Abstract
We sought to determine the prevalence of metabolic syndrome (MS) in patients with acute myocardial infarction and its effect on clinical outcomes. Employing data from the Korea Acute Myocardial Infarction Registry, a total of 1,990 patients suffered from acute ST-elevation myocardial infarction (STEMI) between November 2005 and December 2006 were categorized according to the National Cholesterol Education Program-Adult Treatment Panel III criteria of MS. Primary study outcomes included major adverse cardiac events (MACE) during one-year follow-up. Patients were grouped based on existence of MS: group I: MS (n=1,182, 777 men, 62.8±12.3 yr); group II: Non-MS (n=808, 675 men, 64.2±13.1 yr). Group I showed lower left ventricular ejection fraction (LVEF) (P=0.005). There were no differences between two groups in the coronary angiographic findings except for multivessel involvement (P=0.01). The incidence of in-hospital death was higher in group I than in group II (P=0.047), but the rates of composite MACE during one-year clinical follow-up showed no significant differences. Multivariate analysis showed that low LVEF, old age, MS, low high density lipoprotein cholesterol and multivessel involvement were associated with high in-hospital death rate. In conclusion, MS is an important predictor for in-hospital death in patients with STEMI.
Metabolic syndrome (MS) is characterized by the clustering of risk factors related to insulin resistance (IR) and is associated with an increased risk of cardiovascular disease (1-5). In 2001, the National Cholesterol Education Program-Adult Treatment Panel (NCEP-ATP) III provided a new definition for MS, and this is based on simple clinical criteria and is considered as a prognostic indicator of vascular risk in patients with no overt coronary artery disease (1-4). Most recently, in 2005, American Heart Association/National Heart Lung and Blood Institute (AHA/NHLBI) presented new criteria modified from NCEP-ATP III criteria (6). Several studies based on populations at high risk for cardiovascular disease such as patients with hypertension or type 2 diabetes mellitus (DM) have shown a very high prevalence of MS from 35% to 80% (7, 8). In one cohort study, more than half of symptomatic patients who underwent elective coronary angiography and showed angiographic criteria for coronary artery disease, fulfilled the criteria for MS (9). Furthermore, a recent study in patients with established symptomatic vascular disease (e.g. coronary artery disease, stroke, or peripheral arterial disease) showed that the prevalence of MS correlated with the extent of vascular damage (10). Because scanty data are available on the prognostic role of MS in patients with acute myocardial infarction (MI) (11), authors attempted to assess the prevalence and clinical characteristics of MS, and to validate its association with cardiovascular events in acute ST-elevation MI (STEMI) patients.
The Korea Acute Myocardial Infarction Registry (KAMIR) is a prospective, multi-center, observational registry (CNUH IRB No. 05-0049) designed to examine current epidemiology, inhospital management, and outcome of patients with acute MI in Korea established for the commemoration of the 50th anniversary of the Korean Circulation Society (12, 13). Among the 7,780 patients with acute MI between November 2005 and October 2006, eligible 1,990 patients with acute STEMI were sorted by the diagnostic criteria of MS and followed up during 1 yr. Exclusion criteria were STEMI who could not be sorted by the diagnostic criteria of MS due to lack of data and non-STEMI. Total number of STEMI patients were 4,625 and the number of patients excluded were 2,635. These included patients were grouped based on existence of MS: Group I: The patients who were assigned to MS group, Group II: The patients who were assigned to non-MS group.
Patients were enrolled in the registry if they were admitted to participating hospitals with a suspected diagnosis of MI. A final diagnosis of MI was made in the presence of serial increases in serum biochemical markers of cardiac necrosis, associated with typical electrocardiographic changes and/or typical symptoms (14). Patients with ST-segment elevation ≥1 mm in ≥2 extremity electrocardiographic leads or ≥2 mm in ≥2 contiguous precordial leads or new left bundle branch block on the admission electrocardiogram were defined as having STEMI.
We analyzed baseline demographic and clinical characteristics, and relevant laboratory results. Creatinine clearance (CCr) was calculated using Cockroft and Gaut formula: CCr (mL/min)={[140-age (yr)]*weight (kg)}/[72*serum creatinine (mg/dL)] (multiply by 0.85 for women). Echocardiography was performed in all patients before discharge. The morphology of lesion in coronary angiography was classified by criteria of American College of Cardiology/American Heart Association (ACC/AHA) (15). The degree of coronary flow was classified by Thrombolysis In Myocardial Infarction (TIMI) score (16). Major adverse cardiac events (MACE) were evaluated at the 1 month, 6 months, and 1 yr clinical follow-up and were defined as the composite of 1) cardiac death, 2) non-cardiac death, 3) re-infarction, and 4) repercutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG). Re-infarction was defined as the recurrence of symptoms or electrocardiographic changes in association with a rise in cardiac enzymes above the upper limit of normal. All data were recorded on a standardized, electronic, web-based registry at http://www.kamir.or.kr.
