Abstract
We developed a nomogram to predict the probability of extracapsular extension (ECE) in localized prostate cancer and to determine when the neurovascular bundle (NVB) may be spared. Total 1,471 Korean men who underwent radical prostatectomy for prostate cancer between 1995 and 2008 were included. We drew nonrandom samples of 1,031 for nomogram development, leaving 440 samples for nomogram validation. With multivariate logistic regression analyses, we made a nomogram to predicts the ECE probability at radical prostatectomy. Receiver operating characteristic (ROC) analyses were also performed to assess the predictive value of each variable alone and in combination. The internal validation was performed from 200 bootstrap re-samples and the external validation was also performed from the another cohort. Overall, 314 patients (30.5%) had ECE. Age, Prostate specific antigen (PSA), biopsy Gleason score, positive core ratio, and maximum percentage of biopsy tumor were independent predictors of the presence of ECE (all P values <0.05). The nomogram predicted ECE with good discrimination (an area under the ROC curve of 0.777). Our nomogram allows for the preoperative identification of patients with an ECE and may prove useful in selecting patients to receive nerve sparing radical prostatectomy.
While classic radical prostatectomy results in impotence and decreased quality of life, nerve sparing radical prostatectomy, which was introduced in 1983, is a milestone for improving treatment of clinically localized prostate cancer and maintaining adequate cancer control (1). However, methods to select the patients for nerve sparing radical prostatectomy are still controversial. To date, several selection criteria for nerve sparing radical prostatectomy have been investigated, including digital rectal examination, biopsy Gleason score, assessing surgical margins in the region of the neurovascular bundle (NVB) by intraoperative frozen sections or palpation (2, 3). These criteria are subjective and difficult to apply generally due to interclinician variability. Most widely used method of the selection is predicting extracapsular extension (ECE), because knowledge of the presence of ECE before treatment helps patients and physicians make better decisions (4). Therefore, much effort has been paid to the accurate preoperative prediction of the presence or the location of ECE. As results of efforts, pretreatment nomograms have been constructed on the basis of clinical stage, prostate specific antigen (PSA) level, and biopsy Gleason score. Nomograms are simple mathematical formulas or algorithms optimized for predictive accuracy. Such statistical models almost always perform better than any individual predictive factor and informed clinical judgment (5). Currently, several studies have tried to determine selection criteria for nerve-sparing radical prostatectomy based on biopsy-derived variables as well as the aforementioned factors (4, 6, 7).
Meanwhile, there are huge differences in incidence and aggressiveness of prostate cancer between Asian and Western countries (8-12). When compared with age-matched men in Western countries, Asian men have lower normal ranges of serum PSA and smaller prostate volumes (13-15). Moreover, almost all of the currently available data about the selection of patients for nerve sparing radical prostatectomy, especially about predicting the presence of ECE, were obtained from studies on Western populations. As a consequence, nomograms based on Asian data need to be established. Therefore, we developed a model predicting the probability of ECE in a multi-institutional cohort of Korean men by incorporating a detailed, quantitative assessment of biopsy results into a nomogram.
Nine hospitals of Korea participated in this retrospective multicenter study. Between January 1995 and December 2008, 1,582 consecutive patients who underwent radical retropubic prostatectomy for clinically localized prostate cancer without neoadjuvant therapy were evaluated. To optimize ECE data analysis, we excluded 111 patients who underwent bilateral nerve sparing surgery or unilateral nerve sparing including missing values since ECE status could not be determined precisely. We analysed nonrandom samples of 1,031 for nomogram development (e.g., according to center), leaving 440 for nomogram validation. Patient age, biopsy Gleason score, clinical stage, PSA, PSA density (PSAD), number of positive biopsy cores and maximum percentage of tumor in any core were analyzed preoperatively in each case. Prostate volume was measured by Transrectal ultrasound (TRUS) using the formula for elliptical volume (π/6*height*width*length). PSAD was evaluated as PSA (ng/mL) devided by TRUS-estimated prostate volume (mL).
All histological grading of biopsies and prostatectomy specimens were pathologically re-analyzed by nine uropathologists who are members of the Korean Genitourinary Pathology Study Group. In all cases the diagnosis was made by systemic biopsy (6 cores or more than 10 cores). The positive core ratio was calculated by dividing the number of positive cores by the number of cores taken at TRUS biopsy. The maximum percentage of tumor in any core was defined as the greatest tumor percent among the positive cores of biopsy. Each prostate was sectioned at 4-mm intervals in a transverse plane perpendicular to the posterior surface. Extracapsular extension was defined as tumor in contact with periprostatic soft tissue.
