Abstract
Human metapneumovirus (HMPV) shares clinical and epidemiological characteristics with well-known respiratory syncytial virus (RSV). The aim of this study was to investigate the clinical and epidemiological differences between HMPV- and RSV-induced wheezing illnesses. A total of 1,008 nasopharyngeal aspirate specimens was collected from 1,008 pediatric patients hospitalized with acute respiratory tract infection at Inje University Sanggye Paik Hospital from December 2003 to April 2008, and tested for seven common respiratory viruses. Conditions classified as wheezing illness were bronchiolitis, reactive airways disease, and bronchial asthma. HMPV caused a significantly lower proportion of wheezing illness when compared to RSV (48.1% vs. 82.2%, P<0.05). HMPV-induced wheezing illness occurred predominantly in older patients when compared to RSV patients (P<0.001). RSV infections peaked in the fall and winter followed by peaks of HMPV infection in winter and spring. Eosinophil counts were significantly higher (P<0.01) in RSV patients when compared to HMPV patients. These results show that human metapneumovirus patients exhibit several different clinical and epidemiological characteristics, such as higher proportion of wheezing illness, age and seasonal incidence, and eosinophil counts, when compared to RSV patients.
Human metapneumovirus (HMPV), a recently discovered member of the family Paramyxoviridae, has been isolated from the respiratory secretions of patients worldwide (1-4). Though not as common as respiratory syncytial virus (RSV), it is a frequent etiologic agent of both upper and lower respiratory tract infections. Evidence suggests that this virus has been circulating for over 50 yr and most individuals have been exposed to it by the age of 5 (5). However, the epidemiological picture of HMPV infections in Korean children remains unclear.
RSV is a common cause of respiratory illness in children, and is considered the most important cause of viral bronchiolitis in young children (6). Several studies have shown clinical manifestations of HMPV and RSV infections to be very similar, and range from mild respiratory problems to bronchiolitis, pneumonia, severe cough, high fever, and myalgia; consequently, they are difficult to distinguish clinically (5, 7). RSV is known as a major causative agent of acute wheezing in children, and RSV bronchiolitis in early childhood is strongly associated with asthma development later in life (8). Several research groups have reported HMPV is also an etiologic agent of wheezing illness in children and adults (9-12), though there have been contradictory results (13).
RSV and HMPV share genomic (14) and seasonal distribution (15, 16) patterns, as well. Both viruses circulate in the winter and spring months with recurrent epidemics occurring in the winter. Studies have also shown that HMPV causes persistent infections, as does RSV, due to these viruses eliciting only a partially protective immune response (17). Because of their clinical, genetic, and epidemiological homogeneity, it has been suggested they also share similar replicative, pathophysiologic, and immunologic functions (14). To date this question remains unanswered.
In our previous report, HMPV was found to be prevalent in Korean children ≤5 yr hospitalized with acute wheezing illness from February to November 2006 (12). This study investigated the relative contribution of HMPV to the hospitalization of children for acute wheezing illness and to further elucidate the clinical and epidemiological differences of HMPV infection in relation to RSV infection from December 2003 to April 2008.
A total of 1,008 nasopharyngeal aspirate (NPA) specimens were collected from 1,008 pediatric patients hospitalized with acute respiratory tract infection wheezing illness at Inje University Sanggye Paik Hospital from December 2003 to April 2008. For this study, three different diagnoses were classified as wheezing illness: bronchiolitis, reactive airways disease (RAD) and bronchial asthma. Acute bronchiolitis was defined as a first occurrence of expiratory wheezing with or without tachypnea, air trapping, and substernal retraction in children <3 yr of age. RAD was defined as recurrent wheezing <3 times, and bronchial asthma was defined as recurrent wheezing ≥3 times in any child (18). Informed consent was given before any specimens were taken and the study protocol was approved by the Ethics Committee of Inje University Sang-gye Paik Hospital (IRB # IJ 06-34).
On admission, 2 mL of normal saline were instilled into the nostril and then aspirated using a disposable catheter and suction device. NPAs were centrifuged and the supernatants were stored at -70℃ until tested.
From December 2003 to December 2006, common respiratory viruses (Adenovirus, RSV, Influenza A and B, and Parainfluenza viruses 1-3) were detected by immunofluorescent-antibody test (IFA) (DAKO, Cambridgeshire, UK), while HMPV was detected using multiplex reverse transcriptasepolymerase chain reaction (RT-PCR), as previously described (12). From January 2007 to the end of the study period, RT-PCR was used to test all respiratory viruses investigated, including Rhinovirus (RV).
From December 2003 to April 2008, 1,008 nasopharyngeal aspirates were taken from pediatric patients hospitalized for acute respiratory tract infection and tested for six common viruses (RSV, parainfluenza, HMPV, adenovirus, and influenza A and B). RV was tested for from January 2007 to April 2008.
