Abstract
The surgical closure of patent ductus arteriosus (PDA) is provided more frequently in extremely low birth weight babies who are usually deemed unsuitable for pharmacological closure. We have adopted subaxillary mini-thoracotomy in order to lessen surgical trauma in these babies; and its clinical results were analyzed. From April 2004 to August 2008, out of 50 babies at the neonatal intensive care unit who underwent the surgical closure of PDA, 22 premature babies weighing less than 1 kg at operation were included in the study. Eleven babies were males and mean gestational age was 27 weeks ranging from 23+3 to 30+2 weeks. Mean body weight at operation was 816 g ranging from 490 to 989 g and average age at operation was 17.9±11.9 days. Of them, 17 babies (72%) were ventilator dependent preoperatively, as compared with 13 out of 28 (46%) babies that weighed more than 1 kg (P<0.05). Four babies did not survive to discharge. Among 28 babies who were heavier than 1 kg, there were only one death. However, the mortality difference was not statistically significant (P=0.11). All mortalities were caused by inherent problems of prematurity and co-morbidities. Out of 17 babies who had been ventilator dependent preoperatively, 13 weaned off successfully at 17.0±23.9 days after the operation. The baby patients heavier than 1 kg weaned at 6.0±5.3 days (P=0.27). Surgical outcome of simple and less invasive subaxillary mini-thoracotomy was satisfactory; the surgery is highly recommended for ductal closure in extremely low weight premature babies.
The closure of patent ductus arteriosus is often delayed in prematurities resulting in detrimental effects on successful growth and normal development. Extremely low birth weight (<1,000 g) newborns are usually in a critical condition from inherent problems of prematurity and varying co-morbidities; and thus, surgical closure of the ductus is proposed more frequently in this particular group of patients, who are often deemed unsuitable for pharmacologic closure (1-3). While posterolateral thoracotomy has long been a standard approach for ductal closure, we have lately adopted subaxillary minithoracotomy in prematurities in the hope of lessening surgical trauma. As extremely low birth weight newborns are considered to be highly vulnerable to surgical stress, the clinical results of these babies were analyzed and compared to those of babies weighing more than 1 kg at surgery.
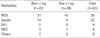
From April 2004 to August 2008, out of 50 babies at the neonatal intensive care unit that underwent the surgical closure of patent ductus arteriosus (PDA), 22 premature babies weighing less than 1,000 grams at operation were included in the study. The operation was performed at the discretion of the pediatric cardiologist and the neonatologist. Eleven babies were males and mean gestational age was 27 weeks ranging from 23+3 to 30+2 weeks. Mean body weight was 816 g ranging from 490 to 989 g and average age at operation was 17.9±11.9 days. Seventeen babies (72%) were ventilator dependent preoperatively, as compared with 13 out of 28 (46%) babies who weighed more than 1 kg (P<0.05) (Table 1). The major co-morbidities were respiratory distress syndrome (n=21), sepsis (n=14), intraventricular hemorrhage (n=5) and necrotizing enterocolitis (n=3) (Table 2).
All operations were performed in the newborn intensive care unit. The surgical procedure has been previously described in detail elsewhere (4). In short, the patient was placed in a lateral position with the left arm abduction under general endotracheal anesthesia. A 2 cm long subaxillary minithoracotomy was made and the pleural cavity was entered via the 3rd intercostal space. The lung was retracted anteroinferiorly with cotton swabs, and the PDA was fully dissected (Fig. 1). The mean size of PDA was 3.4±0.7 mm. For the most part, the ductus was closed with titanium clips; two babies in whom the ductus was ruptured during manipulation underwent ductal division. A chest tube was placed before closing the wound and removed at the end of the procedure in the majority of the cohort. Recently, we prefer to apply single clip rather than double clipping and the procedure became more simplified.
The medical records were reviewed and analyzed in retrospective manner. The numerical values are expressed as mean±standard deviation. SPSS (ver 10.0) software was used for the statistical analysis. Mann-Whitney U test and Fischer's exact test were applied for the comparison of values. P values lower than 0.05 were considered statistically significant.
Mean operative time was 52.1±17.2 min including two cases of ductal rupture. These two babies were salvaged by ductal division and, fortunately, recovered completely without sequalae. Eighteen babies survived to discharge. Four babies succumbed to death after the operation including a baby weighing 490 g, the lowest in the cohort. The main cause of death was sepsis in 3 patients, who died on the 11th, 18th, and 21st postoperative day respectively. The fourth baby suffered from persistent feeding intolerance and was discharged home on the 131st postoperative day against medical advice.
All mortalities were from inherent problems of prematurity and co-morbidities, but not related to the operation per se. Although there were only one death in the group of babies who weighed more than 1 kg, the difference was not statistically significant (P=0.11). No residual shunt was observed postoperatively. In most cases, hemodynamic instability and respiratory distress rapidly improved after the procedure, thus enabling early ventilator weaning and easier volume management. There were no complications among survivors such as hoarseness or chylothorax except for one case of surgical wound infection, which was controlled without difficulty. Delayed pneumothorax developed in one case, supposedly from pneumonia and sepsis, not from operation itself. This patient succumbed to death. Out of 17 babies who had been ventilator dependent preoperatively, 13 were weaned off successfully 17.0±23.9 days after the operation, comparable to 6.0±5.3 days for babies who weighed more than 1 kg (P=0.27). Mean hospital stay after the operation among survivors was 80.0±21.6 days, naturally much longer than that of the babies (37.0±30.8 days) who weighed more than 1 kg (P<0.05) (Table 3).
Follow-up was complete in 18 survivors ranging from 2 months to 56 months. At last follow-up visits, all survivors were growing well, without residual shunts.
Underdevelopment of vascular smooth muscle necessary for ductal closure and a lack of vasocontractile response to oxygen level in blood, along with a increased serum level of vasodilatory prostaglandin, often prevent ductal closure in prematurities, adding the risk of significant left to right shunt to the neonates who are already in critical state from inherent problems associated with prematurity and the presence of various co-morbidities.
The efficacy and safety of the surgical closure of PDA in prematurities has been well addressed (2, 3, 5). In terms of the approach, we have adopted subaxillary mini-thoracotomy instead of standard posterolateral thoracotomy in the hope of lessening surgical trauma as described elsewhere (6); the incision is shorter, the dissection of muscles is minimal and the cosmetic result is excellent as the wound is covered in the axilla. Though exposure is somewhat limited, the dissection is rather straightforward in experienced hands, as premature babies have less connective tissue and the thoracic cavity is not so deep. In fact, based on our experience, the greater the baby weighs, the more demanding the procedure becomes, as the plane of the dissection deepens. The procedure used initially has been simplified over time; now we prefer to apply single clip rather than two and we do not routinely indwell chest tubes.
After operation, in general, blood pressures rose instantaneously and the symptoms of congestion rapidly disappeared. Furthermore, volume management became easier and neonates were weaned off ventilators sooner. Nevertheless, the impact of less invasive surgery on recovery and development of the babies are hardly measurable, as these babies usually continue to be given intensive care for reasons other than PDA. However, we have achieved comparable results in premature babies weighing less than 1 kg to those weighing more in terms of mortality and days of ventilator care after the operation.
Recently, video-assisted thoracoscopic clipping of PDA has been applied to prematurities with reliable results (7, 8). Yet, this technique is not popular partly because it requires special downsized instruments and patient transfer from the intensive care unit to the video equipped operating room. Above all, surgeons are aware of the risk of ductal rupture, no matter how rarely it happens, and its catastrophic consequences. From this point of view, our technique is rather straightforward and offers a reasonable compromise between thoracoscopic and conventional techniques. Some argue that open thoracotomy and inevitable rigorous rib spreading have the potential to exert harmful effects over the thoracic skeletal framework and concerns have been raised of later scoliosis (9), which will need long-term follow-up for confirmatory answer. The transcatheter technique is another modality used for PDA occlusion (10). As yet, it is hardly applicable to low birth weight babies because of the relative inaccessibilities of femoral vessels.
Since the introduction of indomethacin, the standard guideline of treatment has been initial medical treatment for circulatory congestion, followed by indomethacin in repeated rounds as needed. The surgical closure is offered when indomethacin therapy is ineffective (11). However, along with the progress in neonatal care, the prematurities consulted for surgery tend to be younger and weigh less, and often have various co-morbidities that hinder indomethacin trials. Furthermore, the untoward effects of indomethacin are occurring more easily and extensively in seriously ill infants and some infants deteriorates to badly to be salvaged by surgery.
This study shows that our technique is equally effective in extremely low weight babies. In fact, at our institution, the strategy is changing; the neonatologists are fully convinced of the benefit of the procedure and they do not hesitate to consult the patients for surgical closure earlier with fewer attempts of pharmacological closure carrying concomitant risks. We consider, in this context, the operative indications might be extended in favor of early prophylactic surgery to reduce the deadly complications of prematurity such as necrotizing enterocolitis and bronchopulmonary dysplasia.
Figures and Tables
Fig. 1
Operative view. The arrow in (A) indicates clipped PDA and the arrowheads in (B) indicate the healed incision line below the axilla.

