Abstract
Salmonella enterica has been one of the most widespread foodborne pathogens in Korea. Between 1998 and 2007, a total of 9,472 Salmonella isolates were identified from foodborne and waterborne illness patients. During that time, Korea was transitioning into a developed country in industry as well as in its hygiene system. Although the isolation number of total Salmonella including serovar Typhi has decreased since 1999, the isolation of rare Salmonella serovars has emerged. Three most prevalent serovars during 1998-2007 were S. enterica Typhi, S. enterica Enteritidis, and S. enterica Typhimurium. There were remarkable outbreaks caused by rare serovars such as S. enterica Othmarschen, S. enterica London and S. enterica Paratyphi A, and overseas traveler-associated infections caused by S. enterica Weltevreden and S. enterica Anatum. Salmonella serovars from overseas travelers made a diverse Salmonella serovar pool in Korea. This study is the first review of the status of the human Salmonella infection trend in a developing country during 1998-2007. Newly emerging rare Salmonella serovars should be traced and investigated to control new type pathogens in the developed world.
Salmonella has been a major foodborne and waterborne pathogen in Korea (1, 2). In 2006, Salmonella was a major foodborne bacterial pathogen in the United States, causing more deaths than any other foodborne pathogen (3). S. enterica Typhi, a causative agent of typhoid fever, has especially threatened Korean health (4). There were 1,921 deaths resulting in 17% mortality because of typhoid fever during 1945-1960 in Korea. Salmonellosis caused by non-typhoid Salmonella (NTS) gives rise to diarrhea, vomiting, abdominal pain, and enteric fever. Occasionally, systemic infection with bowel perforation, septicemia, and osteomyelitis are also caused by NTS (5-8).
At present, there are more than 2,500 Salmonella serovars in the world with new serovars emerging yearly. Salmonella serotyping is very important to the epidemiology study. Unquestionably, Salmonella serotyping is time-consuming and complex work for the serological identification of bacteria (9). To serotype Salmonella, lipopolysaccharide epitopes in bacterial membrane (O antigens) and flagella proteins (H antigens) should be identified with the respective antibodies. For the identification of S. enterica Typhi, additional antibody specific to capsular polysaccharides (Vi antigen) is essential. Until 1990, reference laboratories in Korea merely performed sero-grouping with only O antigen-specific and Vi-specific antibodies. Therefore, they were unable to complete serotyping of Salmonella due to expensive commercial antibodies and lack of interest in surveillance. Truly, at present, most poor or developing countries perform only sero-grouping of Salmonella because of the cost problem (10).
Korea National Institute of Health (KNIH) is the headquarters for the national surveillance of Salmonella in Korea. KNIH gathered Salmonella isolates and analyzed their epidemiological data from 17 Research Institutes of Health and Environment located in cities and provinces and 13 quarantine stations located in airports and harbors in Korea. The microbiologists in these 17 regional institutes covering all country and 13 quarantine stations isolated enteric bacteria from patients according to the standardized protocols distributed by KNIH. According to Korea's Infectious Diseases Prevention Act which has been enforced since 1954, certain infectious diseases must be reported to government authorities. These diseases are classified into four classes according to the grade of danger and threat to public health. Among the infectious diseases caused by Salmonella species, typhoid fever and paratyphoid fever are classified as Class 1 notifiable infectious diseases, and NTS-causing diseases are classified as Class 4.
As Korea has developed, the desire for an advanced social hygiene system for the well-being of the people has increased. Transportation, water supply and drainage, medical and food-processing systems were developed. Between the 1990s and 2000s, Korea had one of the highest economic growths in the world. This rapid growth resulted in dramatic changes in lifestyles as well as in incidence of foodborne Salmonella (11).
In this review, three major Salmonella serovars, S. enterica Typhi, S. enterica Enteritidis, and S. enterica Typhimurium, and several remarkable outbreaks caused by rare Salmonella serovars in 1998-2007 are discussed. As complete serotyping of Salmonella was started and its security electronic database was constructed in national reference laboratories from 1998, this study is the first review of the status of the human Salmonella infections trend in Korea during 1998-2007. Finally, overseas-travel associated infection cases and the effects on serovar prevalence in Korea are also discussed.
From 1998 to 2007, S. enterica Typhi, S. enterica Enteritidis, and S. enterica Typhimurium were the most frequent Salmonella serovars in diarrhea patients and foodborne diseases in Korea (Fig. 1, Table 1) (12). From 422 to 2,252 culture-proven Salmonella infection cases and their isolates have been identified every year since 1998. The percentage of these 3 serovars among Salmonella isolates was over 70% almost every year from 1998 to 2007.
