Abstract
The efficacy of tandem high-dose chemotherapy and autologous stem cell rescue (HDCT/ASCR) was investigated in patients with high-risk neuroblastoma. Patients over 1 yr of age who were newly diagnosed with stage 4 neuroblastoma from January 2000 to December 2005 were enrolled in The Korean Society of Pediatric Hematology-Oncology registry. All patients who were assigned to receive HDCT/ASCR at diagnosis were retrospectively analyzed to investigate the efficacy of single or tandem HDCT/ASCR. Seventy and 71 patients were assigned to receive single or tandem HDCT/ASCR at diagnosis. Fifty-seven and 59 patients in the single or tandem HDCT group underwent single or tandem HDCT/ASCR as scheduled. Twenty-four and 38 patients in the single or tandem HDCT group remained event free with a median follow-up of 56 (24-88) months. When the survival rate was analyzed according to intent-to-treat at diagnosis, the probability of the 5-yr event-free survival±95% confidence intervals was higher in the tandem HDCT group than in the single HDCT group (51.2±12.4% vs. 31.3±11.5%, P=0.030). The results of the present study demonstrate that the tandem HDCT/ASCR strategy is significantly better than the single HDCT/ASCR strategy for improved survival in the treatment of high-risk neuroblastoma patients.
The prognosis of high-risk neuroblastoma after conventional chemotherapy is generally poor (1-3). Therefore, a strategy using high-dose chemotherapy and autologous stem cell rescue (HDCT/ASCR) has been explored to improve the prognosis of patients with high-risk neuroblastoma (2-5). This strategy is based on the hypothesis that dose escalation might improve the survival of children with high-risk neuroblastoma. The results of randomized trials comparing HDCT/ASCR with chemotherapy alone showed a better event-free survival (EFS) in the HDCT/ASCR arm than in the continuous chemotherapy arm (3, 6). However, the overall EFS was unsatisfactory.
In this context, a few studies have examined the efficacy of double or triple tandem HDCT/ASCR procedures to further improve the outcome of high-risk neuroblastoma patients (7-9). George et al. (7) and Sung et al. (8) carried out a single arm trial of tandem HDCT/ASCR as consolidation therapy and reported improved long-term survival with acceptable toxicity. Kletzel et al. (9) also conducted a single arm trial of triple tandem HDCT/ASCR and reported improved survival. These studies demonstrated that further dose escalation might result in additional improvements in the EFS of high-risk neuroblastoma patients. However, there is no study that has compared the efficacy of single and tandem HDCT/ASCR for the treatment of high-risk neuroblastoma. Therefore, the present study retrospectively compared the efficacy of single and tandem HDCT/ASCR and showed that the tandem HDCT/ASCR strategy might be better than the single HDCT/ASCR strategy in terms of the EFS in patients with high-risk neuroblastoma.
From January 2000 to December 2005, patients with newly diagnosed stage 4 neuroblastoma over 1 yr of age at diagnosis were enrolled in the Korean Society of Pediatric Hematology-Oncology (KSPHO) registry. In the present study, the patients who were assigned to receive single or tandem HDCT/ASCR at diagnosis, as consolidation therapy after induction therapy, were analyzed to investigate the efficacy of tandem HDCT/ASCR compared to single HDCT/ASCR. Patients who were assigned to receive HDCT/ASCR after relapse or progression were excluded from this analysis. Samsung Medical Center Institutional Review Board approved the present study (2008-07-002).
The diagnosis of neuroblastoma was made based on either histological examination of tumor specimens or bone marrow infiltration with neuroblastoma cells and elevated urine catecholamine levels. The extent of the disease was evaluated using computerized tomography, a technetium-99 (99Tc) bone scan, bilateral bone marrow aspirates and biopsy specimens, and an iodine-131 or 123-metaiodobenzylguanidine scan; the patients were staged according to the international neuroblastoma staging system (INSS) (10). However, the N-myc copy number and tumor karyotype were not routinely evaluated.
A variety of chemotherapy regimens were employed for induction treatment (Table 1). Definitive surgery was usually performed after 3-6 cycles of preoperative chemotherapy, except for those patients who had surgical resection of their primary tumor before the administration of induction chemotherapy. After surgery, 1-5 cycles of postoperative chemotherapy was given prior to HDCT/ASCR. Radiotherapy was given to patients with gross residual tumor after surgery. However, in a few centers, radiotherapy was given to all patients regardless of the resectability of the tumor. The timing of radiotherapy was after surgery or after HDCT/ASCR. Peripheral blood stem cells were usually collected during the recovery phase after chemotherapy following surgery.