For the diagnosis of MS at baseline, we used the NCEP-ATP III criteria. Merely, central obesity was defined as waist circumference >90 cm in men or >80 cm in women by modified ATP III guideline that WHO-Western Pacific Region (WPR) and International Association for the Study of Obesity (IASO) presented for Asian populations in 2000. The presence of MS was analyzed considering the presence of the following criteria: 1) Central obesity: waist circumference >90 cm (men), >80 cm (women) or body mass index (BMI) ≥25 kg/m2, 2) A fasting triglyceride level ≥150 mg/dL, 3) Reduced high density lipoprotein (HDL) cholesterol: <40 mg/dL (men), <50 mg/dL (women), 4) Hypertension: blood pressure ≥130/85 mmHg or taking antihypertensive medication, 5) Impaired fasting glucose (IFG): fasting glucose ≥110 mg/dL or taking medication or past history of type 2 DM. Patients were considered to have MS in the presence of ≥3 of criteria, according to the definition proposed by the AHA/NHLBI. Although AHA/NHLBI guideline recommended the definition of IFG is at or above 100 mg/dL, our study adopted NCEP-ATP III guideline (6).
We compared the in-hospital mortality, the admission duration of coronary care unit and the incidence of MACE during 1 month, 6 months, and 1 yr clinical follow-up between two groups.
The Statistical Package for Social Science (SPSS) for Windows, version 15.0 (Chicago, IL, USA) was used for all analysis. Continuous variables were expressed as mean±standard deviation (SD) and they were compared with the use of an unpaired Student's t-test. Categorial variables were compared with the use of the chi-square test, where appropriate. A P value less than 0.05 was deemed as significant. Adjusted odds ratios (OR) with accompanying 95% confidence intervals (CI) were reported. We used the risk ratio with 95% CI to evaluate the association between significant variables and adverse outcomes. A multiple logistic regression model was performed to examine the association between the MS and adverse clinical events.
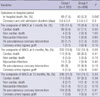
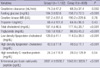
Among the 1,990 patients with acute STEMI who were followed up during one year, there were 1,182 patients with MS and 808 patients without MS. The baseline clinical characteristics and laboratory findings of the study population were described in Tables 1, 2. Patients of group I were younger (P=0.01) and more likely to be women (P<0.001) than those of group II. Also, they showed higher proportion of smoker (P<0.001), central obesity (P<0.001), hypertension (P<0.001) and DM (P<0.001). Group I showed lower left ventricular ejection fraction (LVEF) (P<0.001), but no significant difference in Killip class relative to group II (P=0.78). The levels of N-terminal pro-brain natriuretic peptide and CCr were higher in the group I than in the group II (P<0.001, P=0.002, respectively).
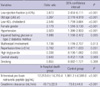
In the group I, coronary angiography was done in 94.1% of patients during hospitalization, and 92.2% in the group II. Also, PCI was done in 95.6% of patients in the group I relative to 95.3% in the group II; and success rate of PCI showed no significant difference between two groups. The baseline coronary angiographic characteristics are shown in Table 3. The most common infarct-related artery was the left anterior descending artery in both groups. A kind of infarct-related artery, lesion type according to ACC/AHA classification, and TIMI flow grade before and after PCI showed no significant differences between two groups. Multivessel involvement was more prevalent in the group I than in the group II (P=0.01).
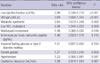
The clinical outcomes during one year follow-up are shown in Table 4. In-hospital mortality of total STEMI patients from KAMIR was 6.4% (n=296), and the estimated in-hospital mortality from present study was 7.5% in the group I and 5.2% in the group II (P=0.047). The duration of admission at the coronary care unit showed no significant difference between two groups. The incidence of composite MACE was not significantly different between two groups in 1 month, 6 months, and 12 months clinical follow-up.
Multivariate analysis was conducted to identify the independent predictors of in-hospital mortality with using the meaningful factors in univariate analysis (Table 5). The independent predictors of in-hospital mortality were found to be a low LVEF (P<0.001), old age (P<0.001), MS (P=0.002), low HDL-cholesterol level (P=0.003), and multivessel involvement (P=0.016) (Table 6).
Only a few studies have evaluated the prevalence of MS, as defined by the NCEP-ATP III criteria, in patients with symptomatic arterial disease. The results of previous studies suggested that MS was very common among patients with coronary artery disease, because almost a half of patients had MS and that it was associated with advanced vascular damage (9, 10). In contrast, recently, some experts have raised concerns about the clinical validity of MS (17, 18), and its clinical significance remained controversial. Our study, based on an unselected population of patients hospitalized with MI, confirmed the high prevalence of MS in patients with acute STEMI. More advanced vascular damage has been associated with the presence of MS in patients with manifest vascular disease, which may worsen the prognosis (10). MS represents a cluster of several risk factors, each of which may be involved in this poor outcome.