References
1. Wright JS, Newman DL. Ligation of the patent ductus: technical considerations at different ages. J Thorac Cardiovasc Surg. 1978. 75:695–698.
2. Trus T, Winthrop AL, Pipe S, Shah J, Langer JC, Lau GY. Optimal management of patent ductus arteriosus in the neonates weighing less than 800 grams. J Pediatr Surg. 1993. 28:1137–1139.
3. Canarelli JP, Poulain H, Clamadieu C, Ricard J, Maingourd Y, Quintard JM. Ligation of the patent ductus arteriosus in premature infantsindications and procedures. Eur J Pediatr Surg. 1993. 3:3–5.
4. Cho JS, Baek WK, Yoon YH, Kim JT, Kim KH, Hong YJ, Jun YH, Shin HR. Surgical closure of the patent ductus arteriosus in premature infants by axillary thoracotomy. Korean J Thorac Cardiovasc Surg. 2007. 40:837–842.
5. Wagner HR, Ellison RC, Zierler S, Lang P, Purohit DM, Behrendt D, Waldhausen JA. Surgical closure of patent ductus arteriosus in 268 preterm infants. J Thorac Cardiovasc Surg. 1984. 87:870–875.

6. Miles RH, DeLeon SY, Muraskas J, Myers T, Quinones JA, Vitullo DA, Bell TJ, Fisher EA, Pifarre R. Safety of patent ductus arteriosus closure in premature infants without tube thoracotomy. Ann Thorac Surg. 1995. 59:668–670.
7. Burke RP, Jacobs JP, Cheng W, Trento A, Fontana GP. Video-assisted thoracoscopic surgery for patent ductus arteriosus in low birth weight neonates and infants. Pediatrics. 1999. 104:227–230.

8. Hines MH, Raines KH, Payne RM, Covitz W, Cnota JF, Smith TE, O'Brien JJ, Ririe DG. Video-assisted ductal ligation in premature infants. Ann Thorac Surg. 2003. 76:1417–1420.

10. Tynan M. Transcatheter occlusion of persistent arterial duct. Report of the European Registry. Lancet. 1992. 340:1062–1066.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download