S. enterica Typhi is a causative pathogen of typhoid fever. Typhoid was an endemic enteric fever disease in Korea. It is not only systemic infection with high morbidity but also a common public health problem in Korea. The overall incidence of typhoid fever was 0.41 per 100,000 population from 1992 to 2000 (4). The number of S. enterica Typhi isolates was always among the three most prevalent Salmonella serovars in Korea from 1998 to 2007, excluding 2002 (Table 1). In 2002, S. enterica Paratyphi A and S. enterica Braenderup were the third and fourth most prevalent respectively followed by S. enterica Typhi. During 1961-1963, S. enterica Typhi was the most dominant serovar in Daegu, Korea, showing 92.6% frequency (13).
Unlike other serovars, S. enterica Typhi infects only humans. Therefore, with good hygiene and control of healthy carriers, the incidence of typhoid fever could be decreased (4). Korea Ministry of Health has controlled typhoid fever as a Class 1 notifiable disease. KNIH receives S. enterica Typhi isolates along with the epidemiological data from medical doctors according to the Infectious Diseases Prevention Act. Vi-passive hemagglutination for preliminary test and S. enterica Typhi isolation and identification are performed with the stool and the blood culture of the patients. In addition, quarantine stations obtain stool samples from overseas travelers who come from high-risk infectious diarrheal disease areas. Regional Health & Environment Institutes then isolate and identify the pathogens from the specimens (14).
The number of S. enterica Typhi isolates has decreased gradually since 1998. Busan and Gyeongsang-do, which face the East Sea, were higher incidence areas for typhoid fever than other Korea peninsulas (4). The integron-associated multidrug-resistant (MDR) S. enterica Typhi was first identified in Korea in 1999. The MDR isolates were resistant to six antimicrobial agents that were ampicillin, chloramphenicol, trimethoprim-sulfamethoxazole, streptomycin, tetracycline, and gentamicin. All the resistance determinants, aacA4b, catB8, aadA1, dfrA1, aac(6')-IIa, and blaP2, were clustered in about a 50 kb plasmid (15). Even though most S. enterica Typhi strains are susceptible to antimicrobial agents, drugs for the treatment of typhoid fever should be chosen carefully (16). From the early 2000s, nalidixic acid resistant S. enterica Typhi isolates were also identified in Korea. The genetic relation by PFGE revealed that the nalidixic acid resistant S. enterica Typhi in Korea was closely linked to those in India, Nepal, and Bangladesh. Increased overseas travelers were one of the main reasons. From the 1990s in Korea, ciprofloxacin was recommended as the drug of choice for typhoid fever (4). Since then, ciprofloxacin has been used widely in other developing and developed countries. According to recent phage-typing study of S. enterica Typhi, major phage type transition from M1 and E1 to A occurred in Korea from 1992 to 2006 (17).
S. enterica Typhimurium is a zoonotic pathogen infecting domestic animals and causing salmonellosis in humans (18). S. enterica Typhimurium was one of the major foodborne pathogens in Korea during 1998-2007 (Table 1). It was a more serious problem because the frequency of MDR S. enterica Typhimurium human isolates increased yearly. MDR S. enterica Typhimurium definitive type (DT) 104 first emerged in Korea in 1997 (19). S. enterica Typhimurium DT104, which harbors SGI1, has been identified as a worldwide threat to human and animal health, and showed a high degree of clonality between isolates obtained from different countries (20-22). Over 50% of MDR S. enterica Typhimurium DT104 isolates during 1997-2007 in Korea were resistant to five antimicrobial agents that were ampicillin, chloramphenicol, streptomycin, sulfonamides, and tetracycline (ACSSuT) like the antibiogram of pandemic S. enterica Typhimurium DT104. During 1997-1998, there were five S. enterica Typhimurium DT104-associated foodborne-disease outbreaks nationwide (Table 2). Some S. enterica Typhimurium DT104 Korean isolates had an additional genetic arrangement of antibiotic resistance determinants with those of pandemic S. enterica Typhimurium DT104 (19). A PFGE experiment revealed that some S. enterica Typhimurium DT104 Korean isolates had an indistinguishable PFGE pattern with those of S. enterica Typhimurium DT104 isolates from American cattle (20). Even S. enterica Typhimurium swine isolates in Korea were resistant to at least 4 antimicrobial agents with class 1 integron. Among the isolates, DT104 was found by phage typing (23). Salmonella Genomic Island 1 (SGI1) in S. enterica Typhimurium DT104 chromosome harboring resistance determinants with two class 1 integrons was first identified only in S. enterica Typhimurium, but it has been discovered in other Salmonella serovars now (24), for example, S. enterica Derby (25), S. enterica Paratyphi B (26), and S. enterica Schleissheim (S. Kim, unpublished data). DT104 represented approximately 7% of phage types of all S. enterica Typhimurium human isolates. However, the major phage type was U302 (approximately 45%) (S. Kim, unpublished data).
