Abstract
Hyperbilirubinemia is frequently observed in Caucasian HIV patients treated with atazanavir. UDP-glucuronosyltransferase 1A1 polymorphism, UGT1A1*28, which is associated with atazanavir-induced hyperbilirubinemia, is less common in Asians than in Caucasians. However, little is known about the incidence of atazanavir-associated hyperbilirubinemia in Asian populations. Our objective was to investigate the incidence of and tolerability of atazanavir-associated hyperbilirubinemia in Korean HIV patients. The prevalence and cumulative incidence of atazanavir-associated hyperbilirubinemia and UGT1A1*28 allele frequency was investigated in 190 Korean HIV-infected patients treated with atazanavir 400 mg per day. The UGT1A1*28 were examined by direct sequencing of DNA from peripheral whole blood. The UGT1A1*28 allele frequency was 11%. The cumulative incidence of any grade of hyperbilirubinemia was 77%, 89%, 98%, and 100%, at 3, 12, 24, and 30 months, respectively. The cumulative incidence of severe (grade 3-4) hyperbilirubinemia was 21%, 41%, 66%, and 75%, at 3, 12, 24, and 30 months, respectively. However, the point prevalence of severe hyperbilirubinemia did not increase with time and remained around 25%. Our data suggest that atazanavir-associated hyperbilirubinemia is common but transient in a population with low UGT1A1*28 allele frequency.
Atazanavir is an HIV protease inhibitor with several advantages including once-daily dosing, low pill burden, and a favorable effect on lipid profile compared with other protease inhibitors (1, 2). Unconjugated hyperbilirubinemia is the major laboratory abnormality associated with use of atazanavir (3). Although atazanavir-associated hyperbilirubinemia is not associated with hepatic injury (3), it may be a hurdle in actual clinical practice because it can cause cosmetic concerns (1).
Atazanavir induces hyperbilirubinemia by competitive inhibition of the microsomal enzyme UDP-glucuronosyltransferase (UGT) 1A1, which is responsible for bilirubin conjugation (4, 5). Promoter containing seven thymine adenine (TA) nucleotide repeats, A(TA)7TAA (the UGT1A1*28 allele), is less active than the common promoter containing 6 TA repeats (6). Homozygosity for the UGT1A1*28 allele is strongly associated with the risk of developing hyperbilirubinemia while receiving atazanavir (5, 7).
The frequency of the UGT1A1*28 allele differs between racial groups. Its frequency is much lower in Asians including Japanese (11%), Chinese (16%), and Koreans (13%), than in other racial groups such as African Americans (43%), Caucasians (36-39%), and Indians (35%) (8-11). Therefore, the incidence of clinically significant hyperbilirubinemia associated with atazanavir might be expected to be lower in Asians than in other racial groups. However, previous studies of atazanavir-associated hyperbilirubinemia were based on Caucasians, Hispanic, and African populations, and to our knowledge, there has been no report focusing on Asian populations. Hence, in this study, we investigated the incidence and tolerability of atazanavir-associated hyperbilirubinemia in Korean HIV patients.
All the HIV-infected patients who initiated antiretroviral therapy with atazanavir (400 mg per day) from May 2005 to April 2007 were identified from the electronic database of Seoul National University Hospital (SNUH). Patients with active liver disease were excluded. Total bilirubin levels and HIV viral titers in blood were measured every 3 months after initiating atazanavir. Subjects who did not discontinue atazanavir were followed up until April 2008. Antiretroviral therapy regimen was managed by the board certified infectious disease specialist.
Atazanavir-associated hyperbilirubinemia was defined as a hyperbilirubinemia developing after initiation of atazanavir therapy in the absence of other cause of hyperbilirubinemia. Hyperbilirubinemia was classified in accordance with the AIDS Clinical Trials Group guidelines for total bilirubin levels: grade 1, 23-32 µM/L (1.3-1.9 mg/dL); grade 2, 33-53 µM/L (1.9-3.1 mg/dL); grade 3, 54-105 µM/L (3.1-6.1 mg/dL); and grade 4, >105 µM/L (>6.1 mg/dL) (12). Viral suppression was defined as <40 copies/mL. Active liver disease was defined as an elevation of hepatic transaminase to more than 2 times the upper limit of normal.