The main finding of present study was that the MS was meaningful predictor of in-hospital death in patients with STEMI. This result suggested that MS can be used for risk stratification in patients with STEMI. Among patients who have a history of acute MI, MS was recently shown to be associated with a higher rate of all-cause death and the composite of cardiovascular death, non-fatal stroke, and non-fatal MI (19). MS has also been shown to be associated with a higher incidence of severe heart failure following acute MI (20). In our study, MS was associated with increased risk of in-hospital mortality, but did not show the meaningful increment of poor long term clinical outcomes. Previous study showed that MS was a strong predictor of late-onset DM in post-MI and the risk of death among patients with MS was mainly associated with the transformation in DM (19). If more prolonged follow-up period is fulfilled, it would be possible that long-term outcome would be meaningfully increased in patient with MS relative to patient without MS. There are a number of reasons why MS could predispose to short-term mortality. Its components, such as central obesity, IR, dyslipidemia, hypertension, are all risk factors for endothelial dysfunction, which is an important factor in the pathophysiology of atherosclerosis and acute coronary syndromes. Hallmarks of the MS include a prothrombotic proinflammatory state and markers of inflammation have been found to correlate with the presence of MS in survivors of acute MI (2, 6, 21). Patients with impaired glucose tolerance found during admission for acute MI have an increased rate of non-fatal stroke, non-fatal MI, severe heart failure, and cardiovascular death (22).
The association between MS and poor prognosis highlights the clinical relevance of this syndrome, especially given the high prevalence among patients presenting with acute MI. Patients with MS should be identified and cared for appropriately, given the increased mortality noted in this study. Although there are currently no specific treatments directed at the MS as a whole, treating the individual components via lifestyle modification and lipid correcting agents have shown to slow the progression of MS and reduce the risk of cardiovascular disease (19, 23, 24).
This study has several limitations. First, our study is multi-center prospective registry, and it was not a randomized, controlled study. Thus there was probably a selection bias when enrolling patients into both study groups. Second, although we assessed risk factors at the time of the index event, we could not reliably measure how long the risk factors had been present before the MI. Third, using high BMI as a marker for truncal adiposity may not have accurately classified patients as having MS. However, BMI and waist circumference are strongly correlated, and high BMI has been shown to be strongly associated with MS (25-28). BMI has also been used as surrogate for waist circumference in other analysis, making it a reasonable choice to use in defining the MS group (19, 26). Finally, the period of our study is relatively short, because our study is a comparison of the MACE at one year clinical follow-up. Although there were such limitations in the present study, it should be emphasized that the presence of MS at the presentation of acue STEMI was associated with an increased short-term incidence of fatal events.
Conclusively, MS is highly prevalent in the patients with acute STEMI and have the detrimental impact on short term outcomes, so awareness and preventative measures are important in hopes of improving outcomes in these patients.
Figures and Tables
Table 4
Clinical outcomes and major adverse cardiac events during follow-up and at 12 months (after discharge)
ACKNOWLEDGMENTS
Korea Acute Myocardial Infarction Registry (KAMIR) Study Group of Korean Society of Cardiology, Jong Hyun Kim, M.D., Doo Il Kim, M.D., Bon Kwon Koo, M.D., Byung Ok Kim, M.D., Myoung Yong Lee, M.D., Kee Sik Kim, M.D., Jin Young Hwang, M.D., Seok Kyu Oh, M.D., Nae Hee Lee, M.D., Kyoung Tae Jeong, M.D., Seung Jea Tahk, M.D., Keum Soo Park, M.D., Kyoo Rok Han, M.D., Tae Hoon Ahn, M.D., Moo Hyun Kim, M.D., Ju Young Yang, M.D., Chong Yun Rhim, M.D., Hyeon Cheol Gwon, M.D., Seong Wook Park, M.D., Young Youp Koh, M.D., Seung Jae Joo, M.D., Soo Joong Kim, M.D., Dong Kyu Jin, M.D., Jin Man Cho, M.D., Byung Ok Kim, M.D., Sang-Wook Kim, M.D., Jeong Kyung Kim, M.D., Tae Ik Kim, M.D., Deug Young Nah, M.D., Si Hoon Park, M.D., Sang Hyun Lee, M.D., Seung Uk Lee, M.D., Hang-Jae Chung, M.D., Jang Hyun Cho, M.D., and Seung Won Jin, M.D.
References
1. Ferrannini E, Haffner SM, Mitchell BD, Stern MP. Hyperinsulinemia: the key feature of a cardiovascular and metabolic syndrome. Diabetologia. 1991. 34:416–422.
2. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002. 106:3143–3421.
3. Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, Salonen JT. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002. 288:2709–2716.