S. enterica Enteritidis has been the most ubiquitous Salmonella serovar from diarrhea patients since 1998 in Korea. The percentage of S. enterica Enteritidis from all isolated Salmonella spp. from 1998 to 2007 was 47.5% (Table 1). This result indicated that half of the Salmonella isolates from humans were S. enterica Enteritidis. Similarly, S. enterica Enteritidis was the most prevalent serovar among the NTS serovars between 2000-2002 in the world (27). Main infection sources were poultry and eggs which were contaminated easily with S. enterica Enteritidis. Molecular epidemiological and phage typing study with S. enterica Enteritidis isolated from patients and chickens revealed that common phage types and PFGE patterns were found in both isolates. The common phage types in isolates from both patients and chickens were PT1 and PT21. Moreover, they were also the most predominant types among the isolates (28). The PFGE patterns of S. enterica Enteritidis isolates from various sources by using XbaI, SpeI, or NotI restriction enzyme were highly clonal and related (29).
In 1999, there were huge foodborne-disease outbreaks caused by S. enterica Enteritidis in Korea (Table 2). The outbreaks which resulted in more than 200 inpatients and one death, occurred by consumption of S. enterica Enteritidis contaminated boiled cockle and beef (30). In addition to these outbreaks, there were many other outbreaks caused by S. enterica Enteritidis infections in 1999. Consequently, the number of S. enterica Enteritidis isolates showed the highest peak in 1999 (Fig. 1).
Most of S. enterica Enteritidis isolates from layers were not MDR (23). However, antimicrobial resistance rate of human isolates has been increasing yearly. Resistance to clinically important antimicrobial agents such as quinolone and cephalosporine has increased in S. enterica Enteritidis isolates. Resistance rate to nalidixic acid was 21.6% which was higher than that of S. enterica Typhimurium (12.1%) (31). PT1 was the most frequent phage type among nalidixic acid resistant isolates (31). Extended spectrum β-lactamase (ESBL)-producing S. enterica Enteritidis isolates were found. The ESBL type was TEM-52 which spread clonally and horizontally in Korea (32).
There were many Salmonella outbreaks in Korea during 1998-2007. Here, I would like to introduce four outbreaks caused by rare Salmonella serovars that are worthy of note in Salmonella human infection history in Korea (Table 2). The rare Salmonella serovars mentioned in this review have not been spotlighted or ranked among the most widespread Salmonella serovars in Korea before 1998.
Salmonella enterica London had been a rare serovar in Korea as well as in the world until 1999. Until then, the outbreak patterns in Korea were traditional in that affected patients were restricted to certain areas (33). However, foodborne outbreaks occurred after 2000 and most of the affected patients were infants nationwide. Epidemiological and molecular study revealed that certain powdered milk for babies was contaminated with S. enterica London. Furthermore, the PFGE patterns of S. enterica London isolates from the powdered milk and the infant patients were indistinguishable (33). The powdered milk manufacturer received administrative penalties and recalled the powdered milk. Subsequently, infant patients decreased but human infections by S. enterica London continued to be reported until 2006. This has become a great concern. Three patients who suffered from gastroenteritis caused by S. enterica London were reported in 2004. The 3 isolates from the patients were CTX-M-14-type ESBL producing S. enterica London of which XbaI PFGE patterns were indistinguishable from those of the pathogens from powdered milk in 2000, indicating that the susceptible clone acquired the ESBL (34).
In brief, these outbreaks were triggered by massive transport of contaminated foods, a typical outbreak pattern in the present era. This S. enterica London case was the first early disease prevention by timely surveillance and the Korea PulseNet system that was started in 2000 and officially connected to PulseNet Asia-Pacific in 2006.
Salmonella enterica Paratyphi A was a rare serovar until 2001. Since 2002, S. enterica Paratyphi A has been ranked among the top 10 Salmonella serovars. S. enterica Paratyphi A is a causative pathogen for paratyphoid fever which is a Class 1 notifiable disease in Korea like typhoid fever (35). Outbreaks by this pathogen infection were not frequent in the world but were reported in India, Nepal, and Singapore (36-39). There was a big waterborne outbreak in Busan by S. enterica Paratyphi A infection in early 2002 (40). More than 200 people were hospitalized. Epidemiologists found that the water-supply system was contaminated with the bacteria. Most of the isolates were resistant to nalidixic acid. The resistance mechanism was due to the point mutation in the 83rd codon of gyrA gene as found by performing allele-specific PCR and restriction fragment length polymorphism (AS-PCR-RFLP). Recent studies showed that plasmid-mediated quinolone resistances were spreading to Enterobacteriacae, suggesting that the mechanisms of resistance to quinolone or fluoroquionolone are developing in bacteria (41).
