Abstract
This study was performed to evaluate the utilization and outcomes of palivizumab in high risk children born prematurely with chronic lung disease (CLD). A retrospective review of 128 patients was conducted from September 2004 to March 2009 at the Ajou University Hospital. All patients were diagnosed with CLD, were born at ≤35 weeks of gestation, were <2 yr old at the onset of respiratory syncytial virus (RSV) season, and had received medical therapy within six months prior to the RSV season. Fifty-three patients did not receive palivizumab prophylaxis and 75 patients received at least one dose of palivizumab. There were no statistically significant differences between the patients with and without palivizumab prophylaxis with regard to demographic characteristics and risk factors for RSV infection. There were no systemic adverse responses. Compliance with the course of prophylaxis was 92.2%. Hospitalization associated with RSV occurred in 12 cases (22.6%) in the group without prophylaxis and in three cases (4.0%) with prophylaxis. Palivizumab prophylaxis significantly reduced the frequency of RSV-related hospitalization in preterm children with CLD. This is the first retrospective review of palivizumab prophylaxis in Korea. Palivizumab is effective and well tolerated in high risk prematurely born children.
Respiratory syncytial virus (RSV) is the major viral cause of respiratory illness and is associated with life-threatening complications in young infants between 8 and 30 weeks of age (1, 2). RSV infection causes acute inflammation, edema, and necrosis of epithelial cells of the small airways, and is associated with increased mucus production and bronchospasm. Overall, mechanical ventilation with intensive care is needed in 1-2% of children with RSV infections (3-5), and worldwide RSV infection accounts for 600,000 deaths per year (3, 6).
Compared to full-term infants, premature infants (less than 35 weeks gestation) are at higher risk for severe lung disease and respiratory failure due to their immature lungs, unfavorable pulmonary compliance, high airway resistance, and friable chest wall. Therefore, RSV infection is associated with a higher morbidity and mortality in premature infants (7, 8).
Various therapeutic interventions including bronchodilators, corticosteroids, ribavirin, chest physiotherapy, and oxygen have been used for treatment; however, no specific therapeutic method has been proven effective against RSV (4). Recently, prevention of RSV infection has focused on passive immunization with palivizumab prophylaxis.
Palivizumab, a humanized monoclonal immunoglobulin G preparation against the F glycoprotein of RSV, was approved for use in the USA in 1998 and it was approved in Europe in 1999. In a placebo-controlled Impact-RSV trial in the USA, intramuscular palivizumab prophylaxis was shown to be safe and reduced RSV-related hospitalization in premature infants by 55% (9).
In Korea, since 2005, palivizumab prophylaxis has been used in premature children with chronic lung disease (CLD) born at ≤35 weeks of gestation, in children <2 yr of age that also received medical therapy (supplemental oxygen, bronchodilator, diuretics, or corticosteroid therapy) within six months prior to the RSV season. However, no data has been published on the efficacy of palivizumab and patient outcomes over multiple seasons in Korea.
We retrospectively reviewed the clinical outcomes of premature children with CLD that received one or more doses of palivizumab during the 2005 to 2009 RSV seasons and the children that did not receive palivizumab during the 2004 to 2009 RSV seasons in Korea. The demographic, clinical characteristics, respiratory illness, and RSV hospitalizations were compared between the two groups.
The goals of the present study were to determine the safety and efficacy of palivizumab prophylaxis for reducing RSV related illness among the high risk premature children with CLD, and to provide information for the utilization and compliance of palivizumab prophylaxis.
We retrospectively reviewed the clinical data of preterm children between September 2004 and March 2009 at the Ajou University Hospital. During the periods, 135 patients needed for oxygen >21% for at least 28 days and had the clinical diagnosis of CLD (or bronchopulmonary dysplasia). The inclusion criteria specified that children were born at ≤35 weeks of gestation, were <2 yr of age at the onset of the RSV season, and had received medical therapy (supplemental oxygen, bronchodilator, diuretics, or corticosteroid therapy) within six months prior to the RSV season. Children were excluded if they had any of the following: known renal impairment, hepatic dysfunction, immunodeficiency, neuromuscular impairment, chromosomal anomalies, congenital metabolic diseases, major congenital anomalies, or congenital heart disease with cyanosis or heart failure except for those with a patent ductus arteriosus or a septal defect that was uncomplicated and hemodynamically insignificant.