4. Sattar N, Gaw A, Scherbakova O, Ford I, O'Reilly DS, Haffner SM, Isles C, Macfarlane PW, Packard CJ, Cobbe SM, Shepherd J. Metabolic syndrome with and without C-reactive protein as a predictor of coronary heart disease and diabetes in the West of Scotland Coronary Prevention Study. Circulation. 2003. 108:414–419.

6. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC Jr, Spertus JA, Costa F. American Heart Association. National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation. 2005. 112:2735–2752.
7. Rantala AO, Kauma H, Lilja M, Savolainen MJ, Reunanen A, Kesaniemi YA. Prevalence of the metabolic syndrome in drug-treated hypertension patients and control subjects. J Intern Med. 1999. 245:163–174.
8. Isomaa B, Almgren P, Tuomi T, Forsén B, Lahti K, Nissén M, Taskinen MR, Groop L. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001. 24:683–689.

9. Solymoss BC, Bourassa MG, Campeau L, Sniderman A, Marcil M, Lésperance J, Lévesque S, Varga S. Effect of increasing metabolic syndrome score on atherosclerotic risk profile and coronary artery disease angiographic severity. Am J Cardiol. 2004. 93:159–164.

10. Olijhoek JK, van der Graaf Y, Banga JD, Algra A, Rabelink TJ, Visseren FL. SMART Study Group. The metabolic syndrome is associated with advanced vascular damage in patients with coronary heart disease, stroke, peripheral arterial disease or abdominal aortic aneurysm. Eur Heart J. 2004. 25:342–348.

11. Girman CJ, Rhodes T, Mercuri M, Pyörälä K, Kjekshus J, Pedersen TR, Beere PA, Gotto AM, Clearfield M. 4S Group and the AFCAPSTexCAPS Research Group. The metabolic syndrome and risk of major coronary events in the Scandinavian Simvastatin Survival Study (4S) and the Air ForceTexas Coronary Atherosclerosis Prevention Study (AFCAPSTex-CAPS). Am J Cardiol. 2004. 93:136–141.

