Abstract
We investigated the distribution and navigation of periprostatic nerve fibers and constructed a 3-dimensional model of nerve distribution. A total of 5 cadaver specimens were serially sectioned in a transverse direction with 0.5 cm intervals. Hematoxylineosin staining and immunohistochemical staining were then performed on whole-mount sections. Three representative slides from the base, mid-part, and apex of each prostate were subsequently divided into 4 sectors: two lateral, one ventral, and one dorsal (rectal) part. The number of nerve fibers, the distance from nerve fiber to prostate capsule, and the nerve fiber diameters were analyzed on each sector from the representative slides by microscopy. Periprostatic nerve fibers revealed a relatively even distribution in both lateral and dorsal parts of the prostate. There was no difference in the distances from the prostate capsule to nerve fibers. Nerve fibers in the ventral area were also thinner as compared to other areas. In conclusion, periprostatic nerve fibers were observed to be distributed evenly in the periprostatic area, with the exception of the ventral area. As the number of nerve fibers on the ventral part is fewer in comparison, an excessive high up incision is insignificant during the nerve-sparing radical prostatectomy.
Radical retropubic prostatectomy is the surgical treatment of choice for patients with localized prostate cancer. Numerous studies have been published demonstrating excellent tumor control, good functional results, and low morbidity associated with the procedure (1-4).
However, the major long-term morbidity from radical retropubic prostatectomy that remains is erectile dysfunction, despite advances in surgical techniques. Prior to studies done by Walsh and Donker (5) using male fetuses, the cause of erectile dysfunction after radical prostatectomy was not well understood. They proposed and eventually demonstrated that erectile dysfunction occurred secondary to the injury of cavernosal nerves. These nerves were identified branching from the pelvic plexus and running as a plexus of small nerves within a prominent neurovascular bundle on the posterolateral border of the prostate, terminating in the region of the membranous urethra. These nerves are mainly concentrated laterally to the prostate and these neural structures are referred to as neurovascular bundles.
Nerve sparing radical retropubic prostatectomy has led to improvements in potency rates, with studies reporting a 16 to 76% recovery of erectile function in men whose bilateral neurovascular bundles were preserved and 0 to 56% in those with unilateral neurovascular bundle preservation (6, 7). This variability can be attributed to the fact that there was no definite and exact anatomy of periprostatic nerve fibers, especially the cavernosal nerves. Although some papers about the anatomy of periprostatic nerves were published recently, there are still controversies about detailed descriptions of the exact periprostatic nerve distribution in the literature. Thus, in the present study, we described periprostatic nerve distribution and constructed a 3-dimensional model of nerve distribution.
The prostate, together with seminal vesicle, bladder, and rectum, was removed en bloc from five adult male human cadavers (age at death 43-72 yr) after filling urinary bladder with 40% formaldehyde using urethral catheter. The specimens were fixed with 40% formaldehyde until use for pathologic study. Each specimen was sliced by 5 mm step sections from the base of the prostate to the apex, and a total of eight slices of whole-mount histologic sections were embedded in paraffin, and prepared, and then stained with anti-S-100 antibody neural stain to delineate the precise location of this neural tissue.
Immunostaining with anti-S-100 protein antibody was performed by dewaxing the slides in xylene three times for three minutes and then rehydrating in ethanol (two changes of three minutes in 100% ethanol and two changes of three minutes in 90% ethanol) and distilled water. The rabbit polyclonal primary antibody to S-100 protein (Immunon, Pittsburgh, PA, USA) was applied in a 1:500 dilution and incubated for one hour at room temperature. The samples were then washed in PBS, subjected to EnVision-HRP kit (DAKO, Carpinteria, CA, USA), and the reaction product was visualized with chromogen 3, 3'-diaminobenzidine (DAB) for three minutes. Finally, samples were counterstained with hematoxylin and dehydrated in alcohol and xylene.