Among the 135 patients with CLD, seven patients were excluded. They had the clinical diagnosis of tetralogy of Fallot (n=1), tracheoesophageal fistula (n=2), congenital diaphragmatic hernia (n=1), 18 trisomy (n=1), congenital hydrocephalus (n=1) and Goltz syndrome (n=1). We enrolled 128 patients with CLD and reviewed their clinical course. Fifty three patients did not receive palivizumab prophylaxis and 75 received at least one dose of palivizumab.
Personal information was collected including demographics (birth weight, gestational age), neonatal course as well as medical and family history. Injection information included the date, dose, frequency, intervals and the response to the injections over seven days after the injection. Data, specific to hospitalization for respiratory illness, included the type of respiratory infection, hospital stay, isolated microorganisms or viruses, treatment, and dates. The study protocol and procedures were reviewed and approved by the Institutional Review Board of Ajou University Hospital.
Palivizumab (Synagis®, Boehringer Ingelheim Pharma, Biberach an der Riss, Germany) prophylaxis was provided from September to March. Patients received palivizumab (15 mg/kg) by intramuscular injection every 30 days. Palivizumab was supplied as a lyophilized powder in vials that were reconstituted with sterile water for injection and dispensed as a unit dose in a syringe. The final concentration of palivizumab was 100 mg/mL.
The severity of CLD (or bronchopulmonary dysplasia) was classified by the "new" bronchopulmonary dysplasia (BPD) definition criteria (10). Patients hospitalized for respiratory illness were classified into one of four clinical syndromes, according to Denny and Clyde (11).
RSV hospitalization was defined as any hospitalization with a duration of 24 hr or longer in a patient with positive RSV testing. The decision to admit to the hospital was based on the guidelines of the Denver Children's Hospital (Denver, CO, USA) (12). Patients were admitted when they had a poor response to oral medication and/or inhalation therapy, poor oral feeding, apnea, hypoxia, signs of dehydration, and/or signs of sepsis.
Compliance with the injection regimen was determined by comparing the actual number of injections received with the expected number of doses, based on the month the first injection was given.
Nasopharyngeal aspirates were collected on hospital admission by inserting a 5 Fr nasogastric tube into the nasopharynx with negative pressure suction. The aspirates were collected into viral transport medium and delivered to the laboratory. RSV was detected by either the immunofluorescence rapid antigen test with the Respiratory Panel Viral Screening & Identification Kit®(Chemicon, Temecula, CA, USA) or RT-PCR. Virological tests were performed by the clinical laboratory at the Seoul Medical Science Institute.
The characteristics of the patients with and without prophylaxis were compared with the Student's t-test and Fisher's exact test focusing on differences in demographic characteristics, risk factors for RSV infection and RSV associated hospitalization. The severity of BPD in these patients was compared using Pearson chi-square tests. The data were entered into a Microsoft Excel database and SPSS 11.0 was used for the data analysis.
The characteristics of all patients are summarized in Table 1. All patients received oxygen therapy for more than 28 days after birth. A total of 53 patients did not receive palivizumab prophylaxis. Twenty one patients were diagnosed during the 2004 to 2005 RSV season prior to the approval of palivizumab prophylaxis, and 32 patients did not receive palivizumab because their parents declined the injection due to financial problems. Seasonal RSV prophylaxis injections were given to 75 children between September 2005 and March 2009.
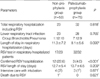