The recognition of TA repetitions at the UGT1A1 promoter gene was assessed by direct sequencing of DNA extracted from peripheral whole blood, using previously reported primers and PCR conditions (4).
Continuous variables are expressed as median and interquartile range (IQR) values. The confidence intervals of the occurrence rates of hyperbilirubinemia were estimated from Poisson distribution 95% confidence limits. Proportions were compared using the chi-square test. Statistical analyses were performed with SPSS software (version 17.0; SPSS Inc., Chicago, IL, USA).
One hundred and ninety HIV-infected patients were included in this study. Total follow-up duration was 3,511 person-months, and median duration of atazanavir treatment was 17 months (IQR, 12-27 months).
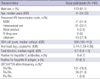
All were Koreans, and 173 (91.1%) of the patients were male. The median age was 41 yr (IQR, 34-53 yr). The median CD4 cell count at the beginning of atazanavir therapy was 258 cells/µL (IQR, 160-413 cells/µL), and 61 (32.1%) patients were antiretroviral naïve patients. Atazanavir containing regimen accounted for 34.3% of initial combination regimens for the antiretroviral-naïve patients during the study period. Antiretroviral drugs that were administered concurrently with atazanavir included zidovudine/lamivudine (n=146, 76.8%), stavudine+lamivudine (n=24, 12.6%), abacavir+lamivudine (n=12, 6.3%), didanosine+lamivudine (n=7, 3.7%), and zidovudine+didanosine (n=1, 0.5%). The genetic study was performed in 168 (88.4%) of these patients and the distribution of UGT1A1 genotypes was as follows: TA6/TA6 in 78.0%, TA6/TA7 in 21.4%, and TA7/TA7 in 0.6% (Table 1).
The data on total bilirubin levels was available in 1,143 (97.7%) of 1,170 bilirubin measurements which were expected during 3,511 person-months follow-up period. The cumulative incidence of hyperbilirubinemia of any grade was 76.8% (95% confidence interval [CI], 70.1-82.4) at 3 months, 89.3% (95% CI, 83.3-93.4) at 12 months, 98.6% (95% CI; 91.9-100) at 24 months, and 100% (95% CI, 90.9-100) at 30 months. The cumulative incidence of grade 3-4 hyperbilirubinemia was 21.4% (95% CI, 16.0-28.1) at 3 months, 41.3% (95% CI; 33.8-49.3) at 12 months, 64.4% (95% CI, 52.9-74.4) at 24 months, and 74.5% (95% CI, 57.0-84.0) at 30 months. Although the cumulative incidence of grade 3-4 hyperbilirubinemia increased consistently with time, the prevalence of grade 3-4 hyperbilirubinemia at specific time points remained around 25% (Fig. 1). There was no significant difference in prevalence of hyperbilirubinemia between total patients and those with viral suppression at each time point (P=0.57).
In the 91 patients who experienced grade 3-4 hyperbilirubinemia during the study period, the median time from atazanavir initiation to detection of grade 3-4 hyperbilirubinemia was 6 months (range 1-27 months). Grade 3-4 hyperbilirubinemia developed more than 3 months after atazanavir initiation in 53 (58.2%) patients, and more than 1 yr in 17 (18.7%) patients. Of the latter 17 patients, 15 (88.2%) maintained the viral suppressed state before the development of grade 3-4 hyperbilirubinemia.
Among the 40 patients who were followed up to 30 months, 29 (72.5%) developed grade 3-4 hyperbilirubinemia. Of these, grade 3-4 hyperbilirubinemia was persistent during the study period in only one (3.4%), while it was transient in the other 28 (96.6%) patients.
Of the 190 patients, 54 (28.4%) discontinued atazanavir therapy during the study period. The most common reason for discontinuation was loss to follow-up (18 patients; 9.5%), followed by viral resistance to atazanavir (14 patients; 7.4%), and cosmetic problem due to hyperbilirubinemia (11 patients; 5.8%). Atazanavir therapy was discontinued in eight (21.1%) of 38 patients in whom grade 3-4 hyperbilirubinemia developed within 16 weeks after initiating atazanavir, and in three (5.7%) of 53 patients in whom it developed after 16 weeks (P=0.034).