Continuous variables were compared using the Mann-Whitney test, whereas categorical variables were compared with chisquare test. The effect of preoperative variables on predicting overall likelihood of extracapsular extension was analyzed with multivariate logistic regression models (MLRM). The increment in predictive accuracy was determined for each variable and was quantified by receiver operating characteristic (ROC) analysis. Subsequently, MLRM coefficients were used to generate a nomogram predicting the probability of ECE at radical prostatectomy. Calibration was carried out for the constructed nomogram and internal validation was analyzed from 200 additional bootstrap samples to decrease the overfit bias. External validation was also performed in another cohort. All analyses were performed using SAS version 9.1 statistical software (SAS Institute, Cary, NC, USA) and R version 2.8.1 (The R Foundation for Statistical Computing, Vienna, Austria).
Preoperative characteristics of prostate cancer patients included in our study are listed in Table 1. Histopathologic evaluation of prostatectomy specimens revealed extracapsular extension in 314 (30.5%) of 1031 patients (Table 1). Of these 1,031 patients, 93 (9%) underwent TRUS-guided preoperative sextant biopsy, while 938 (91%) underwent extended biopsy (≧10 cores) schemes. The total number of biopsy cores ranged from 6 to 20. When comparing variables with and without ECE, all variables except BMI were significantly different as shown in Table 1 (P<0.001). Table 2 shows the multivariate regression analysis fitted in the development cohort. Age, PSA, biopsy Gleason score, positive core ratio and maximum percentage of tumor on biopsy were independent predictors of the presence of ECE (all P values <0.05). A multivariate logistic regression model (MLRM) and ROC curves for predicting ECE were constructed with preoperative variables. The predictive performances of MLRM and other individual variables were demonstrated by area under curve (AUC) (Fig. 1). After 200 bootstrap re-samples of the nomogram regression coefficients, the combined accuracy of the ECE prediction (AUC of MLRM) was 77.7% and exceeded the individual variables (Table 3). Fig. 2 shows the regression coefficient-based nomogram, which was devised from the predictor variables. Nomogram is used by first locating the patient position on each predictor variable scale. Each scale position has a corresponding prognostic points (top axis). The points for each variable are added and the probability of ECE is estimated from the bottom line with total points. The performance characteristics of the nomogram are shown in Fig. 3A, where the nomogram predicted probability of ECE is represented on the x-axis and the observed rate of ECE is plotted on the y-axis. Perfect prediction would correspond to a slope of 1 (diagonal 45-degree dashed line). The dotted line represents the apparent accuracy of this nomogram without correction for over fit. The solid line indicates bootstrap corrected nomogram performance. The external validation cohort data are represented by dotted line in Fig. 3B, where the solid line represents the logistic calibration of the model. The overall discrimination measurement of the validation cohort was 0.782.
With the increased detection of early stage prostate cancer, nerve sparing radical prostatectomy has become a matter of great concern. Although the selection criteria for nerve sparing radical prostatectomy have not been thoroughly determined at present, men with pathologically organ-confined cancer have been regarded as the best candidates for nerve sparing radical prostatectomy (7). Extracapsular extension of prostate cancer is closely connected to a potential risk for a positive surgical margin, which is important due to its adverse outcome for prostate cancer. Consequently, it is essential to know the existence of ECE preoperatively to preserve postoperative quality of life and to control the cancer.
Over the past few years, several studies have investigated the possibility of the presence or location of ECE using preoperative clinical and pathologic factors (7, 16, 17). Sebo et al. (18) studied 207 patients and found that the percent positive cores and percent cancer in systematic biopsies were the strongest predictors of extension beyond the prostate in a stepwise logistic regression analysis. More recently, several models predicting side-specific ECE have been also reported. Data from Naya et al. (17) also indicated that the maximum cancer length in positive cores is a significant risk factor of side-specific posterolateral ECE, independent of biopsy Gleason score. Ohori et al. (16) attempted to further improve the accuracy of the internally validated nomograms to predict the side specific probability of ECE based on sextant-based biopsy. Tsuzuki et al. (4) also reported a model predicting side-specific posterolateral ECE using PSA, finding of digital rectal examination, biopsy Gleason score, average percent of prostatic tissue involved with tumor and percent of positive core. However, in reality, most of the available reports on the selection of patients for nerve sparing radical prostatectomy, especially about predicting the presence of ECE, were based on data from Western populations. It is well known that geographical and ethnic differences in prostate cancer risk exist. A lower incidence of prostate cancer in Asian and Korean men than in European men has been reported (19). In addition, age-matched Korean men have lower normal serum PSA ranges, and their average total prostate volume is smaller than that of European men (13). In addition, prostate cancer screening in Korea is currently not as widespread as in Western countries, and prostate cancer in Korea is generally not detected as early as in Western countries. This situation may have contributed to the differences in cancer biology. Taken together, these differences may limit the usefulness of preexisting nomograms and has prompted efforts to develop a new model for a more accurate preoperative prediction of ECE which is suitable for Korean men.
