Abstract
We performed a prospective, randomized, and double-blind study comparing the top-up effects of 2% lidocaine/100 µg fentanyl/epinephrine (n=31) and 2% lidocaine/saline/epinephrine (n=30) when extending an epidural labor analgesia using low-dose ropivacaine and fentanyl. Survival analysis for the sensory blocks to the T4 level showed no statistically significant differences in onset time to T4 between the 2 groups. Onset times (min) to T4-sensory blocks for cold and pinprick were not different between the two groups. However, median maximum sensory level in the lidocaine-fentanyl group (T1 for cold and T2 for pinprick) was significantly higher than that in the lidocaine-saline group (T3 and T4, respectively). The lidocaine-fentanyl group exhibited less visceral pain (6.5% vs. 36.7%), less supplementation of lidocaine (6.5% vs. 43.3%), and less nausea (6.5% vs. 26.7%) compared with the lidocaine-saline group during the intraoperative period. It is concluded that adding fentanyl to 2% lidocaine does not speed up the onset of the block when the onset is tested with cold or sharp pinprick but improves the quality of analgesia with fewer side effects in emergency top-up for cesarean section.
If a woman receiving epidural labor analgesia requires a cesarean section, the anesthesiologist should provide a block of good quality as quickly as possible. Although the coadministration of opioids to local anesthetics has gained popularity for speeding onset of block and improving quality of analgesia (1, 2), not all clinical studies support this technique particularly in obstetric anesthesia. Recently, several studies have demonstrated that if patients already received epidural fentanyl for labor, the addition of opioids in the top-up would neither accelerate the onset nor decrease the supplementation of analgesics (3-5). However, those studies compared different mixtures of local anesthetic agents for top-up, employed different definitions of surgical readiness, used insufficient analytical power, and had a sample population that was not well controlled, or had large variability in the onset times. Limited data are available on emergency cases, especially with epidural labor analgesia using continuous infusion of ropivacaine and fentanyl.
Our hypothesis was to verify that the addition of 100 µg fentanyl would increase the speed of conversion or maximum level of the block. We designed a prospective, radomized, and double-blind study to compare the efficacies of a 2% lidocaine/epinephrine with and without 100 µg fentanyl for converting continuous epidural labor analgesia containing fentanyl and ropivacaine into a block adequate for emergency cesarean section.
Ethical approval was obtained from the Institutional Review Board and the Hospital Research Ethics Committee (CGH-IRB-2009-48). Informed consents were obtained from all patients. Inclusion criteria for this study were as follows: suitable for cesarean section under epidural anesthesia, emergency cesarean categories III (needing early delivery but no maternal or fetal compromise) (6), and uncomplicated nullipara with singleton pregnancy. Exclusion criteria were as follows: multiple pregnancies, emergency cesarean delivery grade I (immediate threat to life of woman or fetus) or II (maternal or fetal compromise which is not immediately life-threatening) (6), failure of replacement of the epidural catheter, and a poorly functioning epidural catheter during the labor in parturient that did not have symptomatic improvement after bolus. The routine method used for epidural labor analgesia in our maternity unit is the administration of a bolus of 10 mL 0.1% ropivacaine with 50 µg fentanyl and a continuous infusion at a constant rate (10 mL/h) of 0.1% ropivacaine with 2 µg/mL fentanyl. An additional bolus of 5 mL 0.1% ropivacaine was supplemented when required.
The study was performed in prospective, randomized, and double-blind manner. Electrocardiography, pulse oximetry, and noninvasive blood pressure monitoring were commenced. Immediately before the top-up, the level of sensory (cold and pinprick) and motor (modified Bromage scale score: 0, can raise extended leg off bed; 1, can bend knees; 2, can bend ankles; 3, unable to bend knees or ankles) blocks were assessed. Patients in the lidocaine-fentanyl group (n=31) received the freshly prepared 20 mL of 2% lidocaine and 100 µg (2 mL) fentanyl with epinephrine (1:200,000) epidurally. Patients in the lidocaine-saline group (n=31) received 20 mL of 2% lidocaine and 2 mL of normal saline with epinephrine (1:200,000). The solution was injected via epidural catheter by an anesthesiologist blinded to the drug mixture. The speed of epidural top-up was consistent in the 2 groups over 5 min. Patients were assigned to groups using computer-generated random numbers.
If the block for pinprick was not at the T6 level within 20 min from the end of the injection, a 5 mL supplement of 2% lidocaine was given. Subsequently, if the sensory block for pinprick had not attained the T6 level at 30 min despite the supplement, the top-up was deemed to have failed and the anesthesiologist could remedy the situation by whatever means necessary. Fetal heart rate was noted at 5 min intervals to ensure no deterioration in the fetal well-being during the procedure.
The level of the anesthetic block was assessed using a blunt end of pin for the pinprick and a cotton swab doused with alcohol for cold sensation at 2.5-min intervals from administration of the study drug to out of placenta and at 5-min intervals thereafter. We compared the time taken to attain a T4-sensory block (onset time to T4), time to skin incision, time to delivery, maximum height of the block, and time to the end of surgery from the end of the first top-up. During the anesthesia and surgery, hypotension (systolic blood pressure less than 90 mmHg or more than a 20% decrease from baseline value) was treated with fluid infusion and incremental doses of ephedrine. All patients were asked several times about unpleasant feelings, pain, or both. Pain, squeezing, or any unpleasant feeling associated with exteriorization of the uterus or traction of peritoneum was defined as a visceral pain. Visceral pain was treated with 5 mL of epidural lidocaine, fentanyl 50 µg IV, or both at the discretion of the anesthesiologist. Intraoperative hemodynamics including blood pressure and heart rate at 5 min-intervals, requirements for epidural lidocaine supplementation during surgery, and characteristics of the neonate were recorded.