Koreans have a lower frequency of the UGT1A1*28 allele (9-10), which is significantly associated with grade 3-4 hyperbilirubinemia in patients taking atazanavir (5). It might be supposed therefore that the incidence of atazanavir-associated hyperbilirubinemia would be lower in Koreans than in Caucasians. However, contrary to this expectation, the incidence of grade 3-4 hyperbilirubinemia in Korean HIV patients with long-term atazanavir use was similar or even higher than in Caucasians. Among our patients who had taken atazanavir for more than 12 months, 41.3% developed grade 3-4 hyperbilirubinemia. After 24 months of atazanavir treatment, 64.4% of patients experienced grade 3-4 hyperbilirubinemia. The present study showed higher incidences of grade 3-4 hyperbilirubinemia than those reported in the clinical trials using an unboosted atazanavir regimen in Caucasian patients (3, 13). The incidences at 12 months and 24 months were equal to those reported in the clinical trials using boosted atazanavir regimen (14, 15).
In previous studies on Caucasians, bilirubin elevation was detected within the 12-16 weeks of treatment initiation in majority of subjects with grade 3-4 hyperbilirubinemia (3, 7, 13-15). However, in the present study, the median duration from atazanavir initiation to detection of grade 3-4 hyperbilirubinemia was 6 months. Although in patients with delayed-onset hyperbilirubinemia, drug adherence might influence onset of hyperbilirubinemia, its effect was supposed to be minimal because most the patients in this study achieved complete viral suppression.
The clinical course of grade 3-4 hyperbilirubinemia also differed from the results of previous studies in Caucasians. In the studies in Caucasian, grade 3-4 hyperbilirubinemia persisted throughout the atazanavir treatment (3, 13-15). However, in our study, grade 3-4 hyperbilirubinemia was transient in spite of continued atazanavir treatment. This was compatible with the findings that although the cumulative incidence of grade 3-4 hyperbilirubinemia increased steadily over the observed periods, the cross-sectional prevalence of grade 3-4 hyperbilirubinemia remained around 25%.
Although atazanavir-associated hyperbilirubinemia is not associated with hepatic injury, it may lead to cosmetic concerns that result in discontinuation of atazanavir (1). In the clinical trials, the cosmetic concerns appeared to be well tolerated by subjects and led to treatment discontinuation in less than 1% (3, 13-15). In the present study, 11 (5.8%) patients discontinued atazanavir therapy because of jaundice. Interestingly, hyperbilirubinemia detected after 16 weeks was better tolerated than hyperbilirubinemia before 16 weeks, in part because delayed-onset hyperbilirubinemia was generally transient.
There are some limitations to the present study. First, factors other than atazanavir could have affected bilirubin metabolism. To reduce the effect of possible confounders, we excluded patients with active liver disease, which might influence bilirubin metabolism. Second, when investigating the point prevalence of hyperbilirubinemia, patients who discontinued atazanavir were excluded; therefore our prevalence data might have underestimated the actual prevalence of hyperbilirubinemia.
In summary, more than two-thirds of Korean patients who received atazanavir for two years experienced grade 3-4 hyperbilirubinemia in actual clinical practice. This suggests that severe atazanavir-associated hyperbilirubinemia is frequent in Asian population with low UGT1A1*28 prevalence. A further study to find out the genetic factors other than UGT1A1*28 for atazanavir-associated hyperbilirubinemia in Asians is warranted.
Figures and Tables
Notes
References
1. Havlir DV, O'Marro SD. Atazanavir: new option for treatment of HIV infection. Clin Infect Dis. 2004. 38:1599–1604.