There were no significant differences in the neonatal demographics including gestational age, birth weight, gender, and type of delivery. The follow-up duration and initial duration of the hospital stay showed no statistically significant differences. The severity of BPD and co-morbidities included multiple births, congenital heart disease, and patent ductus arteriosus; there were no statistically significant differences among these factors (Table 1).
Seventy one patients received one season of prophylaxis; a second-season of prophylaxis was given to one patient with moderate BPD and three patients with severe BPD. Palivizumab prophylaxis increased during the 2008 to 2009 RSV season (Table 1). Palivizumab injection was started at the neonatology intensive care unit in 63 patients. A total of 284 injection doses were provided. The mean±SD of received injections was 3.4±1.6 (range 1-6). A total of six doses were injected in four patients. All of the expected injections were given to 62 patients. Compliance (Actual No. of injections/No. of recommended injections×100) was 92.2%. None of the patients dropped out; however, the last injection dose was not received in 13 patients. The mean interval between injections was 31.3 days; all doses were given within 35 days after previous injection.
There were no systemic, respiratory or gastrointestinal symptoms noted after the injections. Erythema and swelling at the injection site was noted in three patients, and subsided within three days (Table 2).
Overall, respiratory hospitalizations occurred in 23 patients that did not receive prophylaxis and in 32 patients that received palivizumab prophylaxis. The total number of respiratory hospitalizations, characteristics of lower respiratory tract infections (LRTI), and the length of hospital stay showed no statistically significant differences between patients with or without prophylaxis. Of 55 hospitalized patients, 49 patients were tested for laboratory tests for RSV. The rate of LRTI hospitalizations associated with RSV was 22.6% (12/53) in cases without prophylaxis and 4.0% (3/75) in cases with prophylaxis. Monthly prophylaxis with palivizumab significantly reduced the RSV associated hospitalization. Intubation and intensive care were needed in four patients with RSV, in two patients with a metapneumovirus infection, and in one patient with parainfluenza infection. One of the patients without prophylaxis, with RSV, died while receiving intensive care treatment with mechanical ventilation in January 2005. The length of the RSV hospital stay was not significantly different between the two groups (Table 3). Prior to the hospitalization for RSV, 14 patients were at home and one patient who received prophylaxis was in a rehabilitation facility. RSV hospitalizations occurred throughout the RSV season and in April (Table 4). Of the patients who received RSV prophylaxis, RSV was detected 31 days after previous prophylaxis in two patients, and 32 days after previous prophylaxis in one patient, respectively.
A long term surveillance study in Korea showed that RSV was the most common cause of LRTI among young children (13-16); and readmissions to the hospital for RSV infection has been reported to be 22.2% in premature infants (17).
Outbreaks of RSV occur annually worldwide. In the USA, outbreaks of RSV typically begin in November or December, peak in January or February, and end in March or April (18). A pilot study to establish a nationwide surveillance system was started in 2005 by the Korean Centers for Disease Control and Prevention (KCDC). The KCDC defines the RSV season from October to March in Korea; however, the season varied considerably year by year (13-16).
Occurrence of RSV disease is inevitable especially during seasons. Therefore, prevention is essential for decreasing the morbidity and mortality associated with the disease. After US FDA approval in 1998, palivizumab prophylaxis has been used in many countries (19-23). The data from the Palivizumab Outcomes Registry in the USA showed that the incidence of RSV hospitalization was decreased with palivizumab prophylaxis (21) and the majority of RSV hospitalizations occurred between the first and second dose injections (22).
The American Academy of Pediatrics has revised its evidence-based guidelines for RSV immunoprophylaxis with palivizumab. The 2003 guidelines recommended palivizumab prophylaxis in certain preterm infants without co-morbidities: 1) children born at 28 weeks gestation or earlier that are 12 months of age or less at the start of RSV season, 2) children born at 29 to 32 weeks gestation that are 6 months of age or less at the start of RSV season, and 3) children born at 32 to 35 weeks gestation that are 6 months of age or less at the start of RSV season and have at least two risk factors. The risk factors include congenital abnormalities of the airways, severe neuromuscular disease, child-care attendance, exposure to environmental air pollutants, and school-aged siblings (24, 25).