From the above study group, HMPV had an overall prevalence of 7.2% (73/1,008) while prevalence of RSV was 26.0% (262/1,008).
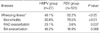
The average age of first infection in the HMPV and RSV groups are shown in Table 1. Virus-positive patients hospitalized with acute respiratory tract infection had an average age of 20.2±21.0 months (range, 1-150 months). The most commonly detected virus was RSV (25.5%) followed by parainfluenza (13.6%), RV (7.3%), HMPV (6.8%), adenovirus (6.5%), and influenza (4.8%).
Eosinophil and neutrophil counts are shown in Table 1. RSV patients had significantly higher (P=0.002) eosinophil counts than HMPV patients; however, there was no significant difference in neutrophil counts.
Of these virus-positive cases, 48.1% of HMPV-infected and 82.2% of RSV-infected patients were diagnosed with wheezing illnesses (P<0.05) (Table 2). RSV caused a significantly higher (P<0.01) proportion of bronchiolitis than HMPV.
All patients positive for HMPV or RSV and hospitalized for wheezing illness at our hospital were divided into three age groups: <12 months, 13-36 months, and >37 months. In the 13-36 months range, the proportion of HMPV cases was significantly greater (P<0.05) than the proportion of RSV cases, while the opposite was true in children <12 months (P<0.05). In children >37 months, the proportions of HMPV and RSV were nearly the same.
The study population investigated for seasonal incidence consisted of 1,008 children cared for at our hospital from December 2003 to April 2008 (Fig. 1). RSV infection occurred predominantly in the fall and winter and usually followed by peaks of HMPV infection in winter and spring.
The co-infection rate in the HMPV group was much higher when compared to the RSV group (25.9% vs. 5.9%). Among HMPV patients co-infected with other respiratory viruses, parainfluenza was the most common (42.9%) followed by RV (28.6%) and adenovirus (28.6%). Among RSV patients co-infected with other respiratory viruses, adenovirus was the most common (66.7%) followed by parainfluenza (16.7%) and RV (16.7%).
To date this is the most comprehensive comparison of HMPV- and RSV-induced wheezing illness and the first report of its kind in Korea. Our results demonstrated HMPV wheezing illnesses exhibited several clinical and epidemiological differences (i.e., proportion of wheezing illness, age and seasonal distribution, and eosinophil counts) when compared to RSV wheezing illnesses. Both HMPV and RSV were prominent etiologic agents of wheezing illness. In our study, the proportions of respiratory HMPV and RSV infections manifesting as wheezing illness were quite substantial (48.1% and 82.2%, respectively). Several studies have shown a strong association between HMPV infection and wheezing illness (2, 10-12, 19), though one study contradicted these results (13). Another study in particular found HMPV bronchiolitis to be an important risk factor for asthma development in preschool years; in fact, the association was at least as strong as that found between RSV-bronchiolitis and asthma development (20). The proportional breakdown of wheezing illness manifestations in our HMPV and RSV patients differed from the few recent studies also comparing them. Bronchiolitis was a significantly more common diagnosis in RSV patients than in HMPV patients in our study (79.5% vs. 30.8%). Manoha et al. (21) found HMPV and RSV infection manifesting as bronchiolitis in nearly equal proportions, while asthma was a significantly more common diagnosis in pediatric inpatients and outpatients with HMPV. A different study also found bronchial asthma significantly more prevalent in HMPV patients (22), in contrast to our results. However, Garcia-Garcia et al. (16) and Kim et al. (23) studies concur with our findings that RSV is a significantly frequent cause of bronchiolitis. Garcia et al. also found HMPV a more frequent cause of recurrent wheezing. Their results, along with ours, are congruent with Kahn's review (24) of HMPV studies, which found this virus to be an important cause of wheezing illness in early childhood.
There were significant differences in age distribution between the HMPV and RSV patients in our study population. The mean age of patients with HMPV was significantly greater than the age of RSV patients. RSV infection occurred predominantly in infants (<12 months), while HMPV was found mainly in children 12-36 months. These results mirror those of others (23). Baer et al. (25) reported both a significantly greater median age of HMPV patients and similar proportions of HMPV and RSV infections in the <12 months age group (39% and 62%, respectively) compared to our study subgroup of the same age (29.6% and 63%, respectively). However, Williams et al. (26) found a younger median age in their HMPV patients compared to those with RSV-induced lower respiratory tract infection. In a study of Danish children, hospitalization for acute respiratory tract infection caused by HMPV occurred only in very young children (1-6 months) (22). Regardless of these different results, both HMPV and RSV predominate in infants and young children as major causes of severe respiratory illness (24). In our study, as age increased, HMPV became a more important agent of wheezing illnesses, such as RAD and bronchial asthma. This is an expected result, as very young children previously infected with RSV would have partial immunity to the virus allowing HMPV to become more dominant in older children.