The stained whole-mount section slide was divided into four arbitrary sectors: two laterals, one ventral, and one dorsal (rectal side) according to one fourth the circumference of whole-mount specimens. Whole-mount specimens were then divided by two axes, such as from 1.5 to 7.5 o'clock and 10.5 to 4.5 o'clock direction (Fig. 1), and three representative slides of each cadaver were analyzed by microscopy. Each slide was taken from the base, mid-part, and apex of the prostate. A pathologist counted the nerve fibers expressing S-100 protein (Fig. 2). Nerve fibers 100 micrometer or greater in diameter were counted in ×200 magnification microscopically (Olympus BX51; Tokyo, Japan), in addition to the number of nerve fibers, the distance from nerve fiber to the true prostate capsule, and nerve fiber diameter on each sector from representative slides.
The three-dimensional periprostatic nerve distribution model was made by connecting the stained nerve fibers from the same location of the same sectors of the eight whole-mount slides from each prostate and reconstructing its image after taking a picture of the three-dimensional model (Fig. 3).
For statistical analysis, the difference in variables was assessed using ANOVA and Kruskal-Wallis nonparametric ANOVA. Statistical significance in this study was considered at P<0.05. All analysis was performed with SPSS® for Windows, version 13.0.
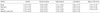
The average number of nerve fibers located in the ventral part of the prostate was 5.75±1.20, and comparatively, the average number in the dorsal (rectal) part was 28.50±2.17. There were even fewer nerve fibers in the ventral part of the prostatic base area, numbering 3.75±1.38. In the right lateral part the average number of nerve fibers was 25.25±9.92, and in the left lateral part 25.75±12.76; thus the number of nerve fibers in the dorsal (rectal), right lateral, and left lateral parts of the prostate capsule showed no significant difference, and nerve fibers were distributed evenly around the prostatic capsule microscopically in the posterior, right lateral, and those in left lateral areas. However, nerve fibers in the ventral part were small in number compared to the dorsal, right lateral, and left lateral parts at all levels (P=0.001) (Table 1). Moving from base to apex, the average number of nerve fibers increased in the ventral area, but this increase was not statistically significant (P=0.386). The average distance from prostatic capsule to nerve fibers was 1.73±0.43 mm in the ventral part, 1.80±0.16 mm in the dorsal (rectal) part, 1.58±0.26 mm in the right lateral part, and 1.23±0.29 mm in the left lateral part. There was no difference in the average distances when comparing the four different parts statistically (P=0.266). Also there was no significant difference among the base, mid-part, and apex levels (P=0.673) (Table 2).
The average thicknesses of nerve fibers in the ventral and dorsal parts were 0.19±0.02 mm and 0.30±0.03 mm, and those in the right and left lateral parts were 0.30±0.03 mm and 0.28±0.03 mm, respectively. There was no difference in nerve fiber thickness according to level such as base, midpart, and apex (P=0.180). However, the average thickness of the nerve fibers in the ventral part was significantly decreased as compared to the other parts (P=0.005) (Table 3).
The three-dimensional model of the periprostatic nerve fibers revealed an almost even distribution and nearly similar thickness of periprostatic nerve fibers on dorsal and both lateral parts. Furthermore, there was absence of a cord-like structure, such as neurovascular bundle, noted on the study. However, the nerve fibers in the ventral part were substantially fewer in number and decreased in thickness.
Traditionally, it was thought that cavernosal nerves branched from the pelvic plexus and ran as a plexus of small nerves within a prominent cord-like neurovascular bundle on the posterolateral border of the prostate (5, 8).
New advancements in surgery, including the use of laparoscopic and robotic modalities and magnifying visual devices in open surgery, have enabled precise nerve dissection. However, despite all these advancements in nerve preservation or restoration, potency rates have remained unsatisfactory (9-11). Recently, several descriptions of the neurovascular bundle have been proposed: The neurovascular bundle, in contrast to the usual concept, appears to contain few pelvic splanchnic nerve components at the bladder-prostate junction. The pelvic splanchnic nerve branches demonstrate a spray-like distribution, and caudal branches reach the dorsolateral portion of the prostate at levels more than 20 mm inferior to the bladder-prostate junction. Therefore, the cavernous nerves appear to be spread and located beyond the neurovascular bundle (12). Tewari et al. (13) found, in addition to the main neurovascular bundles, other nerve branches running between the prostatic capsule and endopelvic fascia, and called them distal accessory nerve pathway. According to these authors, this pathway could explain the unpredictable response to erection recovery and the lack of correlation between surgeon perception of the quality of neurovascular sparing and functional results after radical prostatectomy. Recently, several descriptions of the neurovascular bundle have shown variations in the distributions of autonomic fibers between different individuals. About half of the patients have been reported as having a 'fan-like' nerve fiber distribution on the lateral aspect of the prostate (14).