After the completion of induction therapy, the patients underwent single or tandem HDCT/ASCR as consolidation treatment according to the assignment at diagnosis. Patients with tumor progression prior to HDCT/ASCR received salvage treatment and patients whose parents refused to proceed to HDCT/ASCR for fear of toxicity and death were treated with conventional chemotherapy alone. A variety of HDCT regimens were employed (Table 1). In the tandem group, a second HDCT/ASCR was usually given if the platelet count exceeded 50×109/L after the first HDCT/ASCR without a transfusion requirement and with no evidence of significant organ dysfunction. Approximately half of the collected stem cells were infused for marrow rescue at each HDCT session.
Patients who underwent HDCT/ASCR received 13-cis-retinoic acid for the possible minimal residual tumor cells. Differentiation therapy with 13-cis-retinoic acid was usually initiated 60-90 days after the last HDCT/ASCR. Some patients received immunotherapy using interleukin-2 according to the physician's judgments. In some centers, local radiotherapy was given after the HDCT/ASCR.
The international response criteria were used to evaluate the treatment response (10). Briefly, complete response (CR) was defined as no identifiable tumor with normal catecholamine levels. Very good partial response (VGPR) was defined as a decrease in the primary tumor by 90-99% with normal catecholamine levels with or without any residual 99Tc bone changes. Partial response (PR) was defined as a reduction of the primary tumor and metastatic tumor by more than 50%. Stable disease (SD) and minor response (MR) were responses of less than 50%. Progressive disease (PD) indicated progression at any preexisting tumor site or appearance of a new lesion.
The survival rate along with the 95% confidence interval (CI) was estimated using the Kaplan-Meier method. An event was defined as the occurrence of a relapse, progression or treatment-related mortality (TRM). The differences in the survival rates between the two groups were compared using the logrank test. The differences in the frequencies of the clinical and biological factors between the two groups were compared using the Pearson chi-square test. The differences in the levels of tumor markers were compared using the Mann-Whitney U test. The differences in the ANC and platelet recovery between the first and second HDCT/ASCR were analyzed using a paired t-test. Multivariate analyses including the prognostic factors at diagnosis for EFS were performed using the Cox regression analysis. P values <0.05 were considered significant.
From January 2000 to December 2005, a total of 161 patients over 1 yr of age at diagnosis with newly diagnosed stage 4 neuroblastoma were enrolled in the KSPHO registry by 24 hospitals. A total of 141 out of 161 patients enrolled in the KSPHO registry by 20 hospitals were assigned at diagnosis to receive single or tandem HDCT/ASCR (70 and 71 patients, respectively) as consolidation therapy after induction therapy. While some hospitals adopted one of the two (single or tandem, 6 and 8 hospitals, respectively) strategies, 6 hospitals adopted both strategies according to the status of patients at diagnosis or the study period. Table 2 lists the clinical and biological characteristics of the patients. Although a higher proportion of patients had bone metastasis in the tandem group compared to the single group, no other significant differences were observed for a variety of clinical and biological characteristics between the single and tandem group.
The CEDC regimen was most commonly used in both the single and tandem groups (Table 1). Gross total removal was possible in about half of the patients (51.7% and 47.9% in single and tandem group, respectively, P=NS). Local radiotherapy was given to a greater proportion of patients in the tandem group than in the single group (74.6% and 54.3% in single and tandem group, respectively, P=0.012). A similar proportion of patients in both groups were in the CR or VGPR categories prior to the HDCT/ASCR (73.7% and 74.6%, in single and tandem group, respectively, P=NS). Fig. 1 shows the flow of patients from diagnosis through the tandem HDCT/ASCR. During induction treatment, 6 progressions, 1 TRM and 1 renal insufficiency occurred, and the parents of 5 patients refused to proceed to the scheduled HDCT/ASCR in the single group. In the tandem group, 3 progressions occurred prior to HDCT/ASCR and the parents of 2 patients refused to proceed to the scheduled HDCT/ASCR.
Fifty-seven (81.4%) out of 70 patients in the single group proceeded to the HDCT/ASCR as assigned at diagnosis. Four of them received a second HDCT because the tumor progressed after the first HDCT (n=3) or the patients were not in CR (n=1). In the tandem group, 66 (93.0%) out of 71 patients proceeded to the first HDCT/ASCR as assigned at diagnosis, however, 7 of them could not proceed to the second HDCT/ASCR due to tumor progression after first HDCT (n=1), TRM during the first HDCT (n=2), refusal by parents (n=3) and an insufficient number of stem cells for rescue in the second HDCT (n=1). Therefore, 59 (83.1%) out of 71 patients in the tandem group received the tandem HDCT/ASCR as assigned at diagnosis. Interim conventional chemotherapy was given between the first and second HDCT in 6 patients because they were in PR after the first HDCT. A total of 123 patients underwent at least one HDCT/ASCR and 63 patients underwent tandem HDCT/ASCR.