A visual analogue pain score (VAS, with end points labeled 0=no pain and 100=worst possible pain) was used to assess postoperative pain intensity at 0, 1, 3, 6, 12, 24, and 48 hr after surgery. Perioperative side effects such as nausea, vomiting, respiratory depression (<8/min), or shivering were observed and treated appropriately. Patient-controlled epidural analgesia using a 0.02% bupivacaine in saline and 0.1 mg/mL morphine mixture was provided to all patients postoperatively over 48 hr.
Sample size calculation was based on data published previously by Price et al. (7) who reported a mean±SD time from epidural injection of lidocaine with epinephrine to skin incision of 16.6±6.1. They consider the adequate block as a bilateral complete loss of cold sensation to the level of T6 and pain to T10. We thought that a one-third difference in the time required to an adequate block would be clinically important. We calculated that 28 patients per group were required with an alpha value of 0.05 and power of 80%. Thirty-one patients in each group were enrolled for protocol omissions. Data were compared using independent t-test, Mann-Whitney U-test, Fisher's exact test, or chi-square test. Kaplan-Meier survival curves were constructed for onset time to T4, and the differences between the 2 groups were analyzed. Linear regression was used to investigate the relationship between onset time and either the duration of epidural analgesia, dose of epidural fentanyl given during labor, or pre-existing sensory level before administering the top-up for cesarean section. A value of P<0.05 was taken to denote statistical significance.
Sixty-two patients were enrolled in this study and the indications for cesarean section were failure to progress in all patients. Three patients (2 in the lidocaine-fentanyl group and 1 in the lidocaine-saline group) required second top-ups due to insufficient sensory block. The 2 patients in the lidocaine-fentanyl group showed block level of T7 at 20 min after the first injection and reached to the block level of T6 after the second top-up. In the patient in the lidocaine-saline group, however, top-up resulted in an inadequate block (below T10) for cesarean section even after 30 min. She received general anesthesia with sevoflurane and was excluded from the analysis due to the failed block. All patients except 1 reached the level of sensory block to T4 finally. No patients complained of any neurological symptoms during or after epidural injection through the catheter.
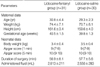
Maternal demographics and neonatal characteristics were similar in each group (Table 1). Details of the pre-existing epidural labor analgesia did not differ between the groups (Table 2).
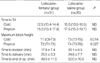
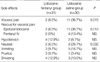
Survival analysis for the sensory blocks to the T4 level showed no statistically significant differences in onset time to T4 between the 2 groups, although the survival curves look some differences (Fig. 1). There were no statistically significant differences in times from the end of first top-up to skin incision and delivery (Table 3); however, the maximum levels of the sensory block were significantly higher in the lidocaine-fentanyl group than the lidocaine-saline group. In addition, a significantly more patients in the lidocaine-saline group complained of visceral pain and required supplementations compared to the patients in the lidocaine-fentanyl group (Table 4).
Changes in blood pressure and heart rate during surgery were not significantly different between the groups. Intraoperative nausea was more frequent in the lidocaine-saline group than the lidocaine-fentanyl group. The incidences of other side effects such as hypotension, vomiting, and shivering did not differ between the groups. No patients from either group exhibited respiratory depression. Postoperative VAS in the 2 groups was similar (Fig. 2).
Pooling data from the 2 groups, there was no significant relationship between onset time and duration of labor analgesia, dose of epidural fentanyl given during labor, or the pre-existing block levels before administering the top-up for cesarean section.
In the present study, we demonstrated that an addition of fentanyl to lidocaine and epinephrine did not accelerate the sensory block but increased maximum height of the block with minimized visceral pain when used to extend epidural analgesia containing fentanyl and ropivacaine during labor.
For elective cesarean section, many anesthesiologists have added a variety of opioids to the local anesthetic used in order to accelerate the onset, enhance the quality and prolong the duration of the blockade. One of the possible mechanisms of the fentanyl-induced acceleration of blocks is the property of blocking nerve conduction in spinal roots. Several electrophysiological studies have demonstrated that opioids inhibit the action potential of A and C fibres, and naloxone pretreatment does not prevent this inhibitory effect (8, 9). These suggested that fentanyl possesses the property of blocking nerve conduction that is not mediated via the opioid receptors. In our study, the fact that the administration of epidural fentanyl resulted in a higher maximum sensory level block compared to that induced by saline is most likely explained by the local anesthetic effect. There are also synergistic interactions between local anesthetics and opioids, although these drugs mostly exert their action independently via separate and distinct mechanisms with epidural administration. Alternatively, opioids interact with opioid receptors either pre- or post-synaptically to exert an inhibitory effect on neuronal transmission (10, 11). Therefore, the combination of local anesthetics and opioids may effectively inhibit multiple areas of neuronal excitability.
A possible explanation for the failure of fentanyl to speed up the onset in our results is that pre-existed epidural fentanyl during labor leads to a near-maximal effect such that further dosing produces no more benefits, unlike the elective case (1, 2). We found that 100 µg fentanyl was not effective, although it was a larger dose of fentanyl compared with the 50-75 µg that other authors gave in their clinical reports (5, 12, 13). The mean onset times for loss of cold and pain sensation in our results were 13.5 min and 15.7 min in the lidocaine-fentanyl group and 15.6 min and 18.9 min in the lidocaine-saline group, respectively. They were only powered to detect a 30% difference in onset times and were underpowered to detect 2-3 min as a statistically significant result. A faster onset is more important to avoid the need for general anesthesia for an urgent cesarean section, thus even a small time advantage of 2 or 3 min may be clinically valuable. Retrospective power analysis revealed that more than 200 patients would be required to have 80% power of detecting the difference we observed. Recently, a study was conducted by Balaji et al. (14). They showed a significantly faster onset (15.2 vs. 10.7 min) of block to T6 and fewer intraoperative supplements in the use of lidocaine-fentanyl-epinephrine compared to levobupivacaine 0.5%. However, their faster onset might be due to fentanyl or the different local anesthetics mixture.
