Abstract
In patients undergoing major orthopedic surgery, data of deep venous thrombosis (DVT) and pulmonary embolism (PE) are lacking as studied by computed tomographic (CT) pulmonary angiography and indirect CT venography (CTPA-CTV). A prospective observational study was performed for 363 Korean patients undergoing major orthopedic surgery to determine the incidence of venous thromboembolism (VTE), especially proximal DVT and PE. The incidence of VTE was 16.3% (n=59). Of them, 8 patients (2.2%) were symptomatic. The rate of VTE was the highest in patients who underwent total knee replacement (40.4%), followed by hip fracture surgery (16.4%), and total hip replacement (8.7%; P<0.001). The incidence of PE was 6.6% (n=24). Of them, 4 patients (1.1%) were symptomatic. Forty-one patients (11.3%) were in the proximal DVT or PE group. Based on multivariate analysis, total knee replacement and age ≥65 yr were significant risk factors for proximal DVT or PE in patients undergoing major orthopedic surgery (odds ratio [OR], 2.4; 95% confidence interval [CI], 1.1-5.1; P=0.025; and OR, 2.1; 95% CI, 1.0-4.4; P=0.046, respectively). Taken together, the overall incidence of PE was 6.6% and rate of symptomatic PE rate was 1.1%. Knee joint replacement and age ≥65 yr were significant risk factors for proximal DVT or PE.
Although venous thromboembolism (VTE) is a major public health issue in Western countries (1), it has traditionally been thought to be rare in Asian population. Therefore, pharmacologic thromboprophylaxis is not routinely given to Asian patients undergoing major orthopedic surgery of the lower limbs, which is considered as one of the high risk groups for VTE in the Western population (2). According to recently published epidemiologic data (1, 3, 4), the incidences of symptomatic and venographic deep venous thromboses (DVT) after major orthopedic surgery are not as low in Asian patients as once thought and in fact, approach the rates are similar with those observed in Western countries.
Because epidemiologic studies regarding postoperative DVT have been done using conventional contrast venography or ultrasonography, the incidence of pulmonary embolism (PE) is therefore less certain (2). This results from the fact that the diagnosis of PE is mainly based on perfusionventilation lung scanning in these studies (5-7). Advances in computed tomography (CT) technology, such as multi-detector row CT (MDCT), have improved the diagnosis of PE, replacing lung scanning as the most frequently used imaging tool for PE (8). Furthermore, addition of indirect venography during CT pulmonary angiography has improved the diagnosis of DVT in patients with suspected PE (9), facilitating the determination of the incidence of DVT along with PE. At present, CT venography is known to have a similar sensitivity and specificity as sonography in diagnosing proximal DVT of the lower extremities in patients with suspected PE (10). For patients with a clinically suspected DVT, CT venography has demonstrated results comparable to conventional venography in the detection of DVT (11). Indirect CT venography has also shown similar results to sonography in diagnosing or excluding DVT (12). However, data using CT pulmonary angiography and indirect CT venography (CTPA-CTV) in detecting asymptomatic, as well as suspected VTE, in patients undergoing major orthopedic surgery are still lacking (13).
We performed a prospective study to determine the incidence of VTE, specifically proximal DVT or PE, from the perspective of PE in Korean patients undergoing major orthopedic surgery without thromboprophylaxis. Another objective of this study was to investigate the risk factors and the value of CTPA-CTV for proximal DVT or PE in these patients.
All patients who were ≥18 yr of age who underwent elective major orthopedic surgery, including total hip replacement, total knee replacement, or hip fracture surgery, at a tertiary referral center (Kyungpook National University Hospital [KNUH] in Daegu, Korea) were eligible for recruitment. Exclusion criteria were: 1) preoperative azotemia (serum creatinine >1.5 mg/dL); 2) an experience of hypersensitivity to contrast media; 3) receiving any kind of pharmacologic thromboprophylaxis, such as unfractionated heparin, low-molecular-weight heparins, vitamin K antagonists, antiplatelet agents, or dextran. Aspirins or non-steroidal anti-inflammatory drugs were discontinued 3-7 days before surgery. Elastic stockings were used postoperatively at least until discharge in all patients.
Between October 2005 and February 2008, 375 patients undergoing the aforementioned orthopedic surgeries at KNUH were recruited in the present study. Of these, 12 were excluded from the study. Seven patients did not agree to the study protocol and five patients were eliminated due to poor quality of CTPA-CTV. Consequently, 363 patients were included in the present study. The patients were scheduled to undergo CT scan 5-9 days after the major orthopedic surgery but CT scan may be delayed until 14 days depending on their clinical conditions, such as postoperative azotemia. This study was approved by the Institutional Review Boards of Kyungpook National University Hospital, and written informed consent was obtained from each patient.
Characteristics of the patients were recorded at baseline and during the hospital stay including age, gender, body mass index (BMI), smoking, history of a VTE, past or active malignancy, congestive heart failure, varicose veins, estrogen use or hormone replacement therapy, type of surgery, type of anesthesia, duration of surgery, and length of hospital stay. A patient who had smoked at least once a day for >1 yr in his or her lifetime was regarded as an ever-smoker. The cumulative cigarette dose (pack-years) was calculated using the following formula: pack-years=(packs per day)×(years smoked).