The CEM regimen in the single group and the CEC regimen in the tandem group were most commonly used for the first HDCT (Table 1). TM-TBI and BM regimens were most frequently used for the second HDCT. Total body irradiation (TBI) was included in the HDCT regimen in a significantly higher proportion of patients in the tandem group than in the single group (63.6% vs. 29.8%, P<0.001). In the tandem group, the TBI was administered as a part of the HDCT/ASCR in 38 (15 in the first and 23 in the second HDCT) out of 59 patients who completed the tandem HDCT/ASCR, but not in the remaining 21 patients. In the tandem HDCT/ASCR, the median interval from the first infusion of stem cells to the initiation of the second HDCT was 90 days (range 43-261) and the interval was less than 120 days in 81.4% of the patients. When the patients who received interim chemotherapy between the first and second HDCT were excluded from the analyses, the median interval was 86 days (range 43-173) and the interval was less than 120 days in 90.6% of the patients.
A median of 3.5×106 CD34+ cells/kg (range 0.6-48.5) were infused for the first HDCT/ASCR, and the median time required to reach an ANC of 0.5×109/L and a platelet count of 20×109/L, without transfusion over the previous 7 days, was 11 days (range 8-52) and 23 days (range 10-362), respectively. A median of 2.9×106 CD34+ cells/kg (range 0.2-42.5) were infused for the second HDCT/ASCR and the median time required to reach an ANC of 0.5×109/L and a platelet count of 20×109/L was 11 days (range 8-27) and 34 days (range 17-417), respectively. When the analysis was confined to only those patients who received tandem transplantation, the platelet recovery was significantly delayed after the second transplantation compared to the first (median 23 days versus 34 days, P=0.003).
A total of 11 (8.9%) TRMs (9 in single group and 2 in tandem group) were noted during the first HDCT/ASCR and were attributed to viral pneumonia (n=4), pulmonary hemorrhage (n=3), sepsis (n=2), hepatic veno-occlusive disease (VOD) (n=1), and an unknown cause (n=1). A total of 6 (9.5%) TRMs were noted during the second HDCT/ASCR and were attributed to VOD (n=3), myocarditis (n=1), acute renal failure (n=1), and sepsis (n=1). Five of the 6 TRMs during the second HDCT occurred in patients who received TBI. While all 5 TRMs occurred in 15 patients who received TBI during the first HDCT, there was no TRM among the 23 patients who received TBI during the second HDCT (P=0.006). Thyroid cancer developed in one patient in the tandem group; however, this patient received only the first HDCT/ASCR and did not proceed to the second HDCT/ASCR due to parental fear of toxicity and death. Otherwise, there were no other secondary malignancies observed in the present study.
The median follow-up duration of all living patients was 56 months (range 24-88) from diagnosis. The tumor relapsed or progressed in 36 out of 70 patients and 10 TRMs occurred in the single group. The remaining 24 patients remained event free with a median follow-up of 68 months (range 24-85) from diagnosis. For the tandem group, the tumor relapsed or progressed in 25 out of 71 patients and 8 TRMs occurred. The remaining 38 patients remained event free with a median follow-up of 41 months (range 28-88) from diagnosis. When the survival rate was analyzed according to intent-to-treat at diagnosis, the probability of 5-yr EFS after diagnosis was higher in the tandem group than in the single group (51.2%±12.4% vs. 31.3%±11.5%, P=0.030, Fig. 2A). When the analysis was confined to the 123 patients who proceeded to HDCT/ASCR as assigned at diagnosis (57 single and 66 tandem), the probability of 5-yr RFS after the first HDCT was higher in the tandem group than in the single group with borderline significance (59.1%±13.5% vs.41.6%±14.5%, P=0.099, Fig. 2B). However, the difference became significant when the analysis was confined to only patients who were not in CR prior to the first HDCT (55.7%±17.0% vs. 0%, P=0.012, Fig. 2C). The probability of RFS after the tandem HDCT was significantly higher in the TBI group than in non-TBI group (70.5%±16.6% vs. 47.4%±23.1%, P=0.049) although the TRM rate was slightly higher in the TBI group than in the non-TBI group (5/38 vs. 1/21, P=NS). Multivariate analyses including the prognostic factors at diagnosis for EFS revealed that tandem HDCT /ASCR treatment was the only independent favorable prognostic factor associated with the EFS (hazard ratio 0.16, 95% confidence interval 0.03-0.91, P=0.039; Table 3).