As mentioned above, the traditional knowledge of the neurovascular bundle has been challenged. Therefore, we performed this study to distinguish microscopic features and anatomic navigation of periprostatic nerves using male adult cadavers. We found that the number of periprostatic nerve fibers was distributed evenly to dorsal and both lateral area of the prostate in our study. Unlike the study of Kiyoshima et al. (14), no cord-like neurovascular bundle was observed in any cadaver case in our study. In addition, the distances from the prostatic capsule were almost the same in both the lateral and dorsal (rectal) parts of the base, middle, and apex levels of the prostate. These data, including numerical values about periprostatic nerve fibers, have not been reported and will serve as a guide for improved results for nerve sparing radical prostatectomy.
Several urologists reported surgical techniques according to the anatomy of the neurovascular bundle related to postoperative sexual dysfunction (14, 15). Lunacek et al. (16) suggested a modified technique of nerve sparing called "curtain dissection", which involves incising the periprostatic fascia and dissecting the neurovascular bundle far more anteriorly than previously described. Graefen et al. (2) reported the technique of open retropubic nerve-sparing radical prostatectomy. In their study, the parapelvic fascia of the prostate is incised at the lateroventral aspect of the prostate at 10 o'clock and 2 o'clock. They noted the importance of starting the incision high up on the ventral aspect of the prostate to preserve a maximum number of nerve fibers because a substantial number of nerve fibers are located at the ventral area. It has been shown that potency rates strongly correlate with the number of preserved nerve fibers.
Recently, robotic radical prostatectomy was subsequently developed and popularized by several surgeon groups. Menon et al. had introduced their modified technique of robotic radical prostatectomy, named Vattikuti Institute Prostatectomy (17). The features of their technique are early transaction of the bladder neck, preservation of the prostatic fascia (veil of Aphrodite), and control of the dorsal vein complex after dissection of the prostatic apex. They reported that the veil nerve sparing procedure offers superior erectile function compared with conventional nerve-sparing surgery without compromising cancer control (18).
Savera et al. (19) performed a histologic study of comparison between the Veil of Aphrodite technique and standard nerve-sparing technique during a robotic prostatectomy. They concluded that the Veil of Aphrodite technique is a safe procedure that effectively preserved the lateral prostatic fascia, which contains nerve bundles that run along the surface of the anterolateral zones. In their study, the nerve bundle counts of the anterolateral zones was different between the two techniques with statistical significance.
Our result means modified nerve-sparing techniques by incising the periprostatic fascia more anteriorly are feasible for saving periprostatic nerves. But an excessive high up incision (over 2, 10 o'clock) would not be effective because the number of nerve fibers of both lateral parts is much more than that of the ventral part of the periprostatic area. These findings are differernt from Eichelberg's reports that the sum of the median percentage of nerves detected in anterior half of the prostate was more than 20% (20). Our result revealed that the mean percentage of nerves in ventral part was 6.7% (range: 4.5-9.4%) (Table 1).
According to Costello et al. (21), the majority of nerves which exist on the anterior aspect of the prostate laterally are not functionally significant parasympathetic nerves. So, there is little evidence to support higher incisions in the lateral prostatic fascia anatomically.
Based on this study, the number of periprostatic nerve fibers is evenly distributed on both lateral and dorsal (rectal) parts from base to apex of the prostate without forming any cord-like structures. Because the number of nerve fibers on the ventral part is few in comparison, an excessive high up incision over 2, 10 o'clock on the ventral part of the prostate is insignificant during nerve-sparing radical prostatectomy.
Figures and Tables
Fig. 1
Classification into four parts in whole-mount section of prostate with immunochemical staining using anti-S-100 protein antibody (asterix, urethra inserted Foley catheter previously).