We found that epidural fentanyl allows the top-up to increase the quality of the block; significantly more visceral pain was noted in the lidocaine-saline group than the lidocaine-fentanyl group. The most of visceral pains in our results were observed in spite of enough level of sensory loss. It suggested that cold and pinprick sensations might not be an appropriate method for assessing the surgical adequacy of the blocks although these are the most widely used methods in the anesthetic community. Recently published textbooks on obstetric anesthesia emphasize the importance of using a block to touch to assess regional bocks for cesarean section (15, 16), however, there is much controversy on the issue (17-19). In a report about the sensory assessment of epidural block for cesarean section, Camorcia et al. (20) observed a close correlation between the complete loss to pinprick sensation and the complete loss to light touch sensation, and thus they speculated that the complete loss of any sensation after pinprick stimulation might predict a painless surgery. Unmyelinated axons by which visceral pain is transmitted are blocked by a higher concentration of local anesthetics than myelinated axons, and an adequate level of blockade might not have been achieved for C-fibers even if the sensory blockade attained a sufficient level. In fact, even with T4 of sensory block, many mothers complain of unpleasant feelings associated with uterus manipulations. Opioids have been reported to depress the C fibers (21, 22). Spinal µ- and δ-opioid receptors also have a significant role in the modulation of visceral nociception (23). Although there was no clinical report about visceral pain in extending epidural analgesia, the numbers of need for extra intraoperative supplementation were not different between the groups with or without opioids (3, 5). This discrepancy may be attributed to differences in analgesic solution during labor, anesthetic protocols, and various methods of assessing visceral pain. Different surgical techniques could also explain the higher incidence of visceral pain in our study. At our hospital, surgeons prefer exteriorization of the uterus after delivery during cesarean section. In the recent National Institute for Clinical Excellence guidelines for cesarean section, however, exteriorization was not recommended because it is associated with more pain (24).
In the present study, it was unclear why the incidence of nausea was higher in the lidocaine-saline group than the lidocaine-fentanyl group. One possible explanation is visceral pain. Hirabayashi et al. reported that visceral pain was accompanied by nausea and vomiting (25). In agreement with their study, our results demonstrated that patients in the lidocaine-fentanyl group showed less visceral pain concomitant with a lower incidence of nausea than the lidocaine-saline group although we did not demonstrate the statistical correlation between them. In contrast, Malhotra and Yenti's demonstrated a higher incidence of nausea and vomiting in the fentanyl-levobupivacaine group than the saline-levobupivacaine group (53% vs. 18%) (5). It should be noted that in their results, there was a greater use of nitrous oxide in their fentanyl group. It is possible that nausea and vomiting were related to nitrous oxide rather than the quality of the blockade.
The failure rate of top-up in our study was 1.6%, which is relatively low compared with the rates reported in other studies. Price et al. (7) and Gaiser et al. (26) have reported 0% failure rates and others have reported 2.6-38% failure rates. Our results closely resemble those of Tortosa et al. (4). The wide range of failure rates might be explained by unspecified definitions of failure and different study protocols.
Because of the importance of extending labor epidural analgesia for emergency situations, we attempted to determine which factors might be associated with a more rapid onset of block to T4. We found that time to T4 was unrelated to the duration of the labor analgesia, dose of epidural fentanyl given during labor, or pre-existing sensory level before top-up. This suggests that we can not predict which patients will be ready for surgery quickly following a top-up. Further studies are needed.
Previous studies have shown that single injection (over 1-5 min) of 20 mL epidural bupivacaine 0.5% (27), lidocaine 2% with adrenalin (7), or a mixture (3) was safe. Although Price et al. reported blocks up to C7, there were no serious complications when this occurred (7). This is unlikely to happen if top-up is administered after a previously well-established epidural block (28). Occasionally, if the epidural catheter has been misplaced in the subdural space, a large top-up may lead to tearing of the arachnoid and an excessively high block (29). However, the pre-existing misplaced catheter usually permits early detection when evaluating the quality of the block during the labor. A limitation in the present study is that we did not compare time taken to prepare the solutions. However, mixing drugs in emergency situations may lead to errors (30) and the mixing itself may cause delays. The blinded nursing staff prepared the solution in the limited time available for delivery.
In conclusion, the addition of fentanyl to the lidocaine-epinephrine top-up offers no advantage with respect to speed of onset when the onset is tested with cold or sharp pinprick but it improves the quality of the anesthesia when existing epidural analgesia is extended for emergency cesarean section.
Figures and Tables
Fig. 1
(A) Kaplan-Meier survival curves for sensory block of cold and pinprick to T4 following the epidural top-ups with lidocaine 2%-fentanyl 100 µg-epinephrine 1:200,000 (lidocaine-fentanyl group) or lidocaine 2%-normal saline 2 mL-epinephrine (lidocaine-saline group). (B) Range (whiskers), interquartile range (boxes), median (thin vertical bars), and mean (thick vertical bars) for sensory block of cold and pinprick to T4. There are no statistical differences in onset time to T4 for cold sensation (P=0.102) and pinprick (P=0.053) between the 2 groups.