Although the strategy of using HDCT/ASCR has improved the survival of patients with high-risk neuroblastoma, the survival rate after a single HDCT/ASCR has been unsatisfactory (2-5). Therefore, investigators have examined the efficacy of tandem HDCT/ASCR to further improve the outcome of high-risk neuroblastoma patients, and have shown that tandem HDCT/ASCR is a feasible approach which might result in further improvements in the survival of high-risk neuroblastoma patients (7-9). However, no study has compared the efficacy of single with tandem HDCT/ASCR for the treatment of high-risk neuroblastoma. Therefore, the present study retrospectively compared the efficacy of single and tandem HDCT/ASCR. The results showed that the tandem HDCT/ASCR strategy is significantly better than single HDCT/ASCR strategy for improved survival of patients with high-risk neuroblastoma. The survival rate in the tandem group, in the present study, was similar to other prior studies that have reported on the tandem double and tandem triple HDCT/ASCR strategies (7-9).
In the present study, the number of cases with tumor progression prior to the first HDCT/ASCR, and the number of TRM during the first HDCT were higher in the single group than in the tandem group. These findings suggest that the quality of medical treatment might not have been the same for the single and tandem groups. These findings might have affected the outcome of the patients (worse EFS in the single group) and create doubt as to whether the tandem HDCT/ASCR itself resulted in a better outcome compared to the single HDCT/ASCR in the present study. However, when the analysis was confined to the patients that successfully preceded to HDCT/ASCR, as assigned at diagnosis, the probability of the 5-yr RFS, after the first HDCT, was still higher in the tandem group than in the single group, particularly in the patients who were not in CR prior to the first HDCT. Taken together, these findings suggest that the tandem HDC T/ASCR strategy can provide better outcomes in patients with high-risk neuroblastoma than single HDCT/ASCR strategy.
While neutrophil recovery after the second HDCT/ASCR was as rapid as after the first HDCT/ASCR, the platelet recovery was significantly delayed after the second HDCT/ASCR compared to the first HDCT/ASCR. However, this was not clinically significant. A total of 6 TRMs were noted during the second HDCT/ASCR in the tandem group. However, this TRM rate might be acceptable considering that the tumor relapsed in 19 patients even after the tandem HDCT/ASCR. Taken together, these findings suggest that the tandem HD CT/ASCR strategy can provide better outcomes than single HDCT/ASCR strategy despite the additional toxicity risks during the second HDCT/ASCR.
TBI was administered as a part of the HDCT/ASCR in 38 out of 59 patients who completed the tandem HDCT, but not in the remaining 21 patients. The probability of RFS after the tandem HDCT was significantly higher in the TBI group compared to the non-TBI group, although the TRM rate during the second HDCT/ASCR was slightly higher in the TBI group than in the non-TBI group. Of note is that there was no TRM during the second HDCT in the patients who received TBI during the second HDCT. All TRMs during the second HDCT in the TBI group occurred in patients who received TBI during the first HDCT. These findings are consistent with the findings in the report by Sung et al (8). They reported that TBI during the first HDCT/ASCR was significantly associated with a higher TRM rate in the second HDCT; they recommended that TBI should be included in the second HDCT/ASCR if TBI is to be included in the tandem HDCT regimen. Taken together, administration of TBI was associated with a higher RFS despite the high TRM rate, and TBI might improve the EFS if TBI is included in the second HDCT/ASCR.
Intensive tandem HDCT/ASCR and radiation therapy (particularly TBI) may improve the survival of patients with high-risk neuroblastoma, but may also increase the frequency and severity of long-term side effects such as a secondary malignancy (11-13). Although no secondary malignancy developed in the patients who completed the tandem HDCT/ASCR, a longer follow-up will be needed to consider this possibility. The optimal combination of regimens for the tandem HDCT has yet to be determined. Further study will be needed to reduce the TRM rate during the second HDCT/ASCR as well as the long-term side effects whilst maintaining or reducing the relapse rate after intensive tandem HDCT/ASCR.
In summary, the results of the present retrospective study demonstrated that the tandem HDCT/ASCR strategy is significantly better than the single HDCT/ASCR strategy in terms of survival for the treatment of patients with high-risk neuroblastoma, particularly when the patient is not in CR prior to the HDCT/ASCR. A randomized prospective study will be needed in the future to explore the safety and efficacy of tandem HDCT/ASCR compared to single HDCT/ASCR, and to confirm our findings.
Figures and Tables
Fig. 1
Flow of patients. Fifty-seven (81.4%) out of 70 patients in the single group proceeded to the HDCT/ASCR as assigned at diagnosis. In the tandem group, 66 (93.0%) out of 71 patients proceeded to the first HDCT/ASCR and 59 (83.1%) patients received the second HDCT/ASCR as assigned at diagnosis.