All patients were examined by a CT scan from 5-14 days after the major orthopedic surgery. On CT scan, PE was diagnosed when a sharply delineated pulmonary arterial filling defect was observed in at least two consecutive image sections and located centrally within the vessel or with acute angles at its interface with the vessel wall (Fig. 1) (14). A DVT was defined as a low-attenuating partial or complete intraluminal filling defect surrounded by a high-attenuating ring of enhanced blood that was seen on at least two consecutive transverse images (Fig. 2) (15). A proximal DVT was defined as a thrombosis at the level of the popliteal vein or above and a distal DVT as a thrombosis affecting the axial calf veins (4).
CT scans were performed using MDCT scanners with 16 detector rows (Light Speed 16; General Electric, Milwaukee, WI, USA) or with 64 detector rows (Aquilion 64; Toshiba Medical System, Tokyo, Japan). The scan was obtained in the craniocaudal direction during a single inspiratory breath-hold, ranging from the apex to the diaphragm. The CT parameters used were 120 kVp and a 16×0.75 mm collimation with a pitch of <1.5. Low osmolar non-ionic contrast material (2 mL/kg; up to 150 mL) was injected through an antecubital vein at 3-4 mL/sec. Individual contrast optimization was achieved using bolus tracking within the main pulmonary artery. Indirect CT venography was done from the diaphragm to the ankles to detect DVT 140 sec after a thoracic scan.
Statistical analyses were performed using SPSS software, version 12.0 (SPSS Inc., Chicago, IL, USA). The data are expressed as the mean±standard deviation (SD) or median with range (minimum-to-maximum), if the data were skewed for continuous variables, and percentages for categorical variables. Between the two groups, the continuous variables were compared by the Student's t-test and Mann-Whitney U test if non-normally distributed, whereas the categorical variables were compared using a chi-square test or Fisher's exact test. Multiple logistic regression analysis was performed to evaluate the variables determining the risk of VTE. The association between VTE and the variables that were significant at a P value <0.1 in the univariate model was analyzed using logistic regression model. In the remaining analyses, two-sided P values <0.05 was considered to be statistically significant.
The baseline characteristics of the subjects are summarized in Table 1. The patients were female dominant (male-to-female ratio, 1:1.4) with a mean age of 63 yr. Approximately 30% of the patients were ever smokers with a median pack-years of 23 pack-years (range, 1-94 pack-years). The mean BMI was 23 kg/m2. The most common co-morbid condition was hypertension followed by trauma, ischemic heart disease and congestive heart failure. The patients were classified as follows according to the type of orthopedic surgery; total hip replacement group (n=184, 50.7%), hip fracture surgery group (n=122, 30.6%), and total knee replacement group (n=57, 15.7%). The median duration of surgery was 150 min (range, 80-490 min) and the length of hospital stay after the surgery was 14 days (range, 7-221 days). Approximately 60% of the patients had general anesthesia and the remaining patients had regional anesthesia (spinal or epidural).
VTE occurred in 59 patients (16.3%; Table 2), of whom 8 patients were symptomatic (2.2%; Table 3). The rate of VTE was the highest in total knee replacement group (40.4%), followed by hip fracture surgery (16.4%), and total hip replacement groups (8.7%; P<0.001). The frequency of distal DVT (P<0.001), proximal DVT (P=0.018), and the combined rate of proximal DVT and PE (P=0.002) were significantly higher in the patients undergoing total knee replacement compared with the other groups of patients.
Proximal DVT occurred in 5.5% of the patients (n=20; Table 2), including 0.8% of patients who were symptomatic (n=3; Table 3). The overall incidence of PE was 6.6% (n=24; Table 2) and the symptomatic PE rate was 1.1% (n=4; Table 3). Only two patients presented with a form of massive PE, but no patients died of VTE.
The proximal DVT or PE group consisted of 41 patients (11.3%). The females were the majority (73.2% vs. 55.9%; P=0.035) and patients ≥65 yr of age was more common (70.7% vs. 49.1%; P=0.009) (Table 4). However, ever-smokers were less common in the proximal DVT or PE group compared with the patients of control group without the proximal DVT or PE. Among co-morbid conditions, ischemic heart disease or congestive heart failure (22.2% vs. 6.5%; P=0.062) and cerebrovascular accidents (9.8% vs. 3.7%; P=0.093) tended to be more common in the proximal DVT or PE group than the control group. In the proximal DVT or PE group, more patients underwent total knee replacement (31.7% vs. 13.7%; P=0.003) and were more frequently anesthetized regionally compared with the control group (61.0% vs. 36.6%; P=0.003). Regional anesthesia is known to reduce the odds of postoperative VTE (16, 17), type of anesthesia was not included in the multivariate analyses, despite a statistical significance on the univariate analysis.
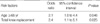
On univariate analyses, the risk factors for proximal DVT or PE, we included female gender, age ≥65 yr, ischemic heart disease or congestive heart failure, cerebrovascular accidents, and total knee replacement surgery as significant factors for multivariate analysis. On multivariate analysis, total knee replacement and age ≥65 yr were significant risk factors for proximal DVT or PE in patients undergoing major orthopedic surgery (odds ratio [OR], 2.4; 95% confidence interval [CI], 1.1-5.1; P=0.025; and OR, 2.1; 95% CI, 1.0-4.4; P=0.046; Table 5).
This is the first large scale study reporting the incidence of PE as well as DVT using CTPA-CTV after major orthopedic surgery. While the incidences of VTE, proximal DVT, and PE were 16.3%, 5.5%, and 6.6%, respectively, symptomatic VTE, proximal DVT, and PE were observed in 2.2%, 0.8%, and 1.1%, respectively. One of the strong points of CTPACTV is making more accurate diagnosis of PE possible (9). Therefore, we focused on the occurrence of PE. In terms of the development of PE, the proximal DVT or PE group comprised 11.3% of all subjects. Subsequently, a multivariate analysis confirmed that total knee replacement and age ≥65 yr were significant risk factors for proximal DVT or PE after major orthopedic surgery in Korean patients.
