Abstract
An 84 yr-old male with a history of nausea and vomiting for 3 weeks was admitted to our hospital. Esopahgogastroduodenoscopy showed the diffuse infiltrative type of gastric cancer encircling from the cardia to the lower body. On abdominal computerized tomography, the gastric wall was diffusely thickened with overlying mucosal enhancement without lymph node involvement. Histologic examination revealed poorly differentiated adenocarcinoma. So surgical resection was planned. However, patient refused all medical care, and then he was discharged. He lived without any medical support and then he revisited our hospital and showed relieved symptoms on the follow-up exam. On esophagogastroduodenoscopy, the gastric mucosa of the body looked normal without any dysplastic change. Abdominal CT revealed a decreased thickening of the gastric wall of the body. The histology from the endoscopic forceps biopsy showed no evidence of malignancy. The patient is alive without any sign of tumor recurrence after 14 months.
Spontaneous regression of a malignant tumor is very rare. It has been estimated that this occurs less than once in 60,000 to 100,000 people with cancer and about 20 such cases have been reported annually (1, 2). Spontaneous regression of a malignant tumor has often noted in hypernephroma, neuroblastoma, malignant melanoma, choriocarcinoma, bladder cancer, but this is extremely rare for stomach cancer (3). We recently experienced a case of spontaneous regression of advanced gastric cancer, Borrmann type IV, and we report on our case along with a review of the related literature.
An 84 yr-old male with a history of nausea and vomiting for the previous 3 weeks was admitted to our hospital. He used no medicine or herbal material except for an oral hypoglycemic agent for diabetes mellitus for 10 yr. His vital signs were stable and the physical examination revealed a palpable mass at the epigastrium. On laboratory examination, the WBC was 7,630/µL, the hemoglobin level was 14.2 g/dL, platelet 194,000/µL, fasting glucose 140 mg/dL, blood urea nitrogen 24.6 mg/dL, creatinine 1.25 mg/dL, total protein 6.62 g/dL, albumin 3.49 g/dL, AST 18 IU/L, ALT 13 IU/L, total bilirubin 0.41 mg/dL, direct bilirubin 0.18 mg/dL, alkaline phosphatase 126 IU/L, γ-GTP 11 IU/L, the prothrombin time (INR) was 1.0 and the activated partial thromboplastin time was 23.0 sec.
Esophagogastroduodenoscopy (EGD) showed rugal fold thickening and widening along the whole length of the gastric body. The mucosa was congested and it looked dysplastic. When touched with biopsy forceps, the mucosa showed friability and bleeding to easy touch (Fig. 1). Since the time of discharge, he took famotidine and itopride HCL without any other medication or herbal medication and he revisited our hospital for follow up 6 months later. EGD showed that the gastric folds were well distended by air inflation and the mucosa looked normal at the previously dysplastic and friable areas from the cardia to the lower body (Fig. 2).
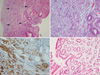
Abdominal computerized tomography (CT) revealed diffuse irregular wall thickening and mucosal enhancement from the cardia to the lower body. Perigastric infiltration was present, yet lymph node enlargement or distant metastatic lesion was not identified (Fig. 3A). Multiple pieces of mucosal biopsy were obtained and the histological examination showed poorly differentiated adenocarcinoma (Fig. 4A-C). Malignant cells were stained at Periodic acid Schiff (PAS) stain and immunohistochemical stain was positive for cytokeratin AE1/AE3 and negative for LCA. Finally, we diagnosed the patient as suffering with advanced gastric cancer, Borrmann type IV, stage II (T3N0M0) and we planned surgical resection. But patient refused surgical resection and chemotherapy on consolation and then he was discharged. Abdominal CT revealed decreased wall thickening of the body compare to that of 6 months ago. The perigastric infiltration had regressed (Fig. 3B). The histology showed no evidence of malignancy (Fig. 4D). We examed DNA test (DNA fingerprinting) using autosomal short tandem repeat to know whether the two biopsy specimens were from the same patient. And the result of DNA test revealed that the DNA of two specimens were identical. The patient is alive without any digestive symptoms 14 months after the follow up exam.
According to Everson's definition, spontaneous regression of malignant tumor is partial or complete disappearance of a malignant tumor in the absence of treatment that is ordinarily considered to be capable of producing regression. Further, the regression need not progress to complete disappearance of the tumor (4). This is very rare phenomenon. Of the 741 cases of spontaneous regression of malignant tumor from the year 1900 year to 1987, nine types of tumor (hypernephroma, malignant melanoma, neuroblastoma, retinoblastoma, leukemia, lymphoma, breast cancer, bladder cancer and choriocarcinoma) were noted in 511 cases (69%) and stomach cancer was noted in 17 cases (2.29%) (3). Regarding gastric cancer, 19 cases (5) of spontaneous regression have been reported.
Spontaneous regression of malignant tumor is very rare and its cause is mostly ambiguous, so it is very difficult to determine the scientific mechanism. Yet the mechanisms suggested till now are a hormonal or immunological mechanism, operative trauma, necrosis or vascular insufficiency, infection and a psychological mechanism (1, 3).
A hormonal mechanism was suggested because the onset of a pregnancy (6) or the cessation of ingestion of oral contraceptives was associated with the onset of a spontaneous regression of tumor (7, 8). In many cases of renal cell carcinoma, the remaining tumor mass regressed after the primary tumor or metastases had been surgically resected (9, 10), so we can presume that host immune system can destroy remaining tumor after the removal of the tumor burden (11). Other important mechanism is a febrile response associated with infection (12, 13). Of the patients with lung cancer, the 5-yr survival is increased in patients who are complicated with postoperative empyema (14). It was also reported that a patient with hepatocellular carcinoma developed severe cholangitis due to choledocholithiasis, and then hepatectomy was performed but the resected tumor demonstrated complete necrosis (15). In addition, some authors suggested a psychological factor (16) as the possible mechanism, but the evidence on this is still not clear.
At first, we suspected that the biopsy specimens could be mistaken. But, it was proven that the DNA of two specimens were identical according to the results of DNA fingerprinting. And the patient had no twin brother. So we could conclude that it was the spontaneous regression of advanced gastric cancer.
In this case, we could not identify any possible reason for the spontaneous regression of advanced gastric cancer. We herein report this very rare case, with a review of the related literature, in which advanced gastric cancer spontaneously regressed in 6 months without any clear cause.
Figures and Tables
Fig. 1
Initial EGD findings. (A) View of body from gastro-esophageal junction. (B) View of fundus and cardia from distal body. These showed a 10×5 cm sized diffuse edematous and erythematous mucosal change from the cardia just below the gastroesophageal junction to the lower body.
EGD, Esophagogastroduodenoscopy.
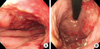
Fig. 2
EGD findings after 6 month. (A) View of body from gastro-esophageal junction. (B) View of fundus and cardia from distal body. This showed that normal mucosa was situated from the cardia just below gastro-esophageal junction to the lower body.
EGD, Esophagogastroduodenoscopy.