Since 2005, we have provided palivizumab prophylaxis to certain children born prematurely with CLD. According to the National Health Insurance Corporation of Korea, palivizumab prophylaxis is only indicated in children with CLD that have received medical therapy (supplemental oxygen, bronchodilator therapy, diuretics, or corticosteroid therapy) within 6 months prior to the RSV season, and are 2 yr of age or younger at the start of RSV season.
This is the first retrospective review of palivizumab prophylaxis, performed from the first year of prophylaxis to the most current RSV season in Korea. In this study, palivizumab prophylaxis was provided to children born prematurely with CLD. A total of 75 patients received palivizumab injections. However, palivizumab prophylaxis was declined in 32 patients by their parents from 2005 to 2009. Palivizumab prophylaxis was given to more infants from 2007 to 2009, during the RSV seasons (Table 1). The economic support from the National Health Insurance Corporation of Korea for prophylaxis has increased starting in 2007. Reducing the economic burden of prophylaxis was helpful for parent agreement. Interruption of prophylaxis (13/75) was most commonly related to economic burden.
Although this study was not a randomized, double-blind, placebo-controlled trial, the demographic characteristics and co-morbidities were not different significantly between patients with and without prophylaxis (Table 1). Palivizumab prophylaxis showed an 82% reduction of RSV-associated hospitalization compared to the patients without prophylaxis. In the present study, the overall frequency of RSV hospitalization among premature children with CLD in the patients that received palivizumab prophylaxis (4.0%). The rate was lower than those reported, in the Impact-RSV clinical trial (7.9%) (9), in the Outcome Registry of USA in 2000-2001 (5.8%) (22), in Canada in 1999-2000 (6.0%) (19) and in a cohort study in Europe during 2000-2002 (11.35%) (21).
RSV testing was not routinely performed in the outpatient setting; and this is a limitation of this study. The data reported here might therefore underestimate the true incidence of RSV-related infection. During the follow-up, however, the total frequency of respiratory hospitalizations and requirement for mechanical ventilation were not significantly different according to palivizumab prophylaxis (Table 3); it is not clear whether palivizumab prophylaxis itself alleviates the severity of the respiratory illness.
In all of three RSV hospitalized patients who received prophylaxis,
RSV was confirmed just prior to the date of scheduled injections. Because these patients had weight gains of 750 to 1,000 g over one month, we assumed that relative activity of the specific IgG against RSV antigen may not be sufficient in these patients. However, we could not confirm this. Also, we could not examine thoroughly the risk factors associated with the failure of palivizumab prophylaxis in these cases.
RSV hospitalization in one patient occurred in April after KCDC definitioning season. A children born prematurely with CLD are susceptible to respiratory infections throughout the year (Table 4). Therefore, for the efficacy of prophylaxis, further study is required including consideration of the variation of RSV outbreaks in Korea.
In conclusion, this is the first study to report on the utilization and outcomes of palivizumab prophylaxis in Korea. Palivizumab prophylaxis was effective, well-tolerated, and compliance was high in the children born prematurely with CLD that were at high risk for developing severe RSV infection. Palivizumab prophylaxis reduced RSV hospitalization significantly (22.6% vs. 4.0% in without and with palivizumab prophylaxis, retrospectively). This result is a favorable outcome when compared to the trial conducted in the USA, data from Outcome Registries, and other prospective studies in different countries. This information can be used to determine the efficacy of palivizumab prophylaxis in children at high risk of RSV infection.
Figures and Tables
Table 1
Comparison of demographics and clinical characteristics including risk factors for RSV infection between patients without prophylaxis and with palivizumab-prophylaxis

