Abstract
We describe a girl with Diamond-Blackfan anemia with accompanying red cell enolase deficiency. At the age of 9 yr old, the patient received allogeneic bone marrow transplantation from her HLA-identical sister who had normal red cell enolase activity. While the post transplant DNA analysis with short tandem repeat has continuously demonstrated a stable mixed chimerism on follow-up, the patient remains transfusion independent and continues to show a steady increase in red cell enolase activity for over two and a half years following bone marrow transplantation.
Diamond-Blackfan anemia (DBA) is a chronic congenital hematological disease characterized by a selective erythroid regenerative defect (1). The hematological features of DBA include anemia, reticulocytopenia and bone marrow erythrocytopenia, and the main stay of treatment involves corticosteroid administration and blood transfusion. Although the majority of patients respond to steroids, some require long-term high-dose steroid therapy, and some of these patients develop steroid resistance and require chronic red cell transfusions.
Red cell enolase deficiency is an enzymopathy, which has been sparsely reported. To the best of our knowledge, the association between DBA and red cell enolase deficiency has never been described in the literature. Rather, in DBA, red cell enzyme activities including enolase were reported to be above the normal mean (2). In this report, we describe a case of DBA with accompanying red cell enolase deficiency in a child, who after successful bone marrow transplantation (BMT) showed resolution of anemia as well as normalization of red cell enolase activity.
A two-month-old baby girl was diagnosed as having DBA. Her physical examination was normal except for signs of anemia, and there was no associated skeletal anomaly. At presentation, her hemoglobin was 2.7g/dL, white blood cell count 3,260/µL, platelet count 321,000/µL and reticulocytes 0.42%. A peripheral blood smear showed macrocytic normochromic anemia with no evidence of hemolysis. A bone marrow evaluation at 10 weeks of age showed a marked decrease in erythropoiesis and maturation arrest of red cell precursors (Fig. 1A). The estimated M:E ratio was 26.8:1. Serology for Parvovirus B19 or Epstein-Barr virus revealed no evidence of active infection (3). After establishing the diagnosis of DBA, the patient was treated with corticosteroid and showed good initial response. However, at 3 yr of age, she became steroid resistant and soon became transfusion dependent. She had usually been transfused every 4 to 8 weeks and required chelating treatment on a number of occasions. The anemia got progressively worsened and reticulocyte counts were low most of the time. Yet, unexplained reticulocytosis was occasionally seen (Fig. 2).
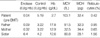
At 4 yr old, a further evaluation of her chronic anemia incidentally revealed very low enolase activity (0.04 IU/g Hb; Hb 4.0 g/dL) compared to normal control (normal control 5.19 IU/g Hb; Hb 13 g/dL) while erythrocyte adenosine deaminase level (eADA) was within normal range (1.5 IU/g Hb; normal control 1.6 IU/g Hb) (4). Other red cell enzyme activities were normal or slightly increased. Her mother and father had normal hemoglobin levels and normal mean corpuscular volume (MCV), but their enolase activities were subnormal. On the other hanad, the red cell enolase activity in her younger sister who subsequently donated marrow was normal (Table 1).
At the age of 7 yr, the patient underwent an allogeneic BMT from her human leukocyte antigen (HLA) identical sister. The conditioning regimen was comprised of intravenous busulfan 3.2 mg/kg/day over 4 days followed by intravenous cyclophosphamide 60 mg/kg/day for 2 days and rabbit antithymocyte globulin 2.5 mg/kg/day for 3 days. A total of 2.92×108/kg unmanipulated BM nucleated cells (CD34+ cells: 3.58×106/kg) were infused. Methotrexate and cyclosporine A were given to prevent graft versus host disease (GVHD). Granulocyte colony-stimulating factor at 10 g/kg/day was administrated from day 5 to day 16. Neutrophil engraftment was achieved on day 15, and platelet engraftment on day 24. No transplant related morbidity