In fact, S. enterica Infantis was not a rare serovar but steady during 1998-2007 (Table 1). It was the fifth common serovar in 2002 worldwide and had been commonly isolated from farm animals and their feed in Europe nations (27). In 2007, there was a huge outbreak caused by S. enterica Infantis infection in Jeollanam-do, a rural site in Korea (S Kim, unpublished data). Although 49 culture proven human cases were found from the outbreak, the source of contamination was not found. The antibiotic phenotype of the isolates was susceptible to 16 antimicrobial agents which were a standard set for antimicrobial test of enteric pathogens in Korean reference laboratories. Due to the outbreak, S. enterica Infantis ranked second most-frequent among serovars in 2007.
Many foodborne outbreaks arise in schools, parties, companies, and other gathering places today (44). Mass catering is rising because of increased provision of meals in public; so many people are exposed to possible foodborne diseases. An outbreak in 2007 caused by Salmonella enterica Othmarschen was such a case. In a funeral service, more than 300 mourners were exposed to contaminated foods with the pathogen and among them 72 persons became ill. The characteristics of this salmonellosis were severe diarrhea, abdominal pain, and fever. Yellow or white watery diarrhea for about 5 days with maximum 50 incidents was a typical symptom. S. enterica Othmarschen was isolated from those patients, food handlers, and foods containing eggs, squash, and seafood. The PFGE patterns of the outbreak isolates were all identical and indistinguishable from that of an American S. enterica Othmarschen isolate (45). It was very interesting that the identical clones were found in geographically distant nations even though S. enterica Othmarschen is such a rare Salmonella serovar in the world (46). All these molecular epidemiological evidences could be harvested because of the PulseNet International activities.
For the quarantine activity and early detection of contagious diseases in airports and harbors, quarantine stations carry out rectal swabs or stool sampling from overseas travelers and crew who show fever, or notify symptoms of diarrhea, abdominal pain, vomit in questionnaire sheets and come from Thailand, the Philippines, Indonesia, Vietnam, Iran, Egypt, Cambodia, and North Korea. These nations are important for cholera epidemic according to a World Health Organization report (47).
During 2004-2005, the proportion of Salmonella isolates from overseas travelers who traveled to the above eight nations was approximately 7% in total Salmonella isolates. S. enterica Weltevreden was the most frequent Salmonella serovar from overseas travelers. The frequency was 19.7%. S. enterica Anatum and S. enterica Tallahassee followed at 8.5% and 7.0%, respectively (14). These three serovars had been rare in Korea, but after 2004, S. enterica Weltevreden and S. enterica Anatum ranked in top 10 prevalent serovars in Korea. Since the early 2000s, there have been many Korean wedding tourists and travelers to Malaysia, Thailand, and other East South-Asian nations. The 3 serovars were mostly isolated from such travelers. S. enterica Weltevreden has been isolated from seafood at relatively high frequency in those nations. In Thailand, S. enterica Weltevreden had been the most prevalent serovar among Salmonella isolates from 1993 to 2002 (48). Recently, there were outbreaks caused by S. enterica Weltevreden infections in France (49), Norway, Denmark, and Finland (50). These phenomena indicated that contaminated food trades and infected travelers between nations seriously affects the health of people in a distance and a nation's health defense (51).
In this study, I showed epidemiological evidence that the incidences of S. enterica Typhi, S. enterica Enteritidis, and S. enterica Typhimurium decreased significantly in Korea during the last 10 yr since 1998. It was a very encouraging epidemiologic trend because these serovars have been health-threatening pathogens in Korea as well as the world. However, the rates of imported cases and outbreaks caused by rare serovars increased during that time. As reviewed in this study, I would like to stress that newly emerging rare Salmonella serovars should be traced and investigated to control new type pathogens in the developed world.
Figures and Tables
Fig. 1
Incidence of four serovars, S. enterica Typhi, S. enterica Paratyphi A, S. enterica Typhimurium and S. enterica Enteritidis and nontyphoidal Salmonella serovars excluding S. enterica Typhi, 1998-2007.
Source: Reference (12).
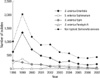
Table 1
Top 15 Salmonella serovars from foodborne and waterborne diseases and their number of isolates, 1998-2007. Bold characters represent 3 major serovars, S. enterica Typhi, S. enterica Typhimurium, and S. enterica Enteritidis. Underlined serovars show emerging serovars causing remarkable foodborne outbreaks which had been rare in Korea