In the current study, we focused only on the probability of presence of ECE, irrespective of location, and especially, the region of the neurovascular bundle (NVB). Our data showed that ECE was seen in 30% of all patients. The incidence of ECE in localized prostate cancer is consistent with that reported in recent studies (17, 20). Our nomogram included six variables: age, PSA, PSA density, biopsy Gleason score, biopsy positive core ratio and maximum percent of tumor in any core. Since the number of cores sampled varies among institutions, we chose the fraction of positive cores in reporting the number of cores, rather than the absolute number of positive cores. All of these predictors are relatively easy to collect clinically before surgery. Our nomogram seems to be simple and practical with a relatively high area under the ROC curve, thus exhibiting good performance. We quantified the gain in predictability on the basis of an increase in the area under the ROC curve. The AUC of our full model nomogram incorporating PSA, clinical stage, PSA density, biopsy Gleason score, percent positive cores and maximum percent of tumor in any core was 0.777. These findings support our selection of variables for determining suitable candidates for nerve sparing radical prostatectomy.
Our investigation has several distinctive features. First, our data regarding ECE were maximized because only non-nerve spared patients were evaluated. The ECE status could be evaluated precisely. Second, while most of published data on the prediction of actual ECE of prostate cancers before surgery have been based on patient cohorts who underwent prostate biopsy with a relatively limited number of cores, as in sextant biopsy, we mainly included men who underwent extended biopsy (≧10 cores). Only 93 (9%) patients underwent sextant biopsy. Third, although we did not present the data, our nomogram was applicable to low risk (biopsy GS ≦7) and high risk (biopsy GS ≧8) group. Fourth, the descriptive cancer statistics presented in this study provide representative data that illustrate the characteristics of prostate cancer in Korean men. Moreover, the pathologic slides were re-evaluated by 9 uropathologists who had fully discussed the pathological assessment criteria including biopsy Gleason grading to improve interobserver reproducibility in our study. We believe that our nomograms will assist physicians in counseling Korean men as well as Asian men with prostate cancer regarding the probability of the presence of ECE.
The potential limitations of this study should be considered. The internal validation was calculated by 200 additional bootstrapping samples to decrease the overfit bias. Although bootstrapping has been shown to represent the best alternative to external validation (21) and external validation was performed with subpopulation group, our accuracy results were not validated in different population and may still be affected by residual overfit bias. Another limitation is that we could not assess the site-specific ECE in the NVB region nor confirm the identification of the biopsy positive site and ECE site of prostatectomy specimens since many of our cases were from outside institutions where this information was not available. Therefore, our study provides no information about the location of the ECE. However, it had been reported that the majority of ECE occurs at the posterolateral border of the prostate. Villers et al. (22) showed that capsular penetration of cancerous tissue is often present at the neurovascular bundle. Others have indicated that the most common location of extracapsular extension in palpable tumors is posterolateral, near the neurovascular bundle (23-25). Hence this nomograms derived from our site-nonspecific risk of ECE can be helpful in selecting patients suited for nerve sparing or non-nerve sparing prostatectomy. In this study, we did not use specific cutoff values for the respective variables, because the nomograms were not designed to be used with a specific cutoff. Despite these limitations, this model may offer an effective tool with which to select men who are suitable candidates for nerve sparing radical prostatectomy in the era of extended biopsy schemes.
In conclusion, we constructed a nomogram to predict the probability of extracapsular extension in prostate cancer based on the data of age, serum PSA levels, prostate volume and systematic biopsy results. In an era when less aggressive surgical treatments are being encouraged for localized prostate cancer, our model represents an important contribution and may assist patients and physicians in making surgical decisions.
Figures and Tables
Fig. 1
Receiver operating characteristics (ROC) curve of multivariate logistic regression model (MLRM) for predicting extracapsular extension (ECE) in prostate cancer.
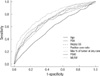
Fig. 2
Nomogram for predicting ECE in localized prostate cancer. Find the position of each variable on the corresponding axis, draw a line to the 'points' axis for the number of points, add the points from all the variables together and draw a line from the 'total points' axis to determine the extracapsular extension probabilities at the bottom.