occurred, e.g., infection, acute GVHD or veno-occlusive disease. Bone marrow aspirates on day 28 showed active trilineage hematopoiesis (Fig. 1B) and mixed chimeric state (recipient DNA: 11.26%) on multiplex short tandem repeat analysis (STR) performed with the AmpFlSTR Blue polymerase chain reaction (PCR) amplification kit (PE Applied Biosystems, Foster City, CA, USA) (5). As hoped for, the enolase activity (0.72 IU/g Hb; normal control 3.4 IU/g Hb) on day 28 after BMT was higher than that of the low pre-transplant level (Fig. 3). At one year after BMT, her red cell enolase level had risen further to 6.54 IU/g Hb (normal control 7.76 IU/g Hb), and DNA analysis of the bone marrow aspirates showed a persistent stable mixed chimerism (recipient DNA 5.08%). She had no longer required any blood transfusion ever since the time of BMT.
Enolase deficiency is extremely rare, and its pathogenesis, inheritance and clinical manifestation have not been firmly established. Enolase deficiency is known to be associated with chromosome 1p locus mutations (1 pter-p36.13) and to cause chronic nonspecific hemolytic anemia (6). Lachant et al. (7) described four generations of a Caucasian family with hereditary red cell enolase deficiency. They reported that this disease entity had a variety of clinical expression with autosomal dominant inheritance pattern. However, in our case, it doesn't seem to correspond to the reported inheritance pattern.
DBA is also markedly heterogeneous with respect to pathogenesis, inheritance, and clinical manifestation. DBA is inherited in about 10-20% of cases, and genetic studies have identified mutations in RPS19 (a ribosomal protein gene) in a quarter of cases (8). Recent studies have also suggested some other associated genes, i.e., chromosomes 8p, 10q (RPS24), 1q31 and 15 (RPS17) (9-11). However, in other cases, genetic linkage with DBA has yet to be identified. This fact suggests its genetic heterogeneity. Unfortunately, genetic screening for the patient and her family was not performed at the time of diagnosis although it could have shed some light in the understanding of the relationship between enolase deficiency and DBA.
Unlike the elevated erythrocyte enzyme activities reported both in hypoplasitic anemia and stress-induced environment of erythropoiesis (2), our patient had a very low enolase level, suggesting that DBA and enolase deficiency might also coexist. On the other hand, our patient may represent a hitherto undescribed disease entity expressing both defective erythropoiesis and enolase deficiency simultaneously.
Unlike our patient described here, the eADA level is known to be generally high in DBA patients. However, the role of eADA in the pathogenesis of DBA has not been established (12).
There's a report of successful BMT in a child with a red cell pyruvate kinase (PK) deficiency (13). After transplant, the patient achieved a complete donor chimerism, normal hemoglobin level and normal red cell PK activity. On the other hand, our patient showed stable mixed chimerism. In non-malignant hematological disorders, it is believed that complete replacement of the recipient's hematopoietic system is not necessarily required to improve the underlying disease state (14). Despite the danger of graft rejection in mixed chimerism, it is known that even a small degree of mixed chimerism may improve the disease status in some hematologic diseases (15, 16). To date, there are too few case reports of HSCT therapy results in RBC enzymopathies. However, as demonstrated in our case, mixed chimerism at an 89-95% level may produce an acceptable outcome in the RBC enolase deficiency.
In summary, the case presented here uniquely illustrates that both red cell aplasia and red cell enzymopathy might coexist, and that successful marrow engrafment even with the mixed chimerism might correct both defective erythropoiesis and the RBC enolase deficiency simultaneously.
Figures and Tables
Fig. 1
(A) Bone marrow aspirates before BMT showed normocellular marrow with markedly reduced erythropoiesis. (B) Bone marrow aspirates obtained 28 days after BMT showed active trilineage hematopoiesis accompanied with presence of erythropoietic precursors (arrows).

