Abstract
Regardless of the preoperative morphology and the type of operation, left ventricular outflow tract obstruction (LVOTO) after biventricular repair of double outlet right ventricle (DORV) may develop. This report presents our 10-yr experience with surgical management of LVOTO after biventricular repair of DORV. Between 1996 and 2006, 15 patients underwent reoperation for subaortic stenosis after biventricular repair of DORV. The mean age at biventricular repair was 23.3±18.3 months (1.1-64.2). Biventricular repairs included tunnel constructions from the left ventricle to the aorta in 14 cases and an arterial switch operation in one. The mean left ventricle-to-aorta peak pressure gradient was 54.0±37.7 mmHg (15-140) after a mean follow-up of 9.5±6.3 yr. We performed extended septoplasty in nine patients and fibromuscular resection in six. There were no early or late mortality. There was one heart block and one aortic valve injury after an extended septoplasty, and two and one after a fibromuscular resection. No patient required reoperation for recurrent subaortic stenosis. The mean pressure gradient was 11.2±11.4 mmHg (0-34) after a mean follow-up of 5.6±2.7 yr. Extended septoplasty is a safe and effective method for the treatment of subaortic stenosis, especially in cases with a long-tunnel shaped LVOTO.
A double outlet right ventricle (DORV) includes a broad spectrum of anatomic variants and associated malformations, and the optimal management remains controversial. The preferred surgical approach for a DORV is an intraventricular tunnel with or without extracardiac procedures such as an arterial switch operation or a right ventricle-to-pulmonary artery conduit formation (Rastelli procedure). Regardless of its preoperative morphology and the type of operation, obstructive subaortic lesions after biventricular repair of a DORV may develop, even in the presence of a sufficient left ventricular outflow tract and a non-restrictive ventricular septal defect (VSD). This report presents our 10-yr experience with the surgical management of left ventricular outflow tract obstruction (LVOTO) after biventricular repair of a DORV.
Between 1996 and 2006, 15 patients underwent reoperation for subaortic stenosis after biventricular repair of a DORV at Seoul National University Children's Hospital and Sejong General Hospital. Two of the patients underwent biventricular repair elsewhere. The other patients underwent biventricular repair between 1985 and 2000, and 295 patients underwent biventricular repair in the same period. Therefore, the incidence of subaortic stenosis after biventricular repair of a DORV was 4.4% (13/295).
The diagnosis of a DORV and subaortic stenosis after biventricular repair of a DORV was based on a combination of preoperative echocardiographic and angiographic findings as well as surgical inspection. A diagnosis of DORV was made with the application of the '50% rule' that one great artery originate entirely and the other more than 50% from the right ventricle (1, 2). The term 'non-committed VSD' was used to describe a VSD which lies at a distance from both the aortic and pulmonary annulus greater than the aortic diameter (3, 4). The term 'DORV-TGA type' (or Taussig-Bing anomaly) was a DORV with a subpulmonary VSD and without pulmonary stenosis, originating the aorta entirely and more than 50% of the pulmonary artery from the right ventricle (5, 6).
Based on the surgical techniques used for subaortic stenosis repair, we divided the patients into two subgroups; the Extended Septoplasty (ES) group (n=9) and the Fibro-Muscular Resection (FMR) group (n=6). Preoperative conventional angiography was performed in 13 patients (8 in the ES group, 5 in the FMR group). But left-sided angiography was not performed in one of them, in the FMR group, because of floating tissue in the left ventricular outflow tract (LVOT). Therefore, there were 12 angiography-proven left ventricle-to-aorta peak pressure gradients. Magnetic resonance angiography or echocardiography were performed in the other 2 patients. In the ES group, the main cause of a reoperation was LVOTO with a peak pressure gradient of more than 50 mmHg except for one patient, who had a peak pressure gradient 15 mmHg and required a reoperation for right ventricle-to-pulmonary artery conduit stenosis. By contrast, in the FMR group, the main cause of reoperation was not LVOTO, but right ventricle-to-pulmonary artery conduit stenosis (n=2), severe pulmonary regurgitation combined with a right ventricular outflow tract (RVOT) aneurysm (n=1), a neoaorta stenosis after an arterial switch operation (n=1), an ascending aortic aneurysm (n=1) and pacemaker failure (n=1). All patients in the FMR group had a peak pressure gradient less than 30 mmHg. Therefore, the ES group had a significantly higher peak pressure gradient than the FMR group (70.8 ±35.5 mmHg, n=8 and 20.5±4.9, n=4 respectively, P=0.048). All but one patient in the ES group had a long-tunnel shaped LVOTO. On the other hand, all but one in the FMR group had a localized LVOTO.
We reviewed the clinical records including operative reports, pre- and postoperative echocardiographic and angiographic studies retrospectively. Seoul National University Hospital Institutional Review Board (study approval number H-0603-093-170) approved this study and individual consent for the study was waived due to its retrospective medical record review design.
Of the 15 patients, nine were boys and six were girls. Overall, the mean age at the time of biventricular repair of the DORV was 23.3±18.3 months (ranged from 1.1 to 64.2 months, median age 23.1). The ES group was younger than the FMR group at the time of biventricular repair of the DORV; this difference was not significant (21.6±19.2 months and 25.9±18.2 respectively, P=0.864). The initial diagnosis of a DORV was the VSD type (DORV with subaortic VSD) in 3 patients, the Fallot type (DORV with subaortic or doubly committed VSD and pulmonary outflow stenosis) in 8, the non-committed VSD type in 3 and TGA type in 1 patient.