Analysis of the seasonal incidence of these two virus infections in Korea (Fig. 1) showed that although both RSV and HMPV infections occur throughout the year, there is a general trend toward RSV occurring mainly in the fall and winter with HMPV infections following in the spring. Incomplete data for the spring of 2008 also demonstrate the predominance of HMPV in this season and no cases of RSV. An exception for HMPV was the winter season of 2004/2005, when this virus was more prevalent than RSV. Kim et al. (23) also reported a spring peak of HMPV and a fall/early winter peak of RSV infections in Korean children. Another study directly comparing the seasonality of RSV and HMPV found similar trends (21) except for the frequent autumnal occurrence of RSV in our study.
Elevated blood eosinophil counts in RSV bronchiolitis were an interesting finding, as eosinophilia has been associated with recurrent wheezing/asthma development later in life (27). In our study the RSV group displayed eosinophilia when compared to the HMPV group. Therefore, RSV-infected patients may have a greater chance of developing recurrent wheezing in the future than HMPV-infected patients. However, a more detailed study of their immunologic profiles, including cytokine and chemokine profiles, will need to be done to more accurately assess HMPV's perturbation of the immune system and to further compare the similarities and differences of these two respiratory viruses from immunologic and pathophysiologic perspectives.
The rate of co-infection in the HMPV group was much higher when compared to the RSV group (25.9% vs. 5.9%). The co-infecting viruses were the same for both groups: parainfluenza, RV and adenovirus. The overlapping seasonal distributions (26), tendency to occur in the same patient population (infants and young children), and similar degree of pathogenicity (28) of these two common viruses may help explain why co-infections have been found in several other studies; however, there were no cases of HMPV and RSV co-infection in our study. The higher rate of co-infection in the HMPV group (25.9%) may also be due to the viral detection methods used in this study: i.e., multiplex RT-PCR for HMPV, and IFA for all other viruses (with the exception of RV) from December 2003 to December 2006, and RT-PCR for all viruses, thereafter, until the study endpoint. In general, RT-PCR is a more sensitive test than IFA for detection of viruses (29), which may result in more HMPV infections detected. There are also conflicting results regarding whether disease severity is associated with co-infection (24). More studies are needed to answer this question.
A weakness of this study was the fact that only patients with infections severe enough to be hospitalized were included. Therefore, the prevalence of HMPV- and RSV-induced wheezing illness in our study population may underestimate their respective prevalence in the community. Furthermore, the location of our tertiary care facility is unique in that it is one of the most densely populated neighborhoods in Korea. The correlation between degree of crowding and incidence and severity of lower respiratory tract infection has been demonstrated (30). Thus, our results cannot be extrapolated to the entire population of Korean children. As previously mentioned, another weakness was the different viral detection methods used for HMPV versus the other viruses investigated.
The clinical relevance of this study is the etiologic determination of wheezing illness in our study population. From this point, a longitudinal study is needed to investigate patients who develop recurrent wheezing and/or asthma. In that way, association between HMPV and/or RSV infection in early childhood and later asthma development could be deduced.
To summarize, our data reveals, first, that HMPV is an important cause of wheezing illness, though the prevalence of wheezing illness in RSV-infected patients was notably higher than the corresponding prevalence in HMPV-infected patients. Second, age distribution analysis showed RSV infections occurred in significantly younger patients. Third, seasonal incidence for the two viruses were also different, though with some overlapping: RSV infections occurred predominantly in the winter, while HMPV infections in the spring. Peak incidence of RSV infection was followed by peak HMPV infection. Fourth, RSV-infected patients exhibited significantly higher eosinophil counts without significant difference in neutrophil counts.
In conclusion, HMPV is an important cause of wheezing illness in infants and young children in Korea. Comparing HMPV and RSV reveals many epidemiological and clinical differences, but many questions remain unanswered. A long-term study should be conducted to determine whether early childhood infection with this virus leads to recurrent wheezing and/or asthma. The next point of comparison should involve the study of their pathophysiology and immunologic profiles to determine how HMPV induces wheezing illness.
Figures and Tables
Fig. 1
Seasonal incidence of HMPV and RSV infection was plotted from December 2003 to April 2008. The Y-axis represents the proportion of the total number of patients with a wheezing illness positive for that respiratory virus.
*proportion of all virus-positive samples.