References
2. Boyce TG, Mellen BG, Mitchel EF Jr, Wright PF, Griffin MR. Rates of hospitalization for respiratory syncytial virus infection among children in medicaid. J Pediatr. 2000. 137:865–870.

3. Holman RC, Shay DK, Curns AT, Lingappa JR, Anderson LJ. Risk factors for bronchiolitis-associated deaths among infants in the United States. Pediatr Infect Dis J. 2003. 22:483–490.

4. American Academy of Pediatrics Subcommittee on Diagnosis and Management of Bronchiolitis. Diagnosis and management of bronchiolitis. Pediatrics. 2006. 118:1774–1793.
5. Loughlin GM, Moscona A. The cell biology of acute childhood respiratory disease: therapeutic implications. Pediatr Clin North Am. 2006. 53:929–959.

6. Thompson WW, Shay DK, Weintraub E, Brammer L, Cox N, Anderson LJ, Fukuda K. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003. 289:179–186.

7. Thorburn K. Pre-existing disease is associated with a significantly higher risk of death in severe respiratory syncytial virus infection. Arch Dis Child. 2009. 94:99–103.

8. Sampalis JS. Morbidity and mortality after RSV-associated hospitalizations among premature Canadian infants. J Pediatr. 2003. 143:5 Suppl. S150–S156.

9. The Impact-RSV Study Group. Palivizumab, a humanized respiratory syncytial virus monoclonal antibody, reduces hospitalization from respiratory syncytial virus infection in high-risk infants. Pediatrics. 1998. 102:531–537.
10. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001. 163:1723–1729.

11. Denny FW, Clyde WA Jr. Acute lower respiratory tract infections in nonhospitalized children. J Pediatr. 1986. 108:635–646.

13. Kim YK, Nyambat B, Hong YS, Lee CG, Lee JW, Kilgore PE. Burden of viral respiratory disease hospitalizations among children in a community of Seoul, Republic of Korea, 1995-2005. Scand J Infect Dis. 2008. 40:946–953.
14. Ahn KM, Chung SH, Chung EH, Koh YJ, Nam SY, Kim JH, Son JA, Park JY, Lee NY, Lee SI. Clinical characteristics of acute viral lower respiratory tract infections in hospitalized children in Seoul, 1996-1998. J Korean Med Sci. 1999. 14:405–411.

15. Kim MR, Lee HR, Lee GM. Epidemiology of acute viral respiratory tract infections in Korean children. J Infect. 2000. 41:152–158.
16. Choi EH, Lee HJ, Kim SJ, Eun BW, Kim NH, Lee JA, Lee JH, Song EK, Kim SH, Park JY, Sung JY. The association of newly identified respiratory viruses with lower respiratory tract infections in Korean children, 2000-2005. Clin Infect Dis. 2006. 43:585–592.

17. Lee EA, Jeong JH, Yu ST, Lee CW, Yoon HS, Park DS, Oh YK. Incidence and risk factors of rehospitalization with respiratory syncytial virus infection in premature infants. Korean J Pediatr. 2004. 47:510–514.
18. Centers for Disease Control and Prevention (CDC). Brief report: respiratory syncytial virus activity-United States, 2005-2006. MMWR Morb Mortal Wkly Rep. 2006. 55:1277–1279.
19. Oh PI, Lanctĵt KL, Yoon A, Lee DS, Paes BA, Simmons BS, Parison D, Manzi P. Palivizumab prophylaxis for respiratory syncytial virus in Canada: utilization and outcomes. Pediatr Infect Dis J. 2002. 21:512–518.

20. Sorrentino M, Powers T. Effectiveness of palivizumab: evaluation of outcomes from the 1998 to 1999 respiratory syncytial virus season. The Palivizumab Outcomes Study Group. Pediatr Infect Dis J. 2000. 19:1068–1071.
21. Frogel M, Nerwen C, Cohen A, VanVeldhuisen P, Harrington M, Boron M. Palivizumab Outcomes Registry Group. Prevention of hospitalization due to respiratory syncytial virus: results from the Palivizumab Outcomes Registry. J Perinatol. 2008. 28:511–517.

22. Palivizumab Outcomes Registry Study Group. Palivizumab prophylaxis of respiratory syncytial virus disease in 2000-2001: results from The Palivizumab Outcomes Registry. Pediatr Pulmonol. 2003. 35:484–489.
23. Saji BT. Indications, efficacy and Safety of Anti-RS Virus Monoclonal Antibody Palivizumab (Synagis) for Pediatric Patients With Congenital Heart Diseases. J Korean Pediatr Cardiol Soc. 2007. 11:149–150.
24. American Academy of Pediatrics Committee on Infectious Diseases and Committee on Fetus and Newborn. Revised indications for the use of palivizumab and respiratory syncytial virus immune globulin intravenous for the prevention of respiratory syncytial virus infections. Pediatrics. 2003. 112:1442–1446.
25. American Academy of Pediatrics. Red-book: 2006 report of the committee on infectious disease. 2006. 27th ed. Elk Grove, IL: American Academy of Pediatrics.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download