The ability of CT venography to detect DVT is comparable to that of Doppler sonography in symptomatic patients, implying that CT venography is an alternative modality, at least in symptomatic patients or patients with a clinical suspicion for a DVT (11, 12, 18, 19). There have been no studies comparing CT venography versus conventional venography in detecting DVT in asymptomatic patients. Recently published epidemiologic studies (1, 3, 4) have demonstrated that the incidence of VTE, especially DVT, in Asian patients was comparable to that in Western populations. Several studies involving Korean patients undergoing total hip replacement without pharmacologic thromboprophylaxis (20-22) demonstrated that the incidence of postoperative DVT was 10-25% based on conventional venography, which was considerable, but less than reported in Western countries. In the present study, however, the incidence of DVT after total hip replacement was only 5%, which was much lower than expected. After total knee replacement, the incidence of DVT (39%) was consistent with that in a previous study (23) for Korean patients, but less than reported in Asian multicenter studies (3, 4). These findings suggest that, unlike suspected DVT, asymptomatic venographic DVT may be underdiagnosed with CT venography compared to conventional venography.
Most of the epidemiologic studies regarding postoperative VTE, especially after orthopedic surgery, have focused on the development of DVT. We directed our attention to PE and tried to determine the combined incidence of PE and proximal DVT on the basis of CTPA-CTV. Although a study (13) in which CTPA-CTV was performed to detect DVT and PE after total knee arthroplasty was recently published, it was small-numbered and PE was not observed in any patient. The incidence of proximal DVT (5.5%) was lower in the present study compared with that based on contrast venography for Asian patients (9.2% and 10.2%, respectively) (3, 4). The overall incidence of CT-angiographic PE was 6.6%, but patients with symptomatic PE constitute 1.1% of the subjects, defining more certainly the incidence of asymptomatic or symptomatic PE. Symptomatic PE was reported to be 0-0.5% on the basis of lung perfusion scans in Asian patients, such as Korean after total knee arthroplasty or total hip arthroplasty (3, 4, 22, 23).
A literature review for Asian populations (24) demonstrated that the adjusted incidence of symptomatic PE was 1.4% after total hip replacement. From these results, we infer that PE develops less frequently in Asian patients compared with the Western population (2). In addition, we confirm that PE is more readily diagnosed on CT pulmonary angiography compared with conventional methods, such as lung perfusion scanning.
Knee joint replacement and age ≥65 yr were confirmed as the risk factors for postoperative proximal DVT or PE. Old age has already been considered as an important risk factor for VTE (2). The importance of knee joint replacement as a risk factor for VTE was noted in previous studies (3, 4, 18). Immobilization, soft tissue swelling, and inflammation after joint surgery are considered the main causes (18). However, this can be explained by a notion that the timing of postoperative VTE may differ with the type of surgery (25, 26). Compared with total hip replacement, total knee replacement is associated with twice the frequency of asymptomatic, venographically detected DVT at discharge from hospital and a median of 7 rather than 17 days to the occurrence of postoperative symptomatic VTE (26). In the present study, the incidences of total VTE, distal DVT, and proximal DVT were higher in the total knee replacement group than the remaining surgical groups. The incidence of VTE in the total knee replacement group (-40%) was very similar to the 39% reported by Miyagi and colleagues (13).
Several limitations need to be noted. First, the data were not compared with conventional pulmonary angiography and venography of the lower extremities, the gold standard for the diagnosis of VTE. Compared with the earlier reports based on conventional venography (2), the frequency of venographic DVT may have been underestimated in the present study. Second, as this study was not a multicenter study, there may be a limitation in applying these findings to the whole Korean population. However, except for asymptomatic DVT cases, the incidence of symptomatic VTE was consistent with a previous report (1), suggesting that the estimates in the present study may reflect those of the overall Korean population. Lastly, the time of CT scan from the surgery was variable. As described above, CT scan was planned 5-9 days after the surgery but delayed until 14 days due to the clinical conditions, such as postoperative azotemia. However, one of the largest epidemiologic studies for postoperative VTE in Asians (3) adopted the same timing of venography as the present study.
In conclusion, the incidence of symptomatic VTE in Korean patients was comparable to that of other Asian patients, but lower than the Western population. The overall incidence of PE was 6.6% with a symptomatic PE rate of 1.1%. Knee joint replacement and age ≥65 yr were significant risk factors for postoperative proximal DVT or PE. CTPA-CTV may be useful in assessing symptomatic or clinically suspected VTE after major orthopedic surgery.
Figures and Tables
 | Fig. 1On CT scan, a pulmonary embolus is visualized as a sharply delineated filling defect (arrow) in posterobasal segmental artery of right lower lobe with intact marginal blood flow in at least two consecutive image sections. |
 | Fig. 2On CT scan, a deep venous thrombus is demonstrated in right superficial femoral vein as an intraluminal filling defect (arrow) surrounded by a high-attenuating ring of enhanced blood on at least two consecutive transverse images. |
References
1. Leizorovicz A, Turpie AG, Cohen AT, Wong L, Yoo MC, Dans A. Epidemiology of venous thromboembolism in Asian patients undergoing major orthopedic surgery without thromboprophylaxis. The SMART study. J Thromb Haemost. 2005. 3:28–34.