2. Choi H, Jeong SJ, Lee HS, Chin BS, Choi SH, Han SH, Kim MS, Kim CO, Choi JY, Song YG, Kim JM. Two cases of multidrug-resistant human immunodeficiency virus infection treated with atazanavir and lopinavir/ritonavir combination therapy. J Korean Med Sci. 2008. 23:737–739.

3. Squires K, Lazzarin A, Gatell JM, Powderly WG, Pokrovskiy V, Delfraissy JF, Jemsek J, Rivero A, Rozenbaum W, Schrader S, Sension M, Vibhagool A, Thiry A, Giordano M. Comparison of once-daily atazanavir with efavirenz, each in combination with fixed-dose zidovudine and lamivudine, as initial therapy for patients infected with HIV. J Acquir Immune Defic Syndr. 2004. 36:1011–1019.

4. Zucker SD, Qin X, Rouster SD, Yu F, Green RM, Keshavan P, Feinberg J, Sherman KE. Mechanism of indinavir-induced hyperbilirubinemia. Proc Natl Acad Sci USA. 2001. 98:12671–12676.

5. Rotger M, Taffe P, Bleiber G, Gunthard HF, Furrer H, Vernazza P, Drechsler H, Bernasconi E, Rickenbach M, Telenti A. Gilbert syndrome and the development of antiretroviral therapy-associated hyperbilirubinemia. J Infect Dis. 2005. 192:1381–1386.

6. Bosma PJ, Chowdhury JR, Bakker C, Gantla S, de Boer A, Oostra BA, Lindhout D, Tytgat GN, Jansen PL, Oude Elferink RP, Chowdhury NR. The genetic basis of the reduced expression of bilirubin UDP-glucuronosyltransferase 1 in Gilbert's syndrome. N Engl J Med. 1995. 333:1171–1175.

7. Rodriguez-Novoa S, Martin-Carbonero L, Barreiro P, Gonzalez-Pardo G, Jimenez-Nacher I, Gonzalez-Lahoz J, Soriano V. Genetic factors influencing atazanavir plasma concentrations and the risk of severe hyperbilirubinemia. AIDS. 2007. 21:41–46.
8. Beutler E, Gelbart T, Demina A. Racial variability in the UDP-glucuronosyltransferase 1 (UGT1A1) promoter: a balanced polymorphism for regulation of bilirubin metabolism? Proc Natl Acad Sci USA. 1998. 95:8170–8174.

9. Ki CS, Lee KA, Lee SY, Kim HJ, Cho SS, Park JH, Cho S, Sohn KM, Kim JW. Haplotype structure of the UDP-glucuronosyltransferase 1A1 (UGT1A1) gene and its relationship to serum total bilirubin concentration in a male Korean population. Clin Chem. 2003. 49:2078–2081.

10. Kim JO, Shin JY, Lee MA, Chae HS, Lee CH, Roh JS, Jin SK, Kang TS, Choi JR, Kang JH. Genetic polymorphisms of UGT1A and their association with clinical factors in healthy Koreans. Genomics Inform. 2007. 5:161–167.
11. Takeuchi K, Kobayashi Y, Tamaki S, Ishihara T, Maruo Y, Araki J, Mifuji R, Itani T, Kuroda M, Sato H, Kaito M, Adachi Y. Genetic polymorphisms of bilirubin uridine diphosphate-glucuronosyltransferase gene in Japanese patients with Crigler-Najjar syndrome or Gilbert's syndrome as well as in healthy Japanese subjects. J Gastroenterol Hepatol. 2004. 19:1023–1028.

12. Fellay J, Boubaker K, Ledergerber B, Bernasconi E, Furrer H, Battegay M, Hirschel B, Vernazza P, Francioli P, Greub G, Flepp M, Telenti A. Swiss HIV Cohort Study. Prevalence of adverse events associated with potent antiretroviral treatment: Swiss HIV Cohort Study. Lancet. 2001. 358:1322–1327.

13. Wood R, Phanuphak P, Cahn P, Pokrovskiy V, Rozenbaum W, Pantaleo G, Sension M, Murphy R, Mancini M, Kelleher T, Giordano M. Long-term efficacy and safety of atazanavir with stavudine and lamivudine in patients previously treated with nelfinavir or atazanavir. J Acquir Immune Defic Syndr. 2004. 36:684–692.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download