Fig. 2
Results of the Kaplan-Meier analysis. (A) When the survival rate was analyzed according to intent-to-treat at diagnosis, the probability of the 5-yr EFS after diagnosis was higher in the tandem group than in the single group (51.2±12.4% vs. 31.3±11.5%, P=0.030). (B) When the analysis was confined to 123 patients who proceeded to HDCT/ASCR as assigned at diagnosis, the probability of 5-yr RFS after the first HDCT was higher in the tandem group than in the single group with borderline significance (59.7±13.5% vs. 41.6±14.5%, P=0.099). (C) However, the difference became significant when the analysis was confined to only patients who were not in CR prior to the first HDCT (55.7±17.0% vs. 0%, P=0.012).

Table 1
Induction chemotherapy and HDCT regimens
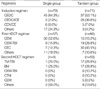
HDCT, high-dose chemotherapy; CEDC, cisplatinum+etoposide+doxorubicin+cyclophosphamide; ICE, ifosfamide+carboplatin+etoposide; CDV, cyclophosphamide+doxorubicin+vincristine; CE, cisplatinum+etoposide; CEM, carboplatin+etoposide+melphalan; TBI, total body irradiation; BM, busulfan+melphalan; CTM, carboplatin+thiotepa+melphalan.
ACKNOWLEDGMENTS
List of contributors: Investigators listed as follow participated in the present study. Eun Jin Choi (Daegu Catholic University Medical Center, Daegu, Korea), Jeong Ok Hah (College of Medicine, Yeungnam University, Daegu, Korea), Pyoung Han Hwang (Chonbuk National University, Jeonju, Korea), In Sang Jeon (Gil Medical Center, Incheon, Korea), Heung Sik Kim (Keimyung University, School of Medicine, Daegu, Korea), Soon Ki Kim (College of Medicine, Inha University, Inchon, Korea), Sun Young Kim (Chungnam National University Hospital, Daejeon, Korea), Jun Ah Lee (Korea Cancer Center Hospital, Seoul, Korea), Kwang Chul Lee (College of Medicine, Korea University, Seoul, Korea), Mee Jeong Lee (Dankook University Hospital, Cheonan, Korea), Young-Ho Lee (Hanyang University Medical Center, Seoul, Korea), Jae Young Lim (Gyeongsang National University Hospital, Jinju, Korea), Young Tak Lim (College of Medicine, Pusan National University, Pusan, Korea), Jun Eun Park (Ajou University School of Medicine, Suwon, Korea), Hyeon Jin Park (National Cancer Center, Ilsan, Korea), Kyung-Ha Ryu (Ewha Womans' University College of Medicine, Seoul, Korea), Eun Sun Yoo (Ewha Womans' University College of Medicine, Seoul, Korea)
References
1. Frappaz D, Michon J, Coze C, Berger C, Plouvier E, Lasset C, Bernard JL, Stephan JL, Bouffet E, Buclon M, Combaret V, Fourquet A, Philip T, Zucker JM. LMCE3 treatment strategy: results in 99 consecutively diagnosed stage 4 neuroblastomas in children older than 1 year at diagnosis. J Clin Oncol. 2000. 18:468–476.