Five patients in the ES group and four in the FMR group had an initial subaortic stenosis including a restrictive VSD or subaortic conal or septal hypertrophic lesions. One in the ES group had an anomalous tricuspid chordae attachment to the conal septum. The patient with the Taussig-Bing anomaly had a single coronary artery pattern from the right coronary sinus. One in the FMR group had an atrioventricular septal defect (AVSD). Two in the FMR group underwent modified Blalock-Taussig shunt and no patient underwent pulmonary artery banding before the biventricular repair.
Fourteen patients underwent a tunnel construction from the left ventricle to the aorta and one patient with the Taussig-Bing anomaly in the FMR group underwent an arterial switch operation with a patch committing the left ventricle to the pulmonary artery (neo-aorta). Four patients in the ES group and two in the FMR group required anterior or anterocaudal VSD enlargement, resection of the subaortic conal or septal hypertrophy or both for the treatment of initial subaortic stenosis. Concomitant procedures were as follows: tricuspid valve chordae transfer who had an anomalous tricuspid chordae attachment to the conal septum (n=1), mitral annuloplasty (n=1) in the ES group and AVSD repair (n=1), tricuspid valvuloplasty (n=1) in the FMR group.
No patient had a LV-to-Aorta peak pressure gradient (ΔP) more than 20 mmHg by echocardiography at hospital discharge. Three patients required a permanent pacemaker implantation due to heart block in the FMR group. There were two reoperations after the biventricular repair: repair of a residual VSD in the ES group (n=1), and mitral valve replacement in a patient with AVSD in the FMR group (n=1).
Fibromuscular resection was usually performed through transarterial approach and transatrial when needed. It depended on surgeon's preference whether extended septoplsty was performed. Extended septoplasty was first described at 1990 in patients with subaortic stenosis after VSD repair (7). We performed an extended septoplasty as follows (Figs. 1, 2). A longitudinal incision was made at the previous patch, and extended toward the apex, beyond the patch, into the apical interventricular septum. It was extended into the conal septum avoiding direct injury to the aortic valve. The new patch was then trimmed along the extended incision, and inserted to secure a sufficient pathway in the LVOT.
Statistical analysis was performed using SPSS 12.0K software (SPSS, Inc, Chicago, IL, USA). Continuous variables were compared using the Mann-Whitney U test and discrete variables were analyzed using Fisher's exact test. All data are expressed as mean±standard deviation with ranges. The P values less than 0.05 were considered significant.
There were no early or late deaths and there was complete follow-up for all patients. Only one patient in ES group had a postoperative pressure gradient >20 mmHg (from 70 mmHg by angiography to 25 by echocardiography) at hospital discharge. The overall time for patient follow-up ranged from 16.5 months to 10.9 yr with a mean follow-up of 5.6±2.7 yr. The overall recent peak pressure gradient was 11.2±11.4 mmHg (13.9±11.2 mmHg in ES group, and 7.2±11.3 in FMR group). Three patients had a newly developed peak pressure gradients >20 mmHg by recent echocardiographic follow-up (25 mmHg and 34 in ES group, 25 in FMR group respectively).
According to the intraoperative findings, all patients in the FMR group had LVOTO mainly caused by subarterial conal muscle hypertrophy with a non-restrictive VSD inlet. And eight patients had subarterial muscle hypertrophy or residual conal septum, who underwent simple fibromuscular resection coincidentally, and 4 had a restirictive VSD inlet in the ES group.
The concomitant procedures were as follows: aortic valvuloplasty (n=3:2 planned and 1 unexpected), tricuspid annuloplasty (n=1), pulmonary valve replacement (n=3), right ventricular outflow tract widening (n=2) and main pulmonary artery angioplasty (n=1) in the ES group, and unexpected aortic valvuloplasty (n=1), tricuspid valvuloplasty (n=1), pulmonary valve replacement (n=1), and a left and right pulmonary artery angioplasty (n=1) in FMR group.
The aortic valve was injured in one patient in each group during the procedures associated with the relief of subaortic stenosis. Primary repairs were done in these patients, and additional pericardial patch repair of perforated site was performed at 17 months after the operation for LVOTO in one patient of FMR group. This patient showed moderate aortic regurgitation by recent echocardiography. The other patient showed mild aortic regurgitation at 56 months postoperative echocardiography follow-up. Heart block, which required the implantation of a permanent pacemaker, developed in one patient in the ES group and two in FMR group. No patient required reoperation for recurrence of a LVOTO.
Table 1 includes preoperative, biventricular repair, reoperative and follow-up data which compared between the two subgroups.
Subaortic stenosis can occur after surgical repair of several congenital heart defects without an initial LVOTO such as coarctation of the aorta, atrioventricular septal defect, DORV, simple VSD, transposition of the great arteries with a VSD and pulmonary stenosis, an interrupted aortic arch, and tetralogy of Fallot (8, 9). In the case of a DORV, especially with a non-committed ventricular septal defect, new surgical techniques have been reported to resolve the problem of ventricular outflow tract stenosis (4, 10). Nevertheless, an intraventricular repair may form a long and akinetic area in the LVOT.
Subaortic stenosis, such as a restrictive ventricular septal defect and a subaortic conal or septal hypertrophy, which may develop after pulmonary artery banding, may be present before biventricular repair of the DORV. Subaortic stenosis is an independent risk factor for LVOTO after biventricular repair of a DORV (11) and it is important to relieve the subaortic stenosis completely during the biventricular repair by means of VSD enlargement and resection of the conal septum (12). However, subaortic stenosis after biventricular repair of a DORV may develop in 3.5-5.5% of cases, even in the presence of a sufficient LVOT and a non-restrictive VSD (11, 13, 14).