2. Geerts WH, Pineo GF, Heit JA, Bergqvist D, Lassen MR, Colwell CW, Ray JG. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004. 126:338S–400S.
3. Leizorovicz A. Epidemiology of post-operative venous thromboembolism in Asian patients. Results of the SMART venography study. Haematologica. 2007. 92:1194–1200.

4. Piovella F, Wang CJ, Lu H, Lee K, Lee LH, Lee WC, Turpie AG, Gallus AS, Planes A, Passera R, Rouillon A. Deep-vein thrombosis rates after major orthopedic surgery in Asia. An epidemiological study based on postoperative screening with centrally adjudicated bilateral venography. J Thromb Haemost. 2005. 3:2664–2670.

5. Lotke PA, Ecker ML, Alavi A, Berkowitz H. Indications for the treatment of deep venous thrombosis following total knee replacement. J Bone Joint Surg Am. 1984. 66:202–208.

6. Stulberg BN, Insall JN, Williams GW, Ghelman B. Deep-vein thrombosis following total knee replacement. An analysis of six hundred and thirty-eight arthroplasties. J Bone Joint Surg Am. 1984. 66:194–201.

7. Dahl OE, Andreassen G, Aspelin T, Müller C, Mathiesen P, Nyhus S, Abdelnoor M, Solhaug JH, Arnesen H. Prolonged thromboprophylaxis following hip replacement surgery-results of a double-blind, prospective, randomised, placebo-controlled study with dalteparin (Fragmin). Thromb Haemost. 1997. 77:26–31.
8. Gulsun Akpinar M, Goodman LR. Imaging of pulmonary thromboembolism. Clin Chest Med. 2008. 29:107–116.