Fig. 2
Postoperative pain scores (VAS) during 48 hr were similar. Data are shown in box plot with ranges (whiskers), interquatile ranges (boxes), median (solid line), and mean (bold line). Lidocaine-fentanyl group, epidural top-up with lidocaine 2%-fentanyl 100 µg-epinephrine 1:200,000; lidocaine-saline group, epidural top-up with lidocaine 2%-normal saline 2 mL-epinephrine 1:200,000.

References
1. Curatolo M, Orlando A, Zbinden AM, Scaramozzino P, Venuti FS. A multifactorial analysis of the spread of epidural analgesia. Acta Anaesthesiol Scand. 1994. 38:646–652.

2. Cherng CH, Wong CS, Ho ST. Epidural fentanyl speeds the onset of sensory block during epidural lidocaine anesthesia. Reg Anesth Pain Med. 2001. 26:523–526.

3. Goring-Morris J, Russell IF. A randomised comparison of 0.5% bupivacaine with a lidocaine/epinephrine/fentanyl mixture for epidural top-up for emergency caesarean section after "low dose" epidural for labour. Int J Obstet Anesth. 2006. 15:109–114.

4. Tortosa JC, Parry NS, Mercier FJ, Mazoit JX, Benhamou D. Efficacy of augmentation of epidural analgesia for Caesarean section. Br J Anaesth. 2003. 91:532–535.