2. Stram DO, Matthay KK, O'Leary M, Reynolds CP, Haase GM, Atkinson JB, Brodeur GM, Seeger RC. Consolidation chemoradiotherapy and autologous bone marrow transplantation versus continued chemotherapy for metastatic neuroblastoma: a report of two concurrent Children's Cancer Group studies. J Clin Oncol. 1996. 14:2417–2426.

3. Matthay KK, Villablanca JG, Seeger RC, Stram DO, Harris RE, Ramsay NK, Swift P, Shimada H, Black CT, Brodeur GM, Gerbing RB, Reynolds CP. Children's Cancer Group. Treatment of high-risk neuroblastoma with intensive chemotherapy, radiotherapy, autologous bone marrow transplantation, and 13-cis-retinoic acid. N Engl J Med. 1999. 341:1165–1173.

4. Ladenstein R, Philip T, Lasset C, Hartmann O, Garaventa A, Pinkerton R, Michon J, Prichard J, Klingebiel T, Kremens B, Pearson A, Coze C, Paolucci P, Frappaz D, Gadner H, Chauvin F. Multivariate analysis of risk factors in stage 4 neuroblastoma patients over the age of one year treated with megatherapy and stem-cell transplantation: a report from the European Bone Marrow Transplantation Solid Tumor Registry. J Clin Oncol. 1998. 16:953–965.

5. Cohn SL, Moss TJ, Hoover M, Katzenstein HM, Haut PR, Morgan ER, Green AA, Kletzel M. Treatment of poor-risk neuroblastoma patients with high-dose chemotherapy and autologous peripheral stem cell rescue. Bone Marrow Transplant. 1997. 20:543–551.

6. Berthold F, Boos J, Burdach S, Erttmann R, Henze G, Hermann J, Klingebiel T, Kremens B, Schilling FH, Schrappe M, Simon T, Hero B. Myeloablative megatherapy with autologous stem-cell rescue versus oral maintenance chemotherapy as consolidation treatment in patients with high-risk neuroblastoma: a randomized controlled trial. Lancet Oncol. 2005. 6:649–658.
7. George RE, Li S, Medeiros-Nancarrow C, Neuberg D, Marcus K, Shamberger RC, Pulsipher M, Grupp SA, Diller L. High-risk neuroblastoma treated with tandem autologous peripheral-blood stem cell-supported transplantation: long-term survival update. J Clin Oncol. 2006. 24:2891–2896.

8. Sung KW, Lee SH, Yoo KH, Jung HL, Cho EJ, Koo HH, Lee SK, Kim J, Lim DH, Suh YL, Kim DW. Tandem high-dose chemotherapy and autologous stem cell rescue in patients over 1 year of age with stage 4 neuroblastoma. Bone Marrow Transplant. 2007. 40:37–45.

9. Kletzel M, Katzenstein HM, Haut PR, Yu AL, Morgan E, Reynolds M, Geissler G, Marymount MH, Liu D, Kalapurakal JA, Shore RM, Bardo DM, Schmoldt J, Rademaker AW, Cohn SL. Treatment of high-risk neuroblastoma with triple-tandem high-dose therapy and stem-cell rescue: results of the Chicago Pilot II Study. J Clin Oncol. 2002. 20:2284–2292.

10. Brodeur GM, Pritchard J, Berthold F, Carlsen NL, Castel V, Castelberry RP, De Bernardi B, Evans AE, Favrot M, Hedborg F. Revisions of the international criteria for neuroblastoma diagnosis, staging, and response to treatment. J Clin Oncol. 1993. 11:1466–1477.

11. Flandin I, Hartmann O, Michon J, Pinkerton R, Coze C, Stephan JL, Fourquet B, Valteau-Couanet D, Bergeron C, Philip T, Carrie C. Impact of TBI on late effects in children treated by megatherapy for Stage IV neuroblastoma. A study of the French Society of Pediatric oncology. Int J Radiat Oncol Biol Phys. 2006. 64:1424–1431.

12. Meacham LR, Gurney JG, Mertens AC, Ness KK, Sklar CA, Robison LL, Oeffinger KC. Body mass index in long-term adult survivors of childhood cancer: a report of the Childhood Cancer Survivor Study. Cancer. 2005. 103:1730–1739.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download