Abstract
Hypersensitivity to mosquito bites (HMB) is a disorder characterized by a necrotic skin reaction and generalized symptoms subsequent to mosquito bites. It has been suggested that HMB is associated with chronic Epstein-Barr virus (EBV) infection and natural killer cell leukemia/lymphoma. We describe here a Korean child who had HMB associated with chronic EBV infection and natural killer cell lymphocytosis. A 5-yr-old boy was suffered from necrotic skin lesions on the right ear lobe. Type A EB virus was detected from hlood cells and bone marrow biospy recognized hemophagocyrosis.
Hypersensitivity to a mosquito bites (HMB) is a disorder characterized by intense skin reaction and various generalized symptoms subsequent to mosquito bites (1). While this disorder is very rare, some cases of HMB mainly reported from East Asia, primarily from Japan (2). However, recently a 7-yr-old Latin American case was reported in 2005 (3). It has been suggested that HMB is associated with chronic Epstein-Barr virus (EBV) infection and natural killer (NK) cell leukemia/lymphoma (1, 4). We describe here a Korean child who had HMB associated with chronic EBV infection and NK cell lymphocytosis.
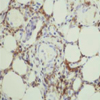
A 5-yr-old male was admitted with well-demarcated necrotic skin lesions and severe swelling on right ear lobe developed after mosquito bites (Fig. 1). In addition to cutaneous lesion, he also had a high temperature. He had suffered several similar symptoms since last summer, which complicated as deep scars on skin. Laboratory tests showed white blood cell (WBC) 7,280/µL (neutrophil 39%, lymphocyte 56%), total eosinophil count 156/µL, IgE by PRIST above 1,000 kIU/L. IgG, A, M levels were normal. Specific IgE for Aedes communis by radioallergosorbent test (RAST) was negative. To perform a skin patch test, we prepared salivary gland extracts from 2 mosquito species, including Aedes togoi (Ae. togoi) and Culex Pipiens (Cx. pipiens). These species were chosen because Ae. Togoi is prevalent throughout eastern Asia and Cx. pipiens is found worldwide (5), especially in Chungnam area of Korea. The protein concentration of the salivary gland extracts were as following; Ae. togoi, 0.079 mg/dL: Cx. pipiens, 0.523 mg/dL. The result of the skin patch tests showed a positive response to Cx. pipiens after 72 hr (Fig. 2). Lymphocyte subset analysis demonstrated increased NK cells (CD16+CD56, 43%) and decreased CD3 and CD4 cells. IgM for anti-nuclear antigen (EBNA), IgM for viral capsid antigen (VCA) and IgM for anti-early antigen (EA) DR to EBV were all negative. However, the levels of anti-VCA IgG (>200 U/mL), anti-EA DR IgG (>150 U/mL) and anti-EBNA IgG (62 U/mL) were increased: these findings are consistent with chronic EBV infection. Type A EB virus was demonstrated in blood mononuclear cells by DNA polymerase chain reaction (PCR) method (Fig. 3). EBER (EBV encoded RNA) in situ hybridization was negative in necrotic tissues. Immunostaining with NK-cell marker (CD56) revealed many immunoreactive cells with the perivascular inflammatory infiltrates in necrotic tissue (Fig. 4). The patient had a bone marrow biopsy performed, and was diagnosed with the hemophagocytic syndrome 2 yr and 6 months after the first symptom appeared. During the immunosuppressive therapy, the patient had four additional episodes of mosquito bites, each of which gave rise to intense local skin reactions as well as a high fever.
HMB was first described in 1938 in a patient from Florida, USA (6). In 1990, Tokura et al. described a patient with HMB in whom 50% to 60% of the peripheral blood mononuclear cells were large granular lymphocytes that were identified phenotypically and functionally as NK cells (4). On the other hand, HMB is seen in a considerable number of patients with chronic active EBV infection (7). Finally, accumulated clinical and laboratory studies have concluded that HMB occurs in close association with NK cell disease where the cells are infected with monoclonal EBV (1). This entity referred to as "mosquito allergy" historically (2), is now referred to as "HMB-EBV-NK disease" (1).
HMB-EBV-NK disease is a very rare. A Korean adolescent who had HMB-EBV-NK disease was reported in 2003 (8). The mean age of onset is 6.7 yr and there is no gender predominance (1). The pathophysiological relationship between HMB, EBV infection, and NK cell neoplasms remains unclear. Tokura et al. (1) demonstrated that EBV infection immortalizes NK cells, which are activated by injection of some mosquito constituents, thereby exhibiting HMB as the primary clinical manifestation. In addition, he reported that NK cell predominant mononuclear cells are infiltrated into mosquito bite sites. The accumulation of NK cells may directly or indirectly mediate the systemic symptoms, and a recurrent and prolonged activated state of NK cells may induce additional genetic damage that leads to the development of leukemias or lymphomas (9).
The typical clinical course of patients with HMB-EBV-NK disease includes three clinical stages. Initailly, an exaggerated reaction to mosquito bites is identified. Older patients may exhibit several episodes with deterioration of general systemic symptoms. Some patients may already have leukemia or lymphoma when the first episode of HMB is diagnosed (1). The hemophagocytic syndrome is one of the major life-threatening complications that occur at the terminal stages (1). Most of the reported cases of HMB have shown a close relationship between mosquito allergy and EBV-infected NK-cell lymphoproliferation. Further investigation of hypersensitivity to mosquito bite pathogenesis, and the relationship between EBV infection and subsequent oncogenesis of NK cell lymphoma/leukemia including chronic NK cell lymphocytosis, is needed.
Figures and Tables
Fig. 1
(A) The skin lesion that developed after mosquito bites on the right ear. (B) Necrotic change of the lesion on the right ear on the sixth hospital day.

