Abstract
This study aims to investigate the factors related to the adoption of clinical practice guidelines in clinical settings in Korea; it also aims to determine how these factors differ depending on the specific situation of health care system and professional climate. The research sample comprised physicians who are board members of academic societies with experiences in development of clinical practice guidelines using a convenient sampling. We analyzed 324 physicians with pooling two-year sample of 2007 and 2008. From all the respondents, 48.8% stated that they followed Clinical Practice Guidelines, and 93.4% agreed with the content in the Clinical Practice Guidelines. With regard to the item on the self-efficacy of practicing guidelines, 90.3% of the respondents selected 'low level'. In the regression analysis, the factors associated with implementation were level of recognition, agreement and self-efficacy and positive attitude towards practice guidelines. Although the health care system in Korea differs from those in Western countries, our results revealed that the factors related to the adoption of practice guidelines were similar to the research results of Western countries. These results suggest that professionals' attitudes towards clinical practice guidelines are universal, and implementation strategies should be developed globally.
Clinical practice guidelines (CPGs) are considered as one of the most powerful and effective tools for the promotion of evidence-based medicine (EBM) (1). CPGs are expected to reduce medical costs by minimizing unnecessary variations in treatment and improve the outcome of patient care (2), and an analysis of empirical studies has confirmed their effectiveness (3). Many countries have been actively promoting the development of CPGs through the provision of financial and administrative support (4). In Korea, various academic associations have been developing CPGs independently and sporadically. In 2006, the Korean Academy of Medical Sciences (KAMS), which represents 130 medical academic societies, reported that 52 CPGs have been developed in Korea to the date, and since 2007, the Korean Ministry for Health, Welfare and Family Affairs has been providing KAMS with financial support for the development and implementation of CPGs by professional groups. As a result, KAMS has directed the development and dissemination of EBM-based CPG for asthma, depression, and breast cancer.
Despite efforts to encourage them, several studies have reported that CPG implementation at clinical sites remains low (5, 6). According to Farquhar et al., clinicians view CPGs as anti-intellectual, standardizing practice at around average levels, preventing discretion in individual cases, cost-cutting, limiting innovation and clinical freedom, and encouraging litigation; and these negative attitudes are critical barriers toward CPG implementation (7). Representative groups of Korean physicians such as the Korean Medical Association have adopted a skeptical or negative attitude toward CPG. In particular, their belief is that CPG are often used as a basis of retrenchment in insurance claims and lead to an increase in regulations, which limit their flexible use for the diversely different situations encountered in clinical practice.
CPGs can be difficult to apply, and the use of CPGs by physicians in clinical practice has not been sufficiently studied (8). In order to promote CPG implementation, the factors that affect clinicians' resistance toward them must be identified and addressed. Several previous studies have investigated the relationship between CPG implementation and clinician attitudes (9) and reported associations between clinician attitude toward CPGs and clinician characteristics (10), patient characteristics (11), and the passage of time (12).
Cabana et al. (13-15) have aimed to identify specific barrier factors to CPGs implementation, including lack of awareness and familiarity toward CPG, lack of agreement, lack of self-efficacy, lack of outcome expectancy, inertia of previous practice, and care environment. In applying this theoretical model to a survey of 829 pediatricians, factors such as lack of agreement, lack of self-efficacy, and lack of outcome expectancy were found to be negatively associated with CPG implementation (16). Although their research was successful in expanding the explanatory power for the CPG compliance-related factors beyond the variables of clinician attitudes, they did not include these variables in their analytic model with an integration of such variables still unresolved.
Furthermore, previous studies have primarily been carried out in Western countries, where healthcare practices and attitudes differ from Korea. The present study aims to develop a comprehensive analysis model that includes both clinician attitudes toward CPGs and barriers to CPG implementation. As a secondary objective, we have attempted to determine whether the attitudes and barriers affecting CPG implementation remain similar across countries with different cultures and healthcare systems.
In this study, academic society members with experience in CPG development were surveyed using a self-administered questionnaire and this research sample was selected through a convenient sampling method. The reason to adopt this sampling method was that the response rates for surveys on physicians were below 10% in Korea and it was difficult to secure an adequate size of sample. Moreover, the CPG development is not a well-known agenda in Korea; thus using a conventional sampling approach such as a random sampling on entire physicians would lead to low response rate due to their low concern about CPG. Therefore, conducting the survey on physician groups with appropriate understanding of this issue was thought to be effective, and medical doctors involved in administrative affairs of the academic societies rather than general members of the societies were ultimately chosen as the research target.
As a result of investigating experience in CPG development among the KAMS members in 2006, 14 out of the entire 130 academic society members had the experience. Among the board members of these academic societies, 226 physicians who agreed to participate in our investigation responded to survey in 2007. In 2008, board members of five additional academic societies with experienced in CPG development were surveyed with the same survey instrument as 2007 and 98 responses of physicians were collected.
