients might have sinus rhythm with very small amplitude of P waves, thus their ECG diagnoses were considered as non-sinus rhythm such as junctional rhythm. However the effects on the overall data might be minimal.
In conclusion, the morphology of P wave in patients after Maze operation showed loss of typical ECG pattern of P mitrale. The characteristics of P wave morphology after Maze operation was small in amplitude, monophasic and with positive polarity.
Figures and Tables
References
1. Cox JL, Schuessler RB, D'Agostino HJ Jr, Stone CM, Chang BC, Cain ME, Corr PB, Boineau JP. The surgical treatment of atrial fibrillation. III. Development of a definitive surgical procedure. J Thorac Cardiovasc Surg. 1991. 101:569–583.
2. Cox JL, Jaquiss RD, Schuessler RB, Boineau JP. Modification of the maze procedure for atrial flutter and atrial fibrillation. II. Surgical technique of the maze III procedure. J Thorac Cardiovasc Surg. 1995. 110:485–495.
3. Cox JL, Schuessler RB, Boineau JP. The development of the Maze procedure for the treatment of atrial fibrillation. Semin Thorac Cardiovasc Surg. 2000. 12:2–14.

4. Stulak JM, Sundt TM 3rd, Dearani JA, Daly RC, Orsulak TA, Schaff HV. Ten-year experience with the Cox-maze procedure for atrial fibrillation: how do we define success? Ann Thorac Surg. 2007. 83:1319–1324.

5. Cox JL, Ad N, Palazzo T, Fitzpatrick S, Suyderhoud JP, DeGroot KW, Pirovic EA, Lou HC, Duvall WZ, Kim YD. Current status of the Maze procedure for the treatment of atrial fibrillation. Semin Thorac Cardiovasc Surg. 2000. 12:15–19.

6. Chen MC, Chang JP, Chang HW, Chen CJ, Yang CH, Chen YH, Fu M. Clinical determinants of sinus conversion by radiofrequency maze procedure for persistent atrial fibrillation in patients undergoing concomitant mitral valvular surgery. Am J Cardiol. 2005. 96:1553–1557.

7. Ueshima K, Hashimoto K, Chiba M, Nakamura M, Nasu M, Hiramori K, Kamata J, Yagi Y, Kawazoe K. What are the predictors of restoration of sinus rhythm after combined treatment with surgical repair for organic heart disease and the Maze procedure for atrial fibrillation? J Cardiovasc Surg (Torino). 1999. 40:793–796.
8. Kim YH, Lee SC, Oh HL, IL R, Lee SH, Hong KP, Park PW, Park JE, Seo JD. Predictors of sinus rhythm restoration after Maze operation and relationship between pre- and post-operative left atrial volume. Korean Circ J. 2004. 34:574–581.

9. Song BG, Cho SJ, Lee SY, Kim JH, Choi SM, Park YH, Choi JO, Lee SC, On YK, Park SW, Kim JS, Park P. Atrial mechanical function after Maze procedure for atrial fibrillation concomitant with mitral valve surgery. Korean Circ J. 2008. 38:606–611.

10. Lo HM, Lin JL, Lin FY, Tseng YZ. Characteristic P wave morphology in patients undergoing the atrial compartment operation for chronic atrial fibrillation with mitral valve disease. Pacing Clin Electrophysiol. 2003. 26:1864–1872.

11. Pasic M, Musci M, Edelmann B, Siniawski H, Bergs P, Hetzer R. Identification of P waves after the Cox-maze procedure: significance of right precordial leads V3R through V6R. Ann Thorac Surg. 1999. 67:1292–1294.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download