References
1. Peret TC, Boivin G, Li Y, Couillard M, Humphrey C, Osterhaus AD, Erdman DD, Anderson LJ. Characterization of human metapneumoviruses isolated from patients in North America. J Infect Dis. 2002. 185:1660–1663.

2. Jartti T, van den Hoogen B, Garofalo RP, Osterhaus AD, Ruuskanen O. Metapneumovirus and acute wheezing in children. Lancet. 2002. 360:1393–1394.

3. Chung JY, Han TH, Kim BE, Kim CK, Kim SW, Hwang ES. Human metapneumovirus infection in hospitalized children with acute respiratory disease in Korea. J Korean Med Sci. 2006. 21:838–842.

4. Madhi SA, Ludewick H, Abed Y, Klugman KP, Boivin G. Human metapneumovirus-associated lower respiratory tract infections among hospitalized human immunodeficiency virus type 1 (HIV-1)-infected and HIV-1-uninfected African infants. Clin Infect Dis. 2003. 37:1705–1710.

5. van den Hoogen BG, de Jong JC, Groen J, Kuiken T, de Groot R, Fouchier RA, Osterhaus AD. A newly discovered human pneumovirus isolated from young children with respiratory tract disease. Nat Med. 2001. 7:719–724.

6. Glezen P, Denny FW. Epidemiology of acute lower respiratory disease in children. N Engl J Med. 1973. 288:498–505.

7. Boivin G, Abed Y, Pelletier G, Ruel L, Moisan D, Cote S, Peret TC, Erdman DD, Anderson LJ. Virological features and clinical manifestations associated with human metapneumovirus: a new paramyxovirus responsible for acute respiratory tract infections in all age groups. J Infect Dis. 2002. 186:1330–1334.
8. Sigurs N, Bjarnason R, Sigurbergsson F, Kjellman B. Respiratory syncytial virus bronchiolitis in infancy is an important risk factor for asthma and allergy at age 7. Am J Respir Crit Care Med. 2000. 161:1501–1507.

9. Jartti T, Lehtinen P, Vuorinen T, Osterback R, van den Hoogen B, Osterhaus AD, Ruuskanen O. Respiratory picornaviruses and respiratory syncytial virus as causative agents of acute expiratory wheezing in children. Emerg Infect Dis. 2004. 10:1095–1101.

10. Williams JV, Tollefson SJ, Heymann PW, Carper HT, Patrie J, Crowe JE. Human metapneumovirus infection in children hospitalized for wheezing. J Allergy Clin Immunol. 2005. 115:1311–1312.