Subsequently, a univariate analysis was performed to identify the systematic difference in the socio-demographic characteristics of respondents and attitudes toward CPGs between the data collected in 2007 and 2008. As a result of the analysis, differences were not observed between them, and the data from all 324 questionnaires were pooled for further analysis.
SPSS v.14.0 was used for statistical analysis in this study, and the relationships between socio-demographic characteristics, and attitudes and outcome expectancies toward CPGs were analyzed using t-test and ANOVA. Correlations between factors affecting CPG implementation were examined by multiple regression analysis.
Survey instruments included basic demographic information of respondents as well their degree of awareness and familiarity, attitude, self-efficacy, and implementation of CPGs. Among the survey items, questions regarding CPG implementation status and reasons were based on the study by Cabana et al. (5), and those regarding attitudes toward CPGs were directly adopted from the study by Tunis et al. (9). The barrier factors affecting CPG implementation such as degree of awareness and familiarity, attitude, self-efficacy, and outcome expectancy were measured on a five-point Likert scale as in previous studies (14-16).
All data were collected without individual identification in this study. Also, we did not get additional consents from the respondents because we described the research purpose and the request of cooperation in questionnaire and we assumed that reply of the questionnaires meant the respondent's agreement. This research was reviewed by the Institutional Review Board at Ewha Womans University Medical Center and was given exemption from the deliberation (ECT-226-6).
The socio-demographic characteristics of respondents are shown (Table 1). Of the 324 respondents, 81.3% were males, 42.0% were in the age group ranging from 20 to 39 yr, and 44.3% had 10-19 yr of clinical experience. Specialty physicians accounted for 96.9% of respondents, and 76.1% of respondents were employed by private healthcare institutions. In addition, 93.4% of respondents were employed by institutions providing residency training, and 67.9% of respondents belonged to university hospitals.
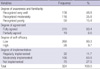
The level of awareness and familiarity with CPGs and CPG implementation are shown (Table 2). While 48.8% of respondents recognized CPGs very well, 15.4% were not familiar with CPGs. When asked how much they agreed with CPGs, the great majority of respondents (93.4%) fully agreed with the contents of CPGs. In terms of self-efficacy, which indicates one's ability to apply CPGs, 90.3% of respondents rated their level of self-efficacy as low. Only 11.7% of respondents implemented CPGs regularly, and 60.8% implemented CPGs to a moderate degree.
In the analysis of outcome expectancy of CPGs (Table 3), positive responses were observed for items of quality improvement in patient care (82.2%) and improvement in systematic education and communication (75.9%). In contrast, negative responses were observed in items of decrease in malpractice suits (25.0%), decrease in defensive medical practice (19.3%), and increase in physician satisfaction (15.4%).
In examining clinicians' attitude toward positive aspects of CPGs, the items of unbiased synthesis of expert opinions had the highest agreement (86.4%), followed by convenient source of advice (84.6%) and intended to improve the quality of care (83.1%). With regard to negative aspects of CPGs, intended to use as a utilization review tool had the highest agreement (69.3%), followed by too rigid to apply to individual patients (59.0%) and oversimplified or 'cookbook' medicine (59.0%). In general, the level of agreement was higher for positive aspects of CPGs than for negative aspects. These results are shown in Table 3.
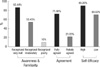
Fig. 1 illustrates CPG implementation level on the basis of respondents' degree of awareness and familiarity, agreement, and self-efficacy. The respondents who were highly aware of and familiar with CPGs showed a higher level of CPG implementation (85.4%) than those who moderately or poorly recognized CPGs. Respondents who fully agreed with CPGs also showed a higher level of CPG implementation (71.5%) than those who only partially agreed with CPGs (21.1%). Similarly, respondents who perceived high self-efficacy in CPGs showed higher CPG implementation (89.3%) than those who perceived low self-efficacy in CPGs.
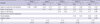
A regression analysis was performed using various factors discussed above in order to determine the factor that had the greatest impact on CPG implementation (Table 4). Socio-demographic variables and environmental factors including gender, age, period of clinical experience, type of medical occupation, clinical location, clinic ownership, clinical training provision, and clinical setting were included in the model as control variables. In Model 5, where all the variables affecting CPG implementation are included, CPG implementation was shown to be high for respondents with a high level of awareness and familiarity, agreement, and self-efficacy (R2=0.25). Subsequently, major variables were supplemented in phases, and variations in R2 were examined to test the influence of each variable (Models 1-4). Respondents' degree of awareness and familiarity with CPG had the highest influence, followed by agreement, positive attitude, and self-efficacy.