12. Lee KH, Jeong MH, Ahn YK, Kim YJ, Chae SC, Hong TJ, Seong IW, Chae JK, Kim CJ, Cho MC, Seung KB, Park SJ. other Korea Acute Myocardial Infarction Registry Investigators. Gender differences of success rate of percutaneous coronary intervention and short term cardiac events in Korea Acute Myocardial Infarction Registry. Int J Cardiol. 2008. 130:227–234.

13. Sim DS, Jeong MH, Ahn YK, Kim YJ, Chae SC, Hong TJ, Seong IW, Chae JK, Kim CJ, Cho MC, Seung KB, Park SJ. Korea Acute Myocardial Infarction Registry (KAMIR) Investigators. Safety and benefit of early elective percutaneous coronary intervention after successful thrombolytic therapy for acute myocardial infarction. Am J Cardiol. 2009. 103:1333–1338.

14. French JK, White HD. Clinical implications of the new definition of myocardial infarction. Heart. 2004. 90:99–106.

15. Kini AS. Coronary angiography, lesion classification and severity assessment. Cardiol Clin. 2006. 24:153–162.

16. Manginas A, Gatzov P, Chasikidis C, Voudris V, Pavlides G, Cokkinos DV. Estimation of coronary flow reserve using the Thrombolysis In Myocardial Infarction (TIMI) frame count method. Am J Cardiol. 1999. 83:1562–1565.

17. Kahn R. Metabolic syndrome: is it a syndrome? Does it matter? Circulation. 2007. 115:1806–1811.
19. Levantesi G, Macchia A, Marfisi R, Franzosi MG, Maggioni AP, Nicolosi GL, Schweiger C, Tavazzi L, Tognoni G, Valagussa F, Marchioli R. GISSI-Prevenzione Investigators. Metabolic syndrome and risk of cardiovascular events after myocardial infarction. J Am Coll Cardiol. 2005. 46:277–283.

20. Zeller M, Steg PG, Ravisy J, Laurent Y, Janin-Manificat L, L'Huillier I, Beer JC, Oudot A, Rioufol G, Makki H, Farnier M, Rochette L, Vergès B, Cottin Y. Observatoire des Infarctus de Cote-d'Or Survey Working Group. Prevalence and impact of metabolic syndrome on hospital outcomes in acute myocardial infarction. Arch Intern Med. 2005. 165:1192–1198.
21. Yudkin JS, Juhan-Vague I, Hawe E, Humphries SE, di Minno G, Margaglione M, Tremoli E, Kooistra T, Morange PE, Lundman P, Mohamed-Ali V, Hamsten A. HIFMECH Study Group. Low grade inflammation may play a role in the etiology of the metabolic syndrome in patients with coronary heart disease: the HIFMECH study. Metabolism. 2004. 53:852–857.
22. Bartnik M, Malmberg K, Norhammar A, Tenerz A, Ohrvik J, Rydén L. Newly detected abnormal glucose tolerance: an important predictor of long-term outcome after myocardial infarction. Eur Heart J. 2004. 25:1990–1997.

23. Grundy SM, Hansen B, Smith SC Jr, Cleeman JI, Kahn RA. American Heart Association. National Heart, Lung, and Blood Institute. American Diabetes Association. Clinical management of metabolic syndrome: report of the American Heart Association/National Heart, Lung, and Blood Institute/American Diabetes Association conference on scientific issues related to management. Circulation. 2004. 109:551–556.
24. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM. Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002. 346:393–403.

25. Wannamethee SG, Shaper AG, Morris RW, Whincup PH. Measures of adiposity in the identification of metabolic abnormalities in elderly men. Am J Clin Nutr. 2005. 81:1313–1321.

26. Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, Allen K, Lopes M, Savoye M, Morrison J, Sherwin RS, Caprio S. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004. 350:2362–2374.

27. Lean ME, Han TS, Morrison CE. Waist circumference as a measure for indicating need for weight management. BMJ. 1995. 331:158–161.

28. Kip KE, Marroquin OC, Kelley DE, Johnson BD, Kelsey SF, Shaw LJ, Rogers WJ, Reis SE. Clinical importance of obesity versus the metabolic syndrome in cardiovascular risk in women: a report from the Women's Ischemia Syndrome Evaluation (WISE) Study. Circulation. 2004. 109:706–713.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download