11. Freymouth F, Vabret A, Legrand L, Eterradossi N, Lafay-Delaire F, Brouard J, Guillois B. Presence of the new human metapneumovirus in French children with bronchiolitis. Pediatr Infect Dis J. 2003. 22:92–94.
12. Chung JY, Han TH, Kim SW, Kim CK, Hwang ES. Detection of viruses identified recently in children with acute wheezing. J Med Virol. 2007. 79:1238–1243.

13. Rawlinson WD, Waliuzzaman Z, Carter IW, Belessis YC, Gilbert KM, Morton JR. Asthma exacerbations in children associated with rhinovirus but not human metapneumovirus infection. J Infect Dis. 2003. 187:1314–1318.

14. Mahalingam S, Schwarze J, Zaid A, Nissen M, Sloots T, Tauro S, Storer J, Alvarez R. Perspective on the host response to human metapneumovirus infection: what can we learn from respiratory syncytial virus infections? Microbes Infect. 2006. 8:285–293.

15. van den Hoogen BG, Osterhaus DM, Fouchier RA. Clinical impact and diagnosis of human metapneumovirus infection. Pediatr Infect Dis J. 2004. 23:Suppl 1. S25–S32.

16. Garcia-Garcia ML, Calvo C, Perez-Brena P, De Cea JM, Acosta B, Casas I. Prevalence and clinical characteristics of human metapneumovirus infections in hospitalized infants in Spain. Pediatr Pulmonol. 2006. 41:863–871.
17. Crowe JE Jr, Williams JV. Immunology of viral respiratory tract infection in infancy. Paediatr Respir Rev. 2003. 4:112–119.

18. Mertsola J, Ziegler T, Ruuskanen O, Vanto T, Koivikko A, Halonen P. Recurrent wheezy bronchitis and respiratory infections. Arch Dis Child. 1991. 66:124–129.
19. Esper F, Boucher D, Weibel C, Martinello RA, Kahn JS. Human metapneumovirus infection in the United States: clinical manifestations associated with a newly emerging respiratory infection in children. Pediatrics. 2003. 111:1407–1410.

20. Garcia-Garcia ML, Calvo C, Casas I, Bracamonte T, Rellan A, Gozalo F, Tenorio T, Perez-Brena P. Human metapneumovirus bronchiolitis in infancy is an important risk factor for asthma at age 5. Pediatr Pulmonol. 2007. 42:458–464.
21. Manoha C, Espinosa S, Aho SL, Huet F, Pothier P. Epidemiological and clinical features of hMPV, RSV and RVs infections in young children. J Clin Virol. 2007. 38:221–226.

22. von Linstow ML, Larsen HH, Eugen-Olsen J, Koch A, Nordmann Winther T, Meyer AM, Westh H, Lundgren B, Melbye M, Hogh B. Human metapneumovirus and respiratory syncytial virus in hospitalized Danish children with acute respiratory tract infection. Scand J Infect Dis. 2004. 36:578–584.
23. Kim YK, Kim JW, Wee YS, Yoo EG, Han MY. Clinical features of Human [Metapneumovirus and Respiratory Syncytial Virus infection in hospitalized children.]. Pediatr Allergy Respir Dis. 2009. 19:12–19.
25. Baer G, Schaad UB, Heininger U. Clinical findings and unusual epidemiologic characteristics of human metapneumovirus infections in children in the region of Basel, Switzerland. Eur J Pediatr. 2008. 167:63–69.

26. Williams JV, Harris PA, Tollefson SJ, Halburnt-Rush LL, Pingsterhaus JM, Edwards KM, Wright PF, Crowe JE Jr. Human metapneumovirus and lower respiratory tract disease in otherwise healthy infants and children. N Engl J Med. 2004. 350:443–450.

27. Ehlenfield DR, Cameron K, Welliver RC. Eosinophilia at the time of respiratory syncytial virus bronchiolitis predicts childhood reactive airway disease. Pediatrics. 2000. 105:79–83.

28. Gerna G, Campanini G, Rovida F, Sarasini A, Lilleri D, Paolucci S, Marchi A, Baldanti F, Revello MG. Changing circulation rate of human metapneumovirus strains and types among hospitalized pediatric patients during three consecutive winter-spring seasons. Brief report. Arch Virol. 2005. 150:2365–2375.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download