Fig. 2
Histological section showing nerve distributions at ventral (A), dorsal (rectal, B), right lateral (C), and left lateral (D) parts. Nerve fibers in the ventral part (A) show decreased diameter and number compared to other parts (original magnification ×40, arrow, nerve fibers stained with anti-S-100 protein antibody).

Fig. 3
A 3-dimensional model of navigation of periprostatic nerve fibers made by connection of silks.

References
1. Augustin H, Hammerer P, Graefen M, Palisaar J, Noldus J, Fernandez S, Huland H. Intraoperative and perioperative morbidity of contemporary radical retropubic prostatectomy in a consecutive series of 1243 patients: results of a single center between 1999 and 2002. Eur Urol. 2003. 43:113–118.

2. Graefen M, Walz J, Huland H. Open retropubic nerve-sparing radical prostatectomy. Eur Urol. 2006. 49:38–48.

3. Hull GW, Rabbani F, Abbas F, Wheeler TM, Kattan MW, Scardino PT. Cancer control with radical prostatectomy alone in 1,000 consecutive patients. J Urol. 2002. 167:528–534.

4. Michl U, Graefen M, Noldus J, Eggert T, Huland H. Functional results of various surgical techniques for radical prostatectomy. Urologe A. 2003. 42:1196–1202.
5. Walsh PC, Donker PJ. Impotence following radical prostatectomy: insight into etiology and prevention. J Urol. 1982. 128:492–497.

6. Geary ES, Dendinger TE, Freiha FS, Stamey TA. Nerve sparing radical prostatectomy: a different view. J Urol. 1995. 154:145–149.

7. Walsh PC, Mostwin JL. Radical prostatectomy and cystoprostatectomy with preservation of potency. Results using a new nerve-sparing technique. Br J Urol. 1984. 56:694–697.

8. Hinman F. Prostate and urethral sphincter, Atlas of urosurgical anatomy. 1993. Philadelphia: WB Saunders Co;345.
9. Walsh PC. Nerve grafts are rarely necessary and are unlikely to improve sexual function in men undergoing anatomic radical prostatectomy. Urology. 2001. 57:1020–1024.

10. Noldus J, Michl U, Graefen M, Haese A, Hammerer P, Huland H. Patient-reported sexual function after nerve-sparing radical retropubic prostatectomy. Eur Urol. 2002. 42:118–124.

11. Kim ED, Nath R, Slawin KM, Kadmon D, Miles BJ, Scardino PT. Bilateral nerve grafting during radical retropubic prostatectomy: extended follow-up. Urology. 2001. 58:983–987.

12. Takenaka A, Murakami G, Soga H, Han SH, Arai Y, Fujisawa M. Anatomical analysis of the neurovascular bundle supplying penile cavernous tissue to ensure a reliable nerve graft after radical prostatectomy. J Urol. 2004. 172:1032–1035.

13. Tewari A, Takenaka A, Mtui E, Horninger W, Peschel R, Bartsch G, Vaughan ED. The proximal neurovascular plate and the tri-zonal neural architecture around the prostate gland: importance in the athermal robotic technique of nerve-sparing prostatectomy. BJU Int. 2006. 98:314–323.

14. Kiyoshima K, Yokomizo A, Yoshida T, Tomita K, Yonemasu H, Nakamura M, Oda Y, Naito S, Hasegawa Y. Anatomical features of periprostatic tissue and its surroundings: a histological analysis of 79 radical retropubic prostatectomy specimens. Jpn J Clin Oncol. 2004. 34:463–468.

15. Montorsi F, Salonia A, Suardi N, Gallina A, Zanni G, Briganti A, Deho F, Naspro R, Farina E, Rigatti P. Improving the preservation of the urethral sphincter and neurovascular bundles during open radical retropubic prostatectomy. Eur Urol. 2005. 48:938–945.

16. Lunacek A, Schwentner C, Fritsch H, Bartsch G, Strasser H. Anatomical radical retropubic prostatectomy: 'curtain dissection' of the neurovascular bundle. BJU Int. 2005. 95:1226–1231.

17. Menon M, Tewari A, Peabody J. Vattikuti Institute prostatectomy: technique. J Urol. 2003. 169:2289–2292.

18. Menon M, Shrivastava A, Kaul S, Badani KK, Fumo M, Bhandari M, Peabody JO. Vattikuti Institute prostatectomy: contemporary technique and analysis of results. Eur Urol. 2007. 51:648–657.

19. Savera AT, Kaul S, Badani K, Stark AT, Shah NL, Menon M. Robotic radical prostatectomy with the "Veil of Aphrodite" technique: histologic evidence of enhanced nerve sparing. Eur Urol. 2006. 49:1065–1073.

20. Eichelberg C, Erbersdobler A, Michl U, Schlomm T, Salomon G, Graefen M, Huland H. Nerve distribution along the prostatic capsule. Eur Urol. 2007. 51:105–110.

21. Costello AJ, Dowdle B, Namdarian B, Murphy D. Immunohistochemical study of the cavernous nerves in the peri-prostatic region. 2009. In : American Urological Association Annual Meeting 25-30 April 2009; Chicago, Illinois, USA: Elsevier;577–578.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download