Source: Reference (12).
*Total number of isolates in each year includes the number of other serovar isolates in addition to the number of top 15 serovars.
ACKNOWLEDGMENTS
I would like to thank Drs B. K. Lee, M. S. Park, and S. H. Kim for their heart warming supports.
References
1. Cho SH, Shin HH, Choi YH, Park MS, Lee BK. Enteric bacteria isolated from acute diarrheal patients in the Republic of Korea between the year 2004 and 2006. J Microbiol. 2008. 46:325–330.

2. Lee WC, Lee MJ, Kim JS, Park SY. Foodborne illness outbreaks in Korea and Japan studied retrospectively. J Food Prot. 2001. 64:899–902.

3. Centers for Disease Control and Prevention (CDC). Preliminary FoodNet data on the incidence of infection with pathogens transmitted commonly through food--10 States, United States, 2005. MMWR Morb Mortal Wkly Rep. 2006. 55:392–395.
4. Yoo S, Pai H, Byeon JH, Kang YH, Kim S, Lee BK. Epidemiology of Salmonella enterica serotype typhi infections in Korea for recent 9 years: trends of antimicrobial resistance. J Korean Med Sci. 2004. 19:15–20.
5. Chiu CH, Su LH, He CC, Jaing TH, Luo CC, Lin TY. Perforation of toxic megacolon in non-typhoid Salmonella enterocolitis spares young infants and is immune-mediated. Pediatr Surg Int. 2002. 18:410–412.
6. Tsai MH, Huang YC, Chiu CH, Yen MH, Chang LY, Lin PY, Lin TY. Nontyphoidal Salmonella bacteremia in previously healthy children: analysis of 199 episodes. Pediatr Infect Dis J. 2007. 26:909–913.

