Abstract
Although little attention has been paid to the less common rheumatoid involvement of the thoracic and lumbar regions, some studies have shown that rheumatoid synovitis with erosive changes can develop in these diarthrodial joints. We report a patient with seropositive rheumatoid arthritis (RA) involving the thoracic and lumbar vertebra with a collapse of the T12 vertebra, who was treated with percutaneous vertebroplasty. In this case of a painful pathological fracture due to RA, percutaneous vertebroplasty was found to be helpful in eliminating the pain. The paper presents the histological evidence, the pathogenesis and treatment of the thoracolumbar lesions affected by RA with a review of the relevant literature.
Rheumatoid arthritis (RA) affecting the cervical spine is well described in the literature but little attention has been paid to the less common rheumatoid involvement of the thoracic and lumbar regions (1-4). Generally, the thoracic and lumbar portions of the spine are usually spared in RA. However, a review of the literature showed that rheumatoid synovitis with erosive changes can develop in these diarthrodial joints. The vertebral bodies and intervertebral discs may be involved through either enthesitis or an extension of the inflammatory process from the apophyseal joints (2, 3, 5-7). There are few reports describing collapse of the vertebrae affected by RA without synovitis and enthesitis (1, 4, 5, 8). This paper reports a case of multiple pathologic fractures caused by RA in a 47-yr-old woman who was treated with percutaneous vertebroplasty (PV) for intractable pain.
A 47-yr-old woman was transferred to the department of neurosurgery from the department of rheumatology as a result of unbearable low back pain that had suddenly become aggravated one week earlier. She had been suffering from seropositive RA since the age of 40 yr, and had been treated with bucillamine 200 mg/day, nabumetone 1,000 mg/day in another hospital. One month earlier, she felt severe back pain without trauma and was admitted to our institute.
The physical examination revealed tenderness over the thoracolumbar area. Joint swelling was also noted on the small joints of the hands and right elbow but there was no tenderness. The blood examination revealed a white blood cell count, hemoglobin concentration, erythrocyte sedimentation rate and C-reactive protein level of 7,400/mL, 13.1 g/dL, 10 mm/hr, and 2.24 mg/dL, respectively. The rheumatoid factor was high at 56 IU/mL and the anti-Nuclear antibody (ANA) was positive (1:160). The anti-cyclic citrullinated peptide antibody (Anti CCP) was 26 IU/mL. A plain radiographic examination of thoracolumbar spine (Fig. 1A) revealed multiple thoracolumbar fractures on T11, L2, and L3, and sclerosis of the vertebral end-plate without evidence of osteophyte formation. Immediate magnetic resonance imaging (MRI) (Fig. 1B, C) revealed vertebral involvement on T11, L2, L3, and L5, which was hyperintense on the gadolinium-enhanced T1 weighted images. A bone scintigram demonstrated increased uptake in the T12, L2, L3, and L5 spine, multiple metacarpophalangeal and proximalinterphalangeal joints of both hands. Dural radiography absorptiometry (DXA) revealed moderate osteopenia in the femoral neck (T score -1.6 SD) and vertebral body (T score -2.0). Her initial medications included bucillamine, non-steroid anti-inflammatory drugs and combinations of analgesics both intravenously and epidurally for multiple compression fractures. However, she had felt increasing pain while standing and lying down for a month.
Upon arrival to our department, she could not walk at all due to aggravated back pain. The new plain radiographs (Fig. 2A) showed the minor progression of compression with surrounding sclerosis at T11, L2, 3, 4, and L5, and a widening of the intervertebral disc space. There was a new compressed vertebral lesion at T12. The sagittal T2-weighted MRI (Fig. 2B, C) showed significant collapse of the T12 vertebral body with the retropulsion of bony fragments, which was evidence of acute fracture.
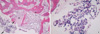
The patient underwent percutaneous vertebroplasty following a needle biopsy on the T12 vertebra (Fig. 3). After vertebroplasty, the patient experienced significant subjective pain relief without any neurological deficit. The postoperative course was good and there were no complications. A histological examination of the specimen obtained from the affected vertebra (Fig. 4) revealed areas of fibrosis with surrounding acute and chronic inflammatory cell infiltration including neutrophils, plasma cells and lymphocytes. And the bacteriological culture of the specimen for bacteria, fungi and mycobacterium tuberculosis was also negative. Finally, a pathological fracture due to the marrow involvement of rheumatoid arthritis was diagnosed based on the absence of any infectious signs, her history of RA and the diagnostic characteristics on the various imaging modalities. After bed rest for one week, she commenced a rehabilitation regimen with a hard corset to regain her walking ability. One year after the procedure, she could walk without pain.