Many possible factors can explain the development of a LVOTO after biventricular repair of a DORV. A subaortic septal or conal muscle hypertrophy or fibrous tissue deposits caused by turbulent flow and the sinuous shape of the tunnelization (11); the decrease in the effective VSD size caused by the baffle itself or fibrous tissue around the VSD or the baffle (15); the diminution of the VSD orifice (11, 15). In addition, growth of the heart without concomitant increases in size of the VSD and baffle (11) and retraction or kinking of the baffle patch (15). Rychik and coworkers suggested 'geometric changes' (16); the left ventricle undergoes geometric changes after a Rastelli operation or intraventricular repair for a DORV and subaortic obstruction may develop in patients with the greatest degree of ventricular contraction and VSD diminution early after biventricular repair.
Subaortic stenosis includes a broad spectrum of pathology from a subaortic membrane to a tunnel-like obstruction, and surgical procedures are chosen based on the anatomical type of subaortic stenosis. The surgical management of the LVOTO remains a surgical challenge in view of the goal of preservation of the aortic valve and the conduction system, ensuring complete relief of the LVOTO, and avoiding the recurrence of the LVOTO. In this study, all but one patient in the ES group had a long-tunnel shaped LVOTO (Fig. 3). On the other hand, all but one in the FMR group had a localized discrete LVOTO. Since the peak pressure gradient did not always correlate with the severity and morphologic features of the LVOTO, it is not always an indication for a certain type of surgery. Kalfa and coworkers (9) reported five recurrent LVOTOs after 33 surgical procedures for secondary (acquired) subaortic stenosis, after surgery for congenital heart anomalies. Belli and colleagues (11) reported that none of the six patients who underwent extended septoplasty required further reoperation, but four of nine patients who underwent fibromuscular resection or septal patch enlargement required further reoperation, and they suggested (3) a 'two stage management': the biventricular repair and reoperation for progressive subaortic stenosis in patients with a DORV non-committed VSD type. Considering the recurrence of LVOTO, extended septoplasty may be considered the preferred technique especially in cases with a long-tunnel shaped LVOTO, even if the left ventricle-to-aorta peak pressure gradient is not very high.
In this study, the fibromuscular resection group had a lower peak pressure gradient than the extended septoplasty group, because the fibromuscular resection group required closer observation so that early detection and surgery for the other causes could be performed before the LVOTO progressed.
Concerning the surgical relief of the LVOTO, the fibromuscular resection and extended septoplasty are alternatives to consider on a case-by-case basis. In this study, the extended septoplasty reduced the peak pressure gradient effectively from 70.8±35.5 mmHg to 13.9±11.2 especially in the patients with a long-tunnel shaped LVOTO. There was no difference in the early and late mortality, current functional status and morbidity, directly associated with the procedures, such as reoperation for recurrence and direct injury to the aortic valve or conduction systems. The fibromuscular resection is useful in patients with a mild or discrete subaortic stenosis especially combined with other sophisticated surgical problems because it is relatively simple, less time-consuming and the operator can focus on other complex procedures. In this study, surgical results for the fibromuscular resection were satisfactory considering the effective reduction of subaortic stenosis, no death, easily combined with other sophisticated procedures and no recurrence of the LVOTO.
There were some limitations in this study. At first, the overall follow-up period after surgery for the relief of subaortic stenosis (5.6±2.7 yr) is somewhat shorter than the overall interval from biventricular repair to reoperation (9.5±6.3 yr). Therefore, a further follow-up is needed, especially in three patients with newly developed peak pressure gradient >20 mmHg. In addition, the main reason for reoperation was LVOTO with a high peak pressure gradient in the extended septoplasty group, however, there were other causes than a LVOTO in the fibromuscular resection group. Considering this baseline difference, it is difficult to compare the outcomes of the two groups directly. Finally, this study was not a controlled and randomized trial but a retrospective medical record review study. Because the initial biventricular repairs were performed between 1985 and 2000, there were some confounding factors, such as technical improvements in the biventricular repair and understanding of LVOTO developmental mechanisms.
In conclusions, for surgical relief of subaortic stenosis after biventricular repairs of a DORV, fibromuscular resection and extended septoplasty are alternative options for surgery. Fibromuscular resection shows satisfactory results in cases with mild, discrete subaortic stenosis especially when combined with other surgical problems, and extended septoplasty is a safe and effective method and ensures complete relief of subaortic stenosis. The extended septoplasty is an excellent choice for surgery, especially in cases with a long-tunnel shaped LVOTO.
Figures and Tables
Fig. 1
Illustrations showing the extended septoplasty. (A) A right ventriculotomy (dotted curve) is made in the right ventricular outflow tract. (B) A longitudinal septal incision is made at the previous patch, and extended toward the apex, beyond the previous patch, into the interventricular septum, and toward the aortic valve, into the conal septum avoiding direct injury to the aortic valve. (C) The new patch is then trimmed along the extended septal incision, and inserted to secure a redundant pathway in the left ventricular outflow tract.