Fig. 3
Abdominal CT findings. (A) Initial abdominal CT findings. It showed diffuse irregular wall thickening and mucosal enhancement from the cardia to the lower body, perigstric infiltration and no evidence of lymph node enlargement or distant metastasis. (B) Abdominal CT findings after 6 months. It showed wall thickening of a decreased sized area limited to the lesser curvature side and the posterior wall side of the lower body in comparison with 6 months previously. The perigastric infiltration had regressed.
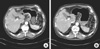
Fig. 4
Histopathologic findings. (A) The initial histopathologic findings. It showed many malignant cells with nuclear pleomorphism and plump eosinophilic cytoplasm at the lamina propria in the arrows (H&E stain, ×100). (B) The initial histopathologic findings with higher magnification. It also showed many malignant cells with large, irregular nucleus (H&E stain, ×200). (C) Immunohistochemical stain for cytokeratin AE1/AE3. It showed the malignant cells were positive for cytokeratin AE1/AE3 (×200). (D) The histopathologic findings after 6 months. It showed normal findings without any evidence of malignancy (H&E stain, ×40).
ACKNOWLEDGMENTS
We thank to Dr. Kyu Chan Hwang, Chief Director of Humanpass for his concern and support to the DNA test.
References
2. Jerry LM, Challis EB. Rakel RE, editor. Oncology. Textbook of family practice. 1984. 3rd ed. Philadelphia: WB Saunders;1061–1081.
3. Challis GB, Stam HJ. The spontaneous regression of cancer. A review of cases from 1900 to 1987. Acta Oncol. 1990. 29:545–550.