Although the cervical spine is more commonly involved in RA, and atlantoaxial subluxation is well known, there are some reports of thoracolumbar spine involvement in a few patients with RA (1-3, 6-9). With regard to the disease incidence, Heywood and Meyers reported a frequency of 0.94% (seven cases in 746 patients satisfying the criteria of definite rheumatoid arthritis) (2). Recently, Nakase et al. and Sakai et al. suggested that asymptomatic involvement is relatively common (7, 8). Usually, a radiological examination shows disc narrowing without osteophyosis, spondylolisthesis, osteoporosis and ill-defined margins of the apophyseal joints (2, 3). Several radiological features distinguish these patients from those with degenerative spondylosis. Of these, an ill-defined, blurred and eroded margin of the vertebral end-plates is most important (4).
Previous reports on the involvement of the thoracolumbar spine in RA dealt mainly with the radiological features and pathogenesis (1-4, 8). Three pathways for the involvement of the subcervical vertebra include synovitis in the apophyseal joints, inflammation of the disco-vertebral junction and rarely, granulomatous nodule formation in the marrow space of the vertebral bodies (2, 7). Synovitis probably begins in the apophyseal joints, slowing erosion of the cartilage and subchondral bone in precisely the same manner as that observed in the peripheral joints. The next lesion, rheumatoid spondylodiscitis, probably begins as an enthesopathy at the discovertebral junction. However, Shichikawa et al. suggested two different types of rheumatoid spondylodiscitis based on their histological findings in 2 cases (4). One patient showed a loss of intervertebral discs and destruction of the vertebral end plates. They suggested that the inflammatory degeneration of collagen at the junction between the disc and the vertebral end-pate leads to a loss of disc substance and invasive erosion of the end-plate. The other patient showed granulomatous nodular lesions that can develop occasionally in the marrow of the vertebral bodies and then spread, causing osteolysis and weakening, which is followed by collapse of the vertebral body.
Histologically, several authors reported the histological findings of vertebral involvement by rheumatoid arthritis. These lesions demonstrate extensive areas of fibrinoid necrosis surrounded by proliferated connective tissue with some histiocytes, plasma cells and chronic inflammatory cells. In contrast, vertebral bodies with fractures secondary to osteoporosis are characterized consistently by focal areas of endochondral new bone formation adjacent to the avascular necrotic bone and unreactive marrow (10). Diamond et al. also identified four stages of fracture healing in a histological analysis of fracture healing in an osteoporotic vertebral fracture (11). These included: 1) fracture hematoma with necrotic bone and fibrovascular stroma; 2) chondrogenesis and bone matrix synthesis; 3) endochondral ossification and woven bone formation; and 4) bone remodelling and modelling. In our case, the histological findings of specimen in conjunction with the clinical and serological data suggested that the spinal lesions were due to rheumatoid arthritis. Moreover, it is likely that the inflammatory tissue arose from the marrow space and not from the intervertebral disc, as evidenced by the histological and radiological findings.
The surgical treatment of the thoracolumbar lesions affected by RA are quite rare, and they need to be tailored to each patient according to the location of the lesion within the vertebra and the patient's symptoms (2, 6, 8, 9). A laminectomy may allow adequate decompression in selected cases, particularly those with an epidural rheumatoid nodule or spinal stenosis (2, 6). An anterior corpectomy is effective, and adequate decompression can be achieved in patients with marked kyphosis and a collapsed vertebral body. In our case, percutaneous vertebroplasty was successful. Percutaneous vertebroplasty, which is usually performed using polymethylmethacrylate, is a relatively new treatment for symptomatic vertebral RA. The pain in the lumbar region disappeared immediately. The stiffness of the anterior and middle columns was also restored. This suggests that patients who present with a pathological compression fracture and intractable back pain are good candidates for PV. However, PV is a palliative treatment, and it is unlikely to reverse the neurological deficits in patients with significant thecal compression as a result of the RA lesion. Moreover, the long-term efficacy of vertebroplasty for thoracolumbar involvement of RA is unknown. Therefore, a careful and long-term follow-up for the recurrence of symptoms after the procedure is essential.
In conclusion, thoracolumbar involvement in rheumatoid arthritis should be more common than previously suggested in the literature. Therefore, a careful radiological examination of the spine is essential in patients affected by RA who present with acute low back pain. In the case of a painful pathological fracture due to RA, PV is helpful in eliminating the pain, at least in the short-term.
Figures and Tables
Fig. 1
A plain radiographic examination of the patient's thoracolumbar spine upon admission (A) shows multiple thoracolumbar fractures on T11, L2, and 3, and sclerosis of the vertebral end-plate without evidence of osteophyte formation. An immediate magnetic resonance imaging (MRI) scan (B, C) shows vertebral involvement on T11, L2, L3, and L5 that appeared hyperintense on the gadolinium enhanced images.