Fig. 3
(A) Calibration curves of preoperative nomogram in internal validation cohort. The x-axis is the predicted probability from the nomogram, and the y-axis is the actual probability of ECE. The dashed line represents performance of the ideal nomogram (predicted outcome perfectly corresponds with actual outcome). The dotted line represents the apparent accuracy of our nomogram without correction for over fit. The solid line represents bootstrap-corrected performance of our nomogram. (B) Calibration plot of nomogram in external validation cohort (n=440). Solid line indicates logistic calibration curve and dotted line represent data for validation cohort.

ACKNOWLEDGMENTS
The authors express their thanks to Korean Uropathology Society for providing pathological support.
References
1. Walsh PC, Lepor H, Eggleston JC. Radical prostatectomy with preservation of sexual function: anatomical and pathological considerations. Prostate. 1983. 4:473–485.

2. Goharderakhshan RZ, Sudilovsky D, Carroll LA, Grossfeld GD, Marn R, Carroll PR. Utility of intraoperative frozen section analysis of surgical margins in region of neurovascular bundles at radical prostatectomy. Urology. 2002. 59:709–714.

3. Hernandez DJ, Epstein JI, Trock BJ, Tsuzuki T, Carter HB, Walsh PC. Radical retropubic prostatectomy. How often do experienced surgeons have positive surgical margins when there is extraprostatic extension in the region of the neurovascular bundle? J Urol. 2005. 173:446–449.

4. Tsuzuki T, Hernandez DJ, Aydin H, Trock B, Walsh PC, Epstein JI. Prediction of extraprostatic extension in the neurovascular bundle based on prostate needle biopsy pathology, serum prostate specific antigen and digital rectal examination. J Urol. 2005. 173:450–453.

5. Kattan MW, Eastham JA, Stapleton AM, Wheeler TM, Scardino PT. A preoperative nomogram for disease recurrence following radical prostatectomy for prostate cancer. J Natl Cancer Inst. 1998. 90:766–771.

6. Taneja SS, Penson DF, Epelbaum A, Handler T, Lepor H. Does site specific labeling of sextant biopsy cores predict the site of extracapsular extension in radical prostatectomy surgical specimen. J Urol. 1999. 162:1352–1357.

7. Graefen M, Haese A, Pichlmeier U, Hammerer PG, Noldus J, Butz K, Erbersdobler A, Henke RP, Michl U, Fernandez S, Huland H. A validated strategy for side specific prediction of organ confined prostate cancer: a tool to select for nerve sparing radical prostatectomy. J Urol. 2001. 165:857–863.