5. Malhotra S, Yentis SM. Extending low-dose epidural analgesia in labour for emergency Caesarean section-a comparison of levobupivacaine with or without fentanyl. Anaesthesia. 2007. 62:667–671.
6. Lucas DN, Yentis SM, Kinsella SM, Holdcroft A, May AE, Wee M, Robinson PN. Urgency of caesarean section: a new classification. J R Soc Med. 2000. 93:346–350.

7. Price ML, Reynolds F, Morgan BM. Extending epidural blockade for emergency caesarean section. Evaluation of 2% lignocaine with adrenaline. Int J Obstet Anesth. 1991. 1:13–18.

8. Gissen AJ, Gugino LD, Datta S, Miller J, Covino BG. Effects of fentanyl and sufentanil on peripheral mammalian nerves. Anesth Analg. 1987. 66:1272–1276.

9. Power I, Brown DT, Wildsmith JA. The effect of fentanyl, meperidine and diamorphine on nerve conduction in vitro. Reg Anesth. 1991. 16:204–208.
10. North RA, Williams JT. On the potassium conductance increased by opioids in rat locus coeruleus neurons. J Physiol. 1985. 364:265–280.
13. Lam DT, Kee WD, Khaw KS. Extension of epidural blockade in labour for emergency Caesarean section using 2% lidocaine with epinephrine and fentanyl, with or without alkalinisation. Anaesthesia. 2001. 56:790–794.

14. Balaji P, Dhillon P, Russell IF. Low-dose epidural top up for emergency caesarean delivery: a rahdomised comparison of levobupivacaine versus lidocaine/epinephrine/fentanyl. Int J Obstet Anesth. 2009. 18:335–341.
15. Holdcroft A, Thomas TA. Principles and Practice of Obstetric Anaesthesia. 2000. Oxford: Blackwell;261.
16. Yentis SM, Brighous D, May A, Bogod D, Elton C. Analgesia and Anaesthesia in Pregnancy. A practical guide. 2001. London: WB Saunders;92.
17. Dahlgren G. At caesarean section under regional anaesthesia, it is essential to test sensory block with light touch before allowing surgery to start. Int J Obstet Anesth. 2006. 15:298–300.

18. Collier C. Is testing touch sensation really necessary before cesarean section? Int J Obstet Anesth. 2005. 14:82–83.
19. Dhileepan S. Assessing regional blocks before Caesarean section. Int J Obstet Anesth. 2007. 16:192.

20. Camorcia M, Capogna G. Sensory assessment of epidural block for Caesarean section: a systematic comparison of pinprick, cold and touch sensation. Eur J Anaesthesiol. 2006. 23:611–617.
21. Dallel R, Duale C, Molat JL. Morphine administered in the substantia gelatinosa of the spinal trigeminal nucleus caudalis inhibits nociceptive activities in the spinal trigeminal nucleus oralis. J Neurosci. 1998. 18:3529–3536.

22. Ma D, Sapsed-Byrne SM, Chakrabarti MK, Ridout D, Whitwam JG. Synergism between sevoflurane and intravenous fentanyl on A delta and C somatosympathetic reflexes in dogs. Anesth Analg. 1998. 87:211–216.

23. Harada Y, Nishioka K, Kitahata LM, Nakatani K, Collins JG. Contrasting actions of intrathecal U50, 488H, morphine, or [D-Pen2, D-Pen5] enkephalin or intravenous U50, 488H on the visceromotor response to colorectal distension in the rat. Anesthesiology. 1995. 83:336–343.
24. Wee MY, Brown H, Reynolds F. The National Institute of Clinical Excellence Guidelines for Caesarean Sections: implications for the anaesthetist. Int J Obstet Anesth. 2005. 14:147–158.
25. Hirabayashi Y, Saitoh K, Fukuda H, Shimizu R. Visceral pain during caesarean section: effect of varying dose of spinal amethocaine. Br J Anaesth. 1995. 75:266–268.

26. Gaiser RR, Cheek TG, Gutsche BB. Epidural lidocaine versus 2-chloroprocaine for fetal distress requiring urgent cesarean section. Int J Obstet Anesth. 1994. 3:208–210.

27. Laishley RS, Morgan BM, Reynolds F. Effect of adrenaline on extradural anaesthesia and plasma concentrations during caesarean section. Br J Anaesth. 1988. 60:180–186.
28. Morgan B. Unexpectedly extensive conduction blocks in obstetric epidural analgesia. Anaesthesia. 1990. 45:148–152.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download