Fig. 2
A plain radiograph after 1 month (A) shows a new pathologic fracture in T12 as well as erosion of the L3-4 disc space with surrounding sclerosis and adjacent discs exhibited ballooning. The sagittal T1-weighted MRI (B) shows a marked collapse of T12 with retropulsion of the bony fragments, which is evidence of an acute fracture. The collapsed T12 and other lumbar lesions after gadolinium contrast enhancement (C).
References
1. Baggenstoss AH, Bickel WH, Ward LE. Rheumatoid granulomatous nodules as destructive lesions of vertebrae. J Bone Joint Surg Am. 1952. 24:601–609.

2. Heywood AW, Meyers OL. Rheumatoid arthritis of the thoracic and lumbar spine. J Bone Joint Surg Br. 1986. 68:362–368.

3. Kawaguchi Y, Matsuno H, Kanamori M, Ishihara H, Ohmori K, Kimura T. Radiologic findings of the lumbar spine in patients with rheumatoid arthritis, and a review of pathologic mechanisms. J Spinal Disord Tech. 2003. 16:38–43.

5. Biasi D, Caramaschi P, Carletto A, Pacor ML, Bambara LM. A case of rheumatoid arthritis with lumbar spine involvement. Rheumatol Int. 1995. 15:125–126.

6. Kawaji H, Miyamoto M, Gembun Y, Ito H. A case report of rapidly progressing cauda equina symptoms due to rheumatoid arthritis. J Nippon Med Sch. 2005. 72:290–294.

7. Sakai T, Sairyo K, Hamada D, Katoh S, Takata Y, Shinomiya F, Yasui N. Radiological features of lumbar spinal lesions in patients with rheumatoid arthritis with special reference to the changes around intervertebral discs. Spine J. 2008. 8:605–611.

8. Nakase T, Fujiwara K, Kohno J, Owaki H, Tomita T, Yonenobu K, Ochi T. Pathological fracture of a lumbar vertebra caused by rheumatoid arthritis--a case report. Int Orthop. 1998. 22:397–399.
9. Inaoka M, Tada K, Yonenobu K. Problems of posterior lumbar interbody fusion (PLIF) for the rheumatoid spondylitis of the lumbar spine. Arch Orthop Trauma Surg. 2002. 122:73–79.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download