4. Everson TC, Cole WH. Spontaneous regression of cancer. 1966. Philadelphia: WB Saunders;1–10.
5. Sharma DN, Mohanti BK, Shukla NK, Rath GK. Spontaneous regression of carcinoma of the stomach. Clin Oncol (R Coll Radiol). 2000. 12:335–336.
6. Serati M, Uccella S, Laterza RM, Salvatore S, Beretta P, Riva C, Bolis PF. Natural history of cervical intraepithelial neoplasia during pregnancy. Acta Obstet Gynecol Scand. 2008. 87:1296–1300.

7. Steinbrecher UP, Lisbona R, Huang SN, Mishkin S. Complete regression of hepatocellular adenoma after withdrawal of oral contraceptives. Dig Dis Sci. 1981. 26:1045–1050.

8. Svrcek M, Jeannot E, Arrivé L, Poupon R, Fromont G, Fléjou JF, Zucman-Rossi J, Bouchard P, Wendum D. Regressive liver adenomatosis following androgenic progestin therapy withdrawal: a case report with a 10-year follow-up and a molecular analysis. Eur J Endocrinol. 2007. 156:617–621.

9. Wyczólkowski M, Klima W, Bieda W, Walas K. Spontaneous regression of hepatic metastases after nephrectomy and metastasectomy of renal cell carcinoma. Urol Int. 2001. 66:119–120.

10. Thoroddsen A, Gudbjartsson T, Geirsson G, Agnarsson BA, Magnusson K. Spontaneous regression of pleural metastases after nephrectomy for renal cell carcinoma. Scand J Urol Nephrol. 2002. 36:396–398.

11. Dunn GP, Old LJ, Schreiber RD. The immunobiology of cancer immunosurveillance and immunoediting. Immunity. 2004. 21:137–148.

12. Mitterbauer M, Fritzer-Szekeres M, Mitterbauer G, Simonitsch I, Knöbl P, Rintelen C, Schwarzinger I, Haas OA, Silberbauer K, Frey K, Bibus B, Pabinger I, Radaszkiewicz T, Lechner K, Jaeger U. Spontaneous remission of acute myeloid leukemia after infection and blood transfusion associated with hypergammaglobulinaemia. Ann Hematol. 1996. 73:189–193.

13. Lefrere F, Hermine O, Radford-Weiss I, Veil A, Picard F, Dreyfus F, Flandrin G, Varet B. A spontaneous remission of lymphoid blast crisis in chronic myelogenous leukaemia following blood transfusion and infection. Br J Haematol. 1994. 88:621–622.

14. Ruckdeschel JC, Codish SD, Stranahan A, McKneally MF. Postoperative empyema improves survival in lung cancer. Documentation and analysis of a natural experiment. N Engl J Med. 1972. 287:1013–1017.
15. Ohta H, Sakamoto Y, Ojima H, Yamada Y, Hibi T, Takahashi Y, Sano T, Shimada K, Kosuge T. Spontaneous regression of hepatocellular carcinoma with complete necrosis: case report. Abdom Imaging. 2005. 30:734–737.

16. Secheny S. Regression of cancer of the rectum after intensive meditation. Med J Aust. 1980. 1:136–137.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download