Fig. 2
Photograph, taken after the extended septal incision and some interrupted sutures for anchoring a new septal patch, showing the previous patch (arrow) and the septal incision (asterisk).
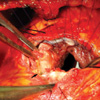
Fig. 3
Angiogram showing the long tunnel-shaped left ventricular outflow tract obstruction after biventricular repair of DORV.
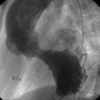
Table 1
Summary of data between the two groups

*calculated by means of echocardiography; †measured by angiography.
ES, extended septoplasty; FMR, fibro-muscular resection; DORV, double outlet right ventricle; VSD, ventricular septal defect; TB, Taussig-Bing; nc-VSD, non-committed ventricular septal defect; PS, pulmonary stenosis; ASO, arterial switch operation; ΔP, left ventricle-to-aorta peak pressure gradient; RV-PA, right ventricle-to-pulmonary artery; LVOTO, left ventricular outflow tract obstruction; NYHA Fc, New York Heart Association functional classification.
ACKNOWLEDGMENT
The authors are grateful to the Medical Research Collaborating Center of Seoul National University Hospital for providing a statistical review of this study.
References
1. Stark J. Stark J, de Leval M, editors. Double-Outlet Ventricles. Surgery for Congenital Heart Defects. 1994. 2nd ed. Philadelphia: WB Saunders;437–446.
2. Stellin G, Ho SY, Anderson RH, Zuberbuhler JR, Siewers RD. The surgical anatomy of double-outlet right ventricle with concordant atrioventricular connection and non-committed ventricular septal defect. J Thorac Cardiovasc Surg. 1991. 102:849–855.