Fig. 2
(A) The skin patch test for the mosquito allergens Lt, Aedes togoi; Rt, Culex pipiens. (B) The skin patch test shows a positive reaction to Culex pipiens (Rt) and a negative reaction to Aedes togoi (Lt).

References
1. Tokura Y, Ishihara S, Tagawa S, Seo N, Ohshima K, Takigawa M. Hypersensitivity to mosquito bites as the primary clinical manifestation of a juvenile type of Epstein-Barr virus associated natural killer cell leukemia/lymphoma. J Am Acad Dermatol. 2001. 45:569–578.
2. Suzuki S, Negishi K, Tomizawa S, Shibasaki M, Kurome T. A case of mosquito allergy. Immunological studies. Acta Allergol. 1976. 31:428–441.

3. Pacheco SE, Gottschalk SM, Gresik MV, Dishop MK, Okmaura T, McCormick TG. Chronic active Epstein-Barr virus infection of natural killer cells presenting as severe skin reaction to mosquito bites. J Allergy Clin Immunol. 2005. 116:470–472.

4. Tokura Y, Tamura Y, Takigawa M, Koide M, Satoh T, Sakamoto T, Horiguchi D, Yamada M. Severe hypersensitivity to mosquito bites associated with natural killer cell lymphocytosis. Arch Dermatol. 1990. 126:362–368.

5. Knight KL, Stone A. A catalog of the mosquitoes of the world. 1977. 2nd ed. Washington: Ent Soc Am (Thomas Say Found);611.
6. Brown A, Griffitts TH, Erwin S, Dyrenforth LY. Arthus' phenomenon from mosquito bites: report of a case with experimental studies. South Med J. 1938. 31:590–596.
7. Ishihara S, Okada S, Wakiguchi H, Kurashige T, Morishima T, Kawa-Ha K. Chronic active Epstein-Barr virus infection in children in Japan. Acta Paediatr. 1995. 84:1271–1275.

8. Park SY, Cho YS, Kim HH, Lee CK, Yoo B, Kim SW, Oh HB, Park CJ, Moon HB. A case of hypersensitivity to mosquito bites with chronic Epstein-Barr virus infection and atypical lymphocytosis. J Asthma Allergy Clin Immunol. 2003. 23:408–413.
9. Tsuge I, Morishima T, Morita M, Kimura H, Kuzushima K, Matsuoka H. Characterization of Epstein-Barr virus infected natural killer cell proliferation in patients with severe mosquito allergy: establishment of an IL-2-dependent NK-like cell line. Clin Exp Immunol. 1999. 115:385–392.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download