8. Wu AH, Whittemore AS, Kolonel LN, John EM, Gallagher RP, West DW, Hankin J, Teh CZ, Dreon DM, Paffenbarger RS Jr. Serum androgens and sex hormone-binding globulins in relation to lifestyle factors in older African-American, white, and Asian men in the United States and Canada. Cancer Epidemiol Biomarkers Prev. 1995. 4:735–741.
9. Lee SE, Kwak C, Park MS, Lee CH, Kang W, Oh SJ. Ethnic differences in the age-related distribution of serum prostate-specific antigen values: a study in a healthy Korean male population. Urology. 2000. 56:1007–1010.

10. Robbins AS, Koppie TM, Gomez SL, Parikh-Patel A, Mills PK. Differences in prognostic factors and survival among white and Asian men with prostate cancer, California, 1995-2004. Cancer. 2007. 110:1255–1263.

11. Song C, Kang T, Ro JY, Lee MS, Kim CS, Ahn H. Nomograms for the prediction of pathologic stage of clinically localized prostate cancer in Korean men. J Korean Med Sci. 2005. 20:262–266.

12. Jung KW, Won YJ, Park S, Kong HJ, Sung J, Shin HR, Park EC, Lee JS. Cancer statistics in Korea: Incidence, Mortality and Survival in 2005. J Korean Med Sci. 2009. 24:995–1003.

13. Ku JH, Ahn JO, Lee CH, Lee NK, Park YH, Byun SS, Kwak C, Lee SE. Distribution of serum prostate-specific antigen in healthy Korean men: influence of ethnicity. Urology. 2002. 60:475–479.

14. Chang YL, Lin AT, Chen KK, Chang YH, Wu HH, Kuo JY, Huang WJ, Lu SH, Hsu YS, Chung HJ, Chang SC. Correlation between serum prostate specific antigen and prostate volume in Taiwanese men with biopsy proven benign prostatic hyperplasia. J Urol. 2006. 176:196–199.

15. Gupta A, Aragaki C, Gotoh M, Masumori N, Ohshima S, Tsukamoto T, Roehrborn CG. Relationship between prostate specific antigen and indexes of prostate volume in Japanese men. J Urol. 2005. 173:503–506.

16. Ohori M, Kattan MW, Koh H, Maru N, Slawin KM, Shariat S, Muramoto M, Reuter VE, Wheeler TM, Scardino PT. Predicting the presence and side of extracapsular extension: a nomogram for staging prostate cancer. J Urol. 2004. 171:1844–1849.

17. Naya Y, Slaton JW, Troncoso P, Okihara K, Babaian RJ. Tumor length and location of cancer on biopsy predict for side specific extraprostatic cancer extension. J Urol. 2004. 171:1093–1097.

18. Sebo TJ, Bock BJ, Cheville JC, Lohse C, Wollan P, Zincke H. The percent of cores positive for cancer in prostate needle biopsy specimens is strongly predictive of tumor stage and volume at radical prostatectomy. J Urol. 2000. 163:174–178.

19. Robbins AS, Koppie TM, Gomez SL, Parikh-Patel A, Mills PK. Differences in prognostic factors and survival among white and Asian men with prostate cancer, California, 1995-2004. Cancer. 2007. 110:1255–1263.

20. Ward JF, Zincke H, Bergstralh EJ, Slezak JM, Myers RP, Blute ML. The impact of surgical approach (nerve bundle preservation versus wide local excision) on surgical margins and biochemical recurrence following radical prostatectomy. J Urol. 2004. 172:1328–1332.

21. Steyerberg EW, Harrell FE Jr, Borsboom GJ, Eijkemans MJ, Vergouwe Y, Habbema JD. Internal validation of predictive models: efficiency of some procedures for logistic regression analysis. J Clin Epidemiol. 2001. 54:774–781.
22. Villers A, McNeal JE, Redwine EA, Freiha FS, Stamey TA. The role of perineural space invasion in the local spread of prostatic adenocarcinoma. J Urol. 1989. 142:763–768.

23. Rosen MA, Goldstone L, Lapin S, Wheeler T, Scardino PT. Frequency and location of extracapsular extension and positive surgical margins in radical prostatectomy specimens. J Urol. 1992. 148:331–337.
24. Hall GS, Kramer CE, Epstein JI. Evaluation of radical prostatectomy specimens. A comparative analysis of sampling methods. Am J Surg Pathol. 1992. 16:315–324.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download