7. Skoutelis A, Gogos C, Siampi V, Dimitracopoulos G, Bassaris H. Salmonella westerstede vertebral osteomyelitis and sepsis in an immunocompetent patient. Int J Infect Dis. 2001. 5:228–229.

8. Ispahani P, Slack RC. Enteric fever and other extraintestinal salmonellosis in University Hospital, Nottingham, UK, between 1980 and 1997. Eur J Clin Microbiol Infect Dis. 2000. 19:679–687.

9. Leader BT, Frye JG, Hu J, Fedorka-Cray PJ, Boyle DS. High-throughput molecular determination of salmonella enterica serovars by use of multiplex PCR and capillary electrophoresis analysis. J Clin Microbiol. 2009. 47:1290–1299.

10. Petersen A, Aarestrup FM, Angulo FJ, Wong S, Stohr K, Wegener HC. WHO global salm-surv external quality assurance system (EQAS): an important step toward improving the quality of Salmonella serotyping and antimicrobial susceptibility testing worldwide. Microb Drug Resist. 2002. 8:345–353.
11. Park JH. Preventive medicine in times of a rapid epidemiologic transition in Korea. J Prev Med Public Health. 2006. 39:2–6.
12. Global Salm-Surv, year data viewed/Republic of Korea. World Health Organization. Accessed on 4 January 2010. Available at http://www.who.int/salmsurv/en/.
13. Chun D. A review of Salmonella and Shigella in Korea. Endemic Dis Bull Nagasaki Univ. 1964. 6:125–138.
14. Kim S, Kim SH, Chun SG, Choi ES, Lee BK. Prevalence of Salmoenlla serovars isolated from domestic residents and overseas travelers in Korea, 2004-2005. J Bacteriol Virol. 2006. 36:69–72.
15. Pai H, Byeon JH, Yu S, Lee BK, Kim S. Salmonella enterica serovar typhi strains isolated in Korea containing a multidrug resistance class 1 integron. Antimicrob Agents Chemother. 2003. 47:2006–2008.

16. Lynch MF, Blanton EM, Bulens S, Polyak C, Vojdani J, Stevenson J, Medalla F, Barzilay E, Joyce K, Barrett T, Mintz ED. Typhoid fever in the United States, 1999-2006. JAMA. 2009. 302:859–865.

17. Kim S, Kim SH, Park JH, Lee KS, Park MS, Lee BK. Clustering analysis of Salmonella enterica serovar Typhi isolates in Korea by PFGE, ribotyping, and phage typing. Foodborne Pathog Dis. 2009. 6:733–738.
18. Graziani C, Busani L, Dionisi AM, Lucarelli C, Owczarek S, Ricci A, Mancin M, Caprioli A, Luzzi I. Antimicrobial resistance in Salmonella enterica serovar Typhimurium from human and animal sources in Italy. Vet Microbiol. 2008. 128:414–418.

19. Kim S, Kim SH, Chun SG, Park MS, Lim HM, Lee BK. An additional novel antimicrobial resistance gene cluster in Salmonella genomic island 1 of a Salmonella enterica serovar Typhimurium DT104 human isolate. Foodborne Pathog Dis. 2009. 6:471–479.
20. Kim S, Chun SG, Lim OY, Park MS, Kang YH, Park YH, Lee BK. Genomic relationship of Salmonella enterica serovar Typhimurium DT104 isolates from Korea and the United States. J Microbiol. 2004. 42:14–19.
21. Ribot EM, Wierzba RK, Angulo FJ, Barrett TJ. Salmonella enterica serotype Typhimurium DT104 isolated from humans, United States, 1985, 1990, and 1995. Emerg Infect Dis. 2002. 8:387–391.

22. Helms M, Ethelberg S, Molbak K. International Salmonella Typhimurium DT104 infections, 1992-2001. Emerg Infect Dis. 2005. 11:859–867.
23. Yang SJ, Park KY, Kim SH, No KM, Besser TE, Yoo HS, Kim SH, Lee BK, Park YH. Antimicrobial resistance in Salmonella enterica serovars Enteritidis and Typhimurium isolated from animals in Korea: comparison of phenotypic and genotypic resistance characterization. Vet Microbiol. 2002. 86:295–301.

24. Levings RS, Lightfoot D, Partridge SR, Hall RM, Djordjevic SP. The genomic island SGI1, containing the multiple antibiotic resistance region of Salmonella enterica serovar Typhimurium DT104 or variants of it, is widely distributed in other S. enterica serovars. J Bacteriol. 2005. 187:4401–4409.