Fig. 2
This graph displays the changes of the hemoglobin level and reticulocytes counts. While on prednisolone from 2 months to 39 months of age, the hemoglobin levels increased with transient reticulocytosis, but later gradually decreased. Since 3 yr of age, she had been intermittently transfused, usually every 4 to 8 weeks. She eventually developed transfusion dependency.

ACKNOWLEDGEMENT
We thank the nursing staffs in the Hemtopoietic Stem Cell Transplantation Unit at the National Cancer Center, without whom this publication could have not been possible, and Dr. Hee-Jin Kim for assaying the red cell enzyme levels as well as giving valuable comments regarding enolase enzymopathy.
References
1. Da Costa L, Willig TN, Fixler J, Mohandas N, Tchernia G. Diamond-Blackfan anemia. Curr Opin Pediatr. 2001. 13:10–15.
2. Wang WC, Mentzer WC. Differentiation of transient erythroblastopenia of childhood from congenital hypoplastic anemia. J Pediatr. 1976. 88:784–789.

3. Sung HJ, Kim SJ, Lee JH, Lee G, Lee KA, Choi CW, Kim BS, Kim JS. Persistent anemia in a patient with diffuse large B cell lymphoma: pure red cell aplasia associated with latent Epstein-Barr virus infection in bone marrow. J Korean Med Sci. 2007. 22:Suppl. S167–S170.

4. Beutler E, Blume KG, Kaplan JC, Löhr GW, Ramot B, Valentine WN. International Committee for standardization in Haematology: recommended methods for red-cell enzyme analysis. Br J Haematol. 1977. 35:331–340.

5. Wallin JM, Buoncristiani MR, Lazaruk KD, Fildes N, Holt CL, Walsh PS. TWGDAM validation of the AmpFISTR blue PCR amplification kit for forensic casework analysis. J Forensic Sci. 1998. 43:854–870.

6. Boulard-Heitzmann P, Boulard M, Tallineau C, Boivin P, Tanzer J, Bois M, Barriere M. Decreased red cell enolase activity in a 40-year-old woman with compensated haemolysis. Scand J Haematol. 1984. 33:401–404.

7. Lachant NA, Jennings MA, Tanaka KR. Partial erythrocyte enolase deficiency: a hereditary disorder with variable clinical expression. Blood. 1986. 65:55A.
8. Perdahl EB, Naprstek BL, Wallace WC, Lipton JM. Erythroid failure in Diamond-Blackfan anemia is characterized by apoptosis. Blood. 1994. 83:645–650.

9. Gazda H, Lipton JM, Willig TN, Ball S, Niemeyer CM, Tchernia G, Mohandas N, Daly MJ, Ploszynska A, Orfali KA, Vlachos A, Glader BE, Rokicka-Milewska R, Ohara A, Baker D, Pospisilova D, Webber A, Viskochil DH, Nathan DG, Beggs AH, Sieff CA. Evidence for linkage of familial Diamond-Blackfan anemia to chromosome 8p23.3-p22 and for non-19q non-8p disease. Blood. 2001. 97:2145–2150.

10. Cmejla R, Cmejlova J, Handrkova H, Petrak J, Pospisilova D. Ribosomal protein S17 gene (RPS17) is mutated in Diamond-Blackfan anemia. Hum Mutat. 2007. 23:1178–1182.

11. Quigley JG, Gazda H, Yang Z, Ball S, Sieff CA, Abkowitz JL. Investigation of a putative role for FLVCR, a cytoplasmic heme exporter, in Diamond-Blackfan anemia. Blood Cells Mol Dis. 2005. 35:189–192.

12. Willig TN, Pérignon JL, Gustavsson P, Gane P, Draptchinskaya N, Testard H, Girot R, Debré M, Stéphan JL, Chenel C, Cartron JP, Dahl N, Tchernia G. The DBA Working Group of Societe d'Immunologie Pediatrique (SHIP). High adenosine deaminase level among healthy probands of Diamond Blackfan anemia (DBA) cosegregates with the DBA gene region on chromosome 19q13. Blood. 1998. 92:4422–4427.
13. Tanphaichitr VS, Suvatte V, Issaragrisil S, Mahasandana C, Veerakul G, Chongkolwatana V, Waiyawuth W, Ideguchi H. Successful bone marrow transplantation in a child with red blood cell pyruvate kinase deficiency. Bone Marrow Transplant. 2000. 26:689–690.

14. Liesveld JL, Rothberg PG. Mixed chimerism in SCT: conflict or peaceful coexistence? Bone Marrow Transplant. 2008. 42:297–310.

15. Wu CJ, Gladwin M, Tisdale J, Hsieh M, Law T, Biernacki M, Rogers S, Wang X, Walters M, Zahrieh D, Antin JH, Ritz J, Krishnamurti L. Mixed haematopoietic chimerism for sickle cell disease prevents intravascular haemolysis. Br J Haematol. 2007. 139:504–507.

16. Walters MC, Patience M, Leisenring W, Rogers ZR, Aquino VM, Buchanan GR, Roberts IA, Yeager AM, Hsu L, Adamkiewicz T, Kurtzberg J, Vichinsky E, Storer B, Storb R, Sullivan KM. Stable mixed hematopoietic chimerism after bone marrow transplantation for sickle cell anemia. Biol Blood Marrow Transplant. 2001. 7:665–673.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download