INTRODUCTION
Mucoepidermoid carcinoma (MEC) most commonly occurs in salivary glands but can also be seen at other organs, including lung, esophagus, breast, pancreas, and thyroid gland (1-10). Primary MEC of the thyroid is very rare and its origin has not been fully understood with debate regarding whether it arises from solid cell nests of ultimobranchial apparatus or from follicular epithelium (5, 7, 10-13). Here, we present a case of unusual tumor of thyroid MEC more suggesting solid cell nest origin than follicular epithelium.
CASE REPORT
A 50-yr-old man presented with a 3-month history of a mass on the left side of his neck, which had recently increased in size on March 26, 2009.
Physical examination showed a firm, fixed mass measuring 3.0×2.5 cm. Ultrasonography and neck CT scan revealed a mass with irregular border in left lobe of thyroid gland and multiple enlargements of cervical lymph nodes. No other abnormalities were seen. Total thyroidectomy was performed. Grossly, the left lobe was almost entirely replaced by en pale yellow to tan solid mass measuring 3.0×2.5×2.0 cm. The mass was not encapsulated and showed infiltrative margin. The right lobe and the isthmus were soft tan to red without any abnormality.
On microscopic examination, the tumor did not have fibrous capsule and infiltrated into surrounding soft tissue. The tumor was composed of follicular variant of papillary carcinoma and mucoepidermoid carcinoma. They were focally intermingled and showed transition from papillary carcinoma to squamous epithelium arranged in sheets (Fig. 1A). Papillary carcinoma tumor cells showed nuclear groove, ground glass nucleus and nuclear pseudoinclusion (Fig. 1B). Mucoepidermoid carcinoma revealed three cell types: columnar cells, mucocytes and squamous cells (Fig. 1C). Columnar cells made ductal or cystic structures and contained eosinophilic material. Some columnar cells in tumor glands showed cilia (Fig. 1D). Squamoid cells showing cytoplasmic keratinization and intercellular bridge were present in solid sheets. Alcian blue and PAS positive mucocytes were mixed with columnar and squamous cells. Eosinophilic material in ductal or cystic structures was also positive for alcian blue and PAS stains (Fig. 1E). Columnar and squamous tumor cells showed mild to moderate nuclear atypia with rare mitosis. A few aggregates of small cysts lined by benign ciliated respiratory epithelial cells and containing mucoid material are seen at the periphery of the tumor (Fig. 1F).
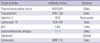
Immunohistochemical analysis was done with commercially prepared antibody panel (Table 1, Fig. 2) using EnVison Plus-HPR detection kit (Dako, Glostrup, Denmark). Papillary carcinoma cells were positive for thyroid transcription factor (TTF-1), thyroglobulin, galectin-3 and cytokeratin 19 and negative for p63, CEA and calcitonin. Squamoid and columnar cells in MEC were positive for pancytokeratin and CEA and negative for calcitonin, TTF-1, thyroglobulin, galectin-3 and cytokeratin 19. Squamoid cells and basal cells of ductal and cystic structures were positive for p63. Benign ciliated respiratory epithelial cells were CEA positive and thyroglobulin negative. The diagnosis of thyroid mucoepidermoid carcinoma combined with follicular variant of papillary carcinoma was made. Dissected neck lymph nodes revealed metastatic mucoepidermoid carcinoma. Four months after the operation, he received radiation therapy and presented dyspnea and wheezing.
DISCUSSION
MEC of the thyroid gland is a rare tumor and is characterized by unique histologic appearance and indolent biologic behavior. It was first described in 1977 by Rhatigan et al. (14) and they considered it to originate from ectopic salivary gland tissue but they couldn't find any remnants of salivary gland tissue. Its pathogenesis has remained unclear. Many authors have suggested that these tumors develop from solid cell nests (SCN), known to be remnants of ultimobranchial body (diverticulum from the fourth pharyngeal pouch), whereas some authors have reported a follicular origin (5, 7, 10-13). SCN is irregular structures of about 1 mm in maximal diameter and usually found in the thyroid lateral lobes. It is basically composed of non-keratinizing squamous cells and ductal structures lined by ciliated columnar epithelium (15). Ando et al. (10) reported MEC showing ductal structures lined by markedly ciliated columnar cells, resembling respiratory epithelial cells. The ductual structures in SCN of the ultimobranchail body also lined with ciliated epithelium and this suggests that SCN might be origin of MEC. And that is the reason tumor cells are p63 positive and TTF-1 and thyroglobulin negative. P63 is a marker of stem cell phenotype and TTF-1 and thyroglobulin are markers of thyroid follicular epithelium. These immunohistochemical results may be helpful in distinguishing ultimobranchial-derived SCN from their mimics such as squamous metaplasia of follicular cell origin tumor and metastatic squamous cell carcinoma. Although ciliated epithelium can be seen on the inner surface of thyroglossal cyst remnant but it is located on the midline. Only one another case reported by Wenig et al. (7) had focal ciliated epithelium lining cysts but that was seen in an integral parts of the neoplastic proliferation associated with squamous foci.
There are several literatures supporting a follicular epithelial origin of MEC. MEC occasionally has concurrent papillary carcinoma and histologic analysis suggests that preexisting PTC may undergo squamous and mucinous metaplasia to give rise to MEC (13, 16). MEC tumor cells are positive for thyroglobulin staining and it has been used support the follicular origin of MEC.
The present tumor is pathologically unique in that it showed ductal structures lined with ciliated columnar cells, resembling respiratory epithelium and p63 positivity suggesting SCN origin and composite papillary carcinoma component suggesting follicular origin of MEC. These findings suggest that the origin of the tumor could be stem cells of SCN and they differentiate toward MEC and papillary carcinoma. BRAF gene mutation was detected in SCN and papillary carcinoma and it was considered as the evidence of a histogenetic relation between SCN and papillary carcinoma (17). There are very limited reports about BRAF gene mutation in MEC and Trovisoco et al. (18) reported that BRAF gene mutation was not found in MEC. In this case, BRAF gene mutation was found both in PTC and MEC (not mentioned in result) but serial sections for microdissection lost SCN. More investigations of PTC, MEC and SCN at the molecular level would be helpful to find out their pathogenesis.
Clinically, thyroid MEC is most often found in female with a ratio that approximates 2:1. Although it has been described as indolent tumors with low-grade malignant potential, some reports have indicated a less favorable behavior of combined other type of carcinoma, especially with foci of undifferentiated carcinoma (19, 20). Our patient presented with combined follicular variant of papillary carcinoma and MEC and metastatic foci in cervical lymph nodes were exclusively MEC. Miranda et al. (13) reported a case of composite follicular variant of papillary carcinoma and mucoepidermoid carcinoma which showed regional lymph node metastasis. To expect the prognosis of mucoepidermoid carcinoma combined with other type of tumor, we need to find more cases.
This is the second report of MEC of thyroid gland showing ciliated glandular cells and also the second report of composite follicular variant of papillary carcinoma and mucopidermoid carcinoma of thyroid gland. These histologic and immunohistochemical findings suggest that MCE is originated from SCN rather than follicular epithelium.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download