25. Vo AT, van Duijkeren E, Fluit AC, Wannet WJ, Verbruggen AJ, Maas HM, Gaastra W. Antibiotic resistance, integrons and Salmonella genomic island 1 among non-typhoidal Salmonella serovars in The Netherlands. Int J Antimicrob Agents. 2006. 28:172–179.

26. Huehn S, Helmuth R, Bunge C, Guerra B, Junker E, Davies RH, Wattiau P, van Pelt W, Malorny B. Characterization of pathogenic and resistant genome repertoire reveals two clonal lines in Salmonella enterica subsp. enterica serovar Paratyphi B (+)-tartrate positive. Foodborne Pathog Dis. 2009. 6:431–443.
27. Galanis E, Lo Fo Wong DM, Patrick ME, Binsztein N, Cieslik A, Chalermchikit T, Aidara-Kane A, Ellis A, Angulo FJ, Wegener HC. World Health Organization Global Salm-Surv. Web-based surveillance and global Salmonella distribution, 2000-2002. Emerg Infect Dis. 2006. 12:381–388.
28. Kim SH, Kim S, Chun SG, Park MS, Park JH, Lee BK. Phage types and pulsed-field gel electrophoresis patterns of Salmonella enterica serovar Enteritidis isolated from humans and chickens. J Microbiol. 2008. 46:209–213.

29. Chung YH, Kwon YI, Kim SY, Kim SH, Lee BK, Chang YH. Antimicrobial susceptibilities and epidemiological analysis of Salmonella enteritidis isolates in Korea by phage typing and pulsed-field gel electrophoresis. J Food Prot. 2004. 67:264–270.

30. Kim JR, Lee SW, Kim HB, Cha J, Lee KH, Bae KW. An epidemiological investigation on the mode of transmission of the lethal salmonellosis outbreak in Hamyang County. Korean J Epidemiol. 1999. 21:185–194.
31. Choi SH, Woo JH, Lee JE, Park SJ, Choo EJ, Kwak YG, Kim MN, Choi MS, Lee NY, Lee BK, Kim NJ, Jeong JY, Ryu J, Kim YS. Increasing incidence of quinolone resistance in human non-typhoid Salmonella enterica isolates in Korea and mechanisms involved in quinolone resistance. J Antimicrob Chemother. 2005. 56:1111–1114.

32. Lee K, Yong D, Yum JH, Kim HH, Chong Y. Diversity of TEM-52 extended-spectrum beta-lactamase-producing non-typhoidal Salmonella isolates in Korea. J Antimicrob Chemother. 2003. 52:493–496.
33. Kim S, Lee BK, Kang YH, Nam HJ, Lim OY, Seok WS, Park JK. A virulent strain of Salmonella enterica serovar London isolated in infants with enteritis traced by active surveillance and molecular epidemiological study. J Korean Med Sci. 2003. 18:325–330.

34. Yong D, Lim YS, Yum JH, Lee H, Lee K, Kim EC, Lee BK, Chong Y. Nosocomial outbreak of pediatric gastroenteritis caused by CTX-M-14-type extended-spectrum beta-lactamase-producing strains of Salmonella enterica serovar London. J Clin Microbiol. 2005. 43:3519–3521.
35. Kapil A, Sood S, Reddaiah VP, Das B, Seth P. Paratyphoid fever due to Salmonella enterica serotype Paratyphi A. Emerg Infect Dis. 1997. 3:407.

36. Bhatta DR, Bangtrakulnonth A, Tishyadhigama P, Saroj SD, Bandekar JR, Hendriksen RS, Kapadnis BP. Serotyping, PCR, phage-typing and antibiotic sensitivity testing of Salmonella serovars isolated from urban drinking water supply systems of Nepal. Lett Appl Microbiol. 2007. 44:588–594.

37. Goh YL, Puthucheary SD, Chaudhry R, Bhutta ZA, Lesmana M, Oyofo BA, Punjabi NH, Ahmed A, Thong KL. Genetic diversity of Salmonella enterica serovar Paratyphi A from different geographical regions in Asia. J Appl Microbiol. 2002. 92:1167–1171.