The results of present study showed that the degree of awareness and familiarity and agreement with CPGs was very high among our respondents. In contrast, the degree of self-efficacy in implementing CPGs was relatively low. Overall, 84.6% of respondents were aware of CPGs; however, only 48.8% of the total respondents claimed to recognize CPGs very well. This finding is similar to that of a previous study conducted in Ontario, in which 86% of the physicians surveyed were familiar with CPGs, but only 5% were familiar with the details of CPGs (17). These results suggest that publicity and activities aimed at actively delivering the detailed contents of CPGs are the most important for facilitating of CPG implementation, because physicians are lacking in detailed knowledge regarding CPGs rather than awareness of CPGs in general. Our identification of low self-efficacy in implementing CPGs as a major problem of implementation is also consistent with previous studies which have reported that the specific skills required for CPG implementation at clinical sites are relatively lower than physicians' awareness of and familiarity with CPGs (16, 18, 19). Therefore, comprehensive practice manuals should be provided to clinicians to promote their familiarity with new guidelines.
The highly expected outcomes of CPGs included the items of 'increase in the quality of patient care' and 'improvement in systematic education and communication', and outcome expectancy among independent or group practice clinicians was higher than among clinicians employed by university hospitals. This disparity may be due to independent or group practice clinicians having less access to systematic support for medical decisions in the provision of patient care, and it indicates the importance of meeting the demand of these clinicians. We observed CPG implementation to be quite high, with 72.5% of respondents regularly or moderately implementing CPGs. However, clinicians regularly implementing CPGs account for only 11.7% of the entire sample, and thus, the systematic and routine use of CPGs remains low. Similar findings have been previously reported (20). Several studies have reported that the mere development and dissemination of CPGs could rarely lead to changes in clinical practice (20-23). And the present study supports these reports.
Overall, in this study, positive attitudes were more prevalent than negative attitudes toward CPGs. However, compared to other studies (10, 24) that adopted the same survey instruments concerning clinicians' attitude toward CPGs (9), we observed a similar rate of response for positive aspects but higher response rates for negative aspects in the present study. Physician attitudes toward CPGs are affected by the socio-cultural characteristics and healthcare systems of their country. And this result indicates that Korean clinicians remain highly concerned about the negative influence of CPGs. Korean clinicians have long been apprehensive of the Korea Republic of Government applying a strong regulation policy toward CPGs in light of their previous experience with the national health insurance system, which operates under strong cost containment regulations. A survey of Canadian oncologists' attitudes toward CPGs also found that their perception as being intended to reduce healthcare costs was the most prevalent negative attitude toward CPGs (10). Therefore, regulatory agencies' ability to reach an appropriate compromise between service quality and cost containment is necessary to enhance CPG compliance.
Furthermore, the present study included attitude variables toward CPGs and confirmed that CPG implementation is high when positive attitudes are dominant (10). Because it includes both barrier factors and attitude variables, the regression model established in the present study is by far the most comprehensive model for the analysis of factors related to CPGs, and this study has verified that these factors are relevant to CPG implementation.
Although this study has produced meaningful results, it has several limitations. The primary limitation of this study is that data were collected through convenient sampling, leading to the problem of representativeness. Clinicians were not generally cooperative toward participating in the survey, and this study was based only on the responses of those who were willing to participate. The clinicians who participated in the survey were more likely to be familiar with CPG development than those who did not, indicating that the findings of this study may not be representative of the general consensus of all clinicians in Korea. In support of this hypothesis, we observed higher recognition levels and positive attitudes toward CPGs than anticipated. Nevertheless, the negative concerns and low level of self-efficacy and knowledge reported by clinicians surveyed in this study indicate that education programs are necessary for Korean clinicians on the importance and benefits of CPGs. Additionally, the survey instrument was originally developed in another language, and data from 2 yr were pooled for analysis because of similarity of responses across the 2 yr. The effect of translation and the discrepancy in response time may also be pointed out as limitations of the present study. In the future, research on CPGs should be conducted on a more representative sample, and studies should examine whether physicians in different socio-cultural settings show similar propensities toward CPG.
Clinician's awareness and familiarity, agreement, and self-efficacy in implementing CPGs and the prevalence of positive attitudes toward CPGs have been consistently identified as important factors affecting CPG implementation. And the present study has further verified through the development of a comprehensive assessment tool that addresses both barriers and attitudes toward CPGs. Most of previous studies regarding CPGs were conducted in Western countries, and the similarity of the findings of this Korean study may imply that the aforementioned variables are globally identifiable factors independent of sociocultural characteristics and healthcare systems. Furthermore, we have shown that global principles in the promotion of CPG implementation and propagation can be established. Sharing the results of detailed propagation strategies attempted by various countries will aid in the continuous improvement of CPG implementation methods.
Figures and Tables
References
1. Wolff M, Bower DJ, Marbella AM, Casanova JE. US family physicians' experiences with practice guidelines. Fam Med. 1998. 30:117–121.
2. Drake RE, Goldman HH, Leff HS, Lehman AF, Dixon L, Mueser KT, Torrey WC. Implementing evidence-based practices in routine mental health services settings. Psychiatr Serv. 2001. 52:179–182.
3. Grimshaw JM, Russell IT. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet. 1993. 342:1317–1322.