9. Stein PD, Fowler SE, Goodman LR, Gottschalk A, Hales CA, Hull RD, Leeper KV Jr, Popovich J Jr, Quinn DA, Sos TA, Sostman HD, Tapson VF, Wakefield TW, Weg JG, Woodard PK. Multidetector computed tomography for acute pulmonary embolism. N Engl J Med. 2006. 354:2317–2327.

10. Thomas SM, Goodacre SW, Sampson FC, van Beek EJ. Diagnostic value of CT for deep vein thrombosis: results of a systematic review and meta-analysis. Clin Radiol. 2008. 63:299–304.

11. Baldt MM, Zontsich T, Stümpflen A, Fleischmann D, Schneider B, Minar E, Mostbeck GH. Deep venous thrombosis of the lower extremity: efficacy of spiral CT venography compared with conventional venography in diagnosis. Radiology. 1996. 200:423–428.

12. Goodman LR, Stein PD, Matta F, Sostman HD, Wakefield TW, Woodard PK, Hull R, Yankelevitz DF, Beemath A. CT venography and compression sonography are diagnostically equivalent: data from PIOPED II. AJR Am J Roentgenol. 2007. 189:1071–1076.

13. Miyagi J, Funabashi N, Suzuki M, Asano M, Kuriyama T, Komuro I, Moriya H. Predictive indicators of deep venous thrombosis and pulmonary arterial thromboembolism in 54 subjects after total knee arthroplasty using multislice computed tomography in logistic regression models. Int J Cardiol. 2007. 119:90–94.

14. Gladish GW, Choe DH, Marom EM, Sabloff BS, Broemeling LD, Munden RF. Incidental pulmonary emboli in oncology patients: prevalence, CT evaluation, and natural history. Radiology. 2006. 240:246–255.

15. Cham MD, Yankelevitz DF, Shaham D, Shah AA, Sherman L, Lewis A, Rademaker J, Pearson G, Choi J, Wolff W, Prabhu PM, Galanski M, Clark RA, Sostman HD, Henschke CI. Deep venous thrombosis: detection by using indirect CT venography. The Pulmonary Angiography-Indirect CT Venography Cooperative Group. Radiology. 2000. 216:744–751.
16. Roders A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A, Sage D, Futter M, Saville G, Clark T, MacMahon S. Reduction of postoperative mortality and morbidity with epidural or spinal anesthesia: results from overview of randomized trials. BMJ. 2000. 321:1493.
17. Urwin SC, Parker MJ, Griffiths R. General versus regional anaesthesia for hip fracture surgery: a meta-analysis of randomized trials. Br J Anaesth. 2000. 84:450–455.

18. Byun SS, Kim JH, Kim YJ, Chun YS, Park CH, Kim WH. Evaluation of deep vein thrombosis with multidetector row CT after orthopedic arthroplasty: a prospective study for comparison with Doppler sonography. Korean J Radiol. 2008. 9:59–66.

19. Lim KE, Hsu WC, Hsu YY, Chu PH, Ng CJ. Deep venous thrombosis: comparison of indirect multidetector CT venography and sonography of lower extremities in 26 patients. Clin Imaging. 2004. 28:439–444.
20. Kim YH, Suh JS. Low incidence of deep-vein thrombosis after cementless total hip replacement. J Bone Joint Surg Am. 1988. 70:878–882.

21. Kim YH, Choi IY, Park MR, Park TS, Cho JL. Prophylaxis for deep vein thrombosis with aspirin or low molecular weight dextran in Korean patients undergoing total hip replacement. A randomized controlled trial. Int Orthop. 1998. 22:6–10.
22. Kim YH, Kim JS. The 2007 John Charnley Award. Factors leading to low prevalence of DVT and pulmonary embolism after THA: analysis of genetic and prothrombotic factors. Clin Orthop Relat Res. 2007. 465:33–39.
23. Kim YH, Kim JS. Incidence and natural history of deep-vein thrombosis after total knee arthroplasty. A prospective, randomised study. J Bone Joint Surg Br. 2002. 84:566–570.
24. Leizorovicz A, Turpie AG, Cohen AT, Dhillon KS, Angchaisuksiri P, Wang CJ. Epidemiology of post-operative venous thromboembolism in Asian countries. Int J Angiol. 2004. 13:101–108.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download