38. Sood S, Kapil A, Dash N, Das BK, Goel V, Seth P. Paratyphoid fever in India: An emerging problem. Emerg Infect Dis. 1999. 5:483–484.

39. Teoh YL, Goh KT, Neo KS, Yeo M. A nationwide outbreak of coconut-associated paratyphoid A fever in Singapore. Ann Acad Med Singapore. 1997. 26:544–548.
40. Kim S, Lim OY, Kim SH, Kim JY, Kang YH, Lee BK. Pulsed-field gel electrophoresis and mutation typing of gyrA gene of quinolone-resistant Salmonella enterica serovar Paratyphi A isolated from outbreak and sporadic cases, 1998-2002, Korea. J Microbiol Biotechnol. 2003. 13:155–158.
41. Tamang MD, Seol SY, Oh JY, Kang HY, Lee JC, Lee YC, Cho DT, Kim J. Plasmid-mediated quinolone resistance determinants qnrA, qnrB, and qnrS among clinical isolates of Enterobacteriaceae in a Korean hospital. Antimicrob Agents Chemother. 2008. 52:4159–4162.

42. Dimitrov T, Udo EE, Albaksami O, Kilani AA, Shehab el-DM. Ciprofloxacin treatment failure in a case of typhoid fever caused by Salmonella enterica serotype Paratyphi A with reduced susceptibility to ciprofloxacin. J Med Microbiol. 2007. 56:277–279.

43. Joshi S, Amarnath SK. Fluoroquinolone resistance in Salmonella typhi and S. paratyphi A in Bangalore, India. Trans R Soc Trop Med Hyg. 2007. 101:308–310.

44. Scott E. Food safety and foodborne disease in 21st century homes. Can J Infect Dis. 2003. 14:277–280.
45. Kim S, Choi YG, Eom JW, Oh TJ, Lee KS, Kim SH, Lee ET, Park MS, Oh HB, Lee BK. An outbreak of Salmonella enterica serovar Othmarschen at a funeral service in Guri-si, South Korea. Jpn J Infect Dis. 2007. 60:412–413.
46. Morosini MI, Blázquez J, Negri MC, Cantón R, Loza E, Baquero F. Characterization of a nosocomial outbreak involving an epidemic plasmid encoding for TEM-27 in Salmonella enterica subspecies enterica serotype Othmarschen. J Infect Dis. 1996. 174:1015–1020.

47. Deen JL, von Seidlein L, Sur D, Agtini M, Lucas ME, Lopez AL, Kim DR, Ali M, Clemens JD. The high burden of cholera in children: comparison of incidence from endemic areas in Asia and Africa. PLoS Negl Trop Dis. 2008. 2:e173.

48. Bangtrakulnonth A, Pornreongwong S, Pulsrikarn C, Sawanpanyalert P, Hendriksen RS, Lo Fo Wong DM, Aarestrup FM. Salmonella serovars from humans and other sources in Thailand, 1993-2002. Emerg Infect Dis. 2004. 10:131–136.
49. D'Ortenzio E, Weill FX, Ragonneau S, Lebon JA, Renault P, Pierre V. First report of a Salmonella enterica serovar Weltevreden outbreak on Reunion Island, France, August 2007. Euro Surveill. 2008. 13:pii: 18949.
50. Emberland KE, Ethelberg S, Kuusi M, Vold L, Jensvoll L, Lindstedt BA, Nygard K, Kjelso C, Torpdahl M, Sorensen G, Jensen T, Lukinmaa S, Niskanen T, Kapperud G. Outbreak of Salmonella Weltevreden infections in Norway, Denmark and Finland associated with alfalfa sprouts, July-October 2007. Euro Surveill. 2007. 12:E071129.4.

51. Swaminathan B, Gerner-Smidt P, Ng LK, Lukinmaa S, Kam KM, Rolando S, Gutierrez EP, Binsztein N. Building PulseNet International: an interconnected system of laboratory networks to facilitate timely public health recognition and response to foodborne disease outbreaks and emerging foodborne diseases. Foodborne Pathog Dis. 2006. 3:36–50.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download