4. Burgers JS, Grol R, Klazinga NS, Mäkelä M, Zaat J. ACREE Collaboration. Towards evidence-based clinical practice: an international survey of 18 clinical guideline programs. Int J Qual Health Care. 2003. 15:31–45.

5. Flores G, Lee M, Bauchner H, Kastner B. Pediatricians' attitudes, beliefs, and practices regarding clinical practice guidelines: a national survey. Pediatrics. 2000. 105:496–501.

6. Scott IA, Buckmaster ND, Harvey KH. Clinical practice guidelines: perspectives of clinicians in Queensland public hospitals. Intern Med J. 2003. 33:273–279.

7. Farquhar CM, Kofa EW, Slutsky JR. Clinicians' attitudes to clinical practice guidelines: a systematic review. Med J Australia. 2002. 177:502–506.

8. Mottur-Pilson C. Internists' evaluation of guidelines: the IMCARE Practice Guidelines Network. Int J Qual Health Care. 1995. 7:31–37.

9. Tunis SR, Hayward RS, Wilson MC, Rubin HR, Bass EB, Johnston M, Steinberg EP. Internists' attitudes about clinical practice guidelines. Ann Intern Med. 1994. 120:956–963.

10. Graham ID, Beardall S, Carter AO, Tetroe J, Davies B. The state of the science and art of practice guideline development, dissemination and evaluation in Canada. J Eval Clin Pract. 2003. 9:195–202.
11. Dickey B, Normand SL, Eisen S, Hermann R, Cleary P, Cortés D, Ware N. Associations between adherence to guidelines for antipsychotic dose and health status, side effects, and patient care experiences. Med Care. 2006. 44:827–834.

12. Inouye J, Kristopatis R, Stone E, Pelter M, Sandhu M, Weingarten S. Physicians' changing attitudes toward guidelines. J Gen Intern Med. 1998. 13:324–326.

13. Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, Rubin HR. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999. 282:1458–1465.

14. Cabana MD, Flores G. The role of clinical practice guidelines in enhancing quality and reducing racial/ethnic disparities in paediatrics. Paediatr Respir Rev. 2002. 3:52–58.

15. Cabana MD, Kim C. Physician adherence to preventive cardiology guidelines for women. Women's Health Issues. 2003. 13:142–149.

16. Cabana MD, Rand CS, Becher OJ, Rubin HR. Reasons for pediatrician nonadherence to asthma guidelines. Arch Pediatr Adolesc Med. 2001. 155:1057–1062.

17. Rosser WW, Palmer WH. Dissemination of guideline on cholesterol. Canadian Family Physician. 1993. 39:280–284.
18. Wechsler H, Levine S, Idelson RK, Rohman M, Taylor JO. The physician's role in health promotion- a survey of primary care practiotioners. N Engl J Med. 1983. 308:97–100.
19. Ammerman AS, DeVellis RF, Carey TS, Keyserling TC, Strogatz DS, Haines PS, Simpson RJ Jr, Siscovick DS. Physician-based diet counseling for cholesterol reduction: current practices, determinants, and strategies for improvement. Prev Med. 1993. 22:96–109.

20. Lomas J, Anderson GM, Domnick-Pierre K, Vayda E, Enkin MW, Hannah WJ. Do practice guidelines guide practice? The effect of a consensus statement on the practice of physicians. N Engl J Med. 1989. 321:1306–1311.
21. Mittman BS, Tonesk X, Jacobson PD. Implementing clinical practice guidelines: social influence strategies and practitioner behavior change. QRB Qual Rev Bull. 1992. 18:413–422.

22. Main DS, Cohen SJ, DiClemente CC. Measuring physician readiness to change cancer screening: preliminary results. Am J Prev Med. 1995. 11:54–58.

23. Meyers DG, Steinle BT. Awareness of consensus preventive medicine practice guidelines among primary care physicians. Am J Prev Med. 1997. 13:45–50.

24. Hayward RS, Guyatt GH, Moore KA, McKibbon KA, Carter AO. Canadian physicians' attitudes about and preferences regarding clinical practice guidelines. CMAJ. 1997. 156:1715–1723.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download