3. Belli E, Serraf A, Lacour-Gayet F, Hubler M, Zoghby J, Houyel L, Planche C. Double-outlet right ventricle with non-committed ventricular septal defect. Eur J Cardiothorac Surg. 1999. 15:747–752.

4. Lacour-Gayet F, Haun C, Ntalakoura K, Belli E, Houyel L, Marcsek P, Wagner F, Weil J. Biventricular repair of double outlet right ventricle with non-committed ventricular septal defect (VSD) by VSD rerouting to the pulmonary artery and arterial switch. Eur J Cardiothorac Surg. 2002. 21:1042–1048.

5. Stellin G, Zuberbuhler JR, Anderson RH, Siewers RD. The surgical anatomy of the Taussig-Bing malformation. J Thorac Cardiovasc Surg. 1987. 93:560–569.

6. Wetter J, Belli E, Sinzobahamvya N, Blaschzok HC, Brecher AM, Urban AE. Transposition of the great arteries associated with ventricular septal defect: surgical results and long-term outcome. Eur J Cardiothorac Surg. 2001. 20:816–823.

7. DeLeon SY, Ilbawi MN, Arcilla RA, Thilenius OG, Quinones JA, Duffy EC, Sulayman RF. Transatrial relief of diffuse subaortic stenosis after ventricular septal defect closure. Ann Thorac Surg. 1990. 49:429–434.

8. Jahangiri M, Nicholson IA, del Nido PJ, Mayer JE, Jonas RA. Surgical management of complex and tunnel-like subaortic stenosis. Eur J Cardiothorac Surg. 2000. 17:637–642.

9. Kalfa D, Ghez O, Kreitmann B, Metras D. Secondary subaortic stenosis in heart defects without any initial subaortic obstruction: a multifactorial postoperative event. Eur J Cardiothorac Surg. 2007. 32:582–587.

10. Barbero-Marcial M, Tanamati C, Atik E, Ebaid M. Intraventricular repair of double-outlet right ventricle with noncommitted ventricular septal defect: advantages of multiple patches. J Thorac Cardiovasc Surg. 1999. 118:1056–1067.

11. Belli E, Serraf A, Lacour-Gayet F, Inamo J, Houyel L, Planche C. Surgical treatment of subaortic stenosis after biventricular repair of double-outlet right ventricle. J Thorac Cardiovasc Surg. 1996. 112:1570–1580.

12. Lacour-Gayet F. Biventricular repair of double outlet right ventricle with noncommitted ventricular septal defect. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2002. 5:163–172.

13. Luber JM, Castaneda AR, Lang P, Norwood WI. Repair of double-outlet right ventricle: early and late results. Circulation. 1983. 68(3 pt 2):II144–II147.
14. Kirklin JW, Pacifico AD, Blackstone EH, Kirklin JK, Bargeron LM Jr. Current risks and protocols for operations for double-outlet right ventricle. Derivation from an 18 year experience. J Thorac Cardiovasc Surg. 1986. 92:913–930.
15. Rocchini AP, Rosenthal A, Castaneda AR, Keane JF, Jeresaty R. Subaortic obstruction after the use of an intracardiac baffle to tunnel the left ventricle to the aorta. Circulation. 1976. 54:957–960.

16. Rychik J, Jacobs ML, Norwood WI. Early changes in ventricular geometry and ventricular septal defect size following Rastelli operation or intraventricular baffle repair for conotruncal anomaly. A cause for development of subaortic stenosis. Circulation. 1994. 90